Translate this page into:
Dermoscopy of Zoon balanitis

*Corresponding author: Arun Somasundaram, Department of Dermatology, Venereology and Leprology, JIPMER, Puducherry, India. arunsomasundaram25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramar S, Ramamoorthy L, Somasundaram A. Dermoscopy of Zoon balanitis. CosmoDerma 2023;3:158.
A 50-year-old male presented with an asymptomatic skin lesion over the glans. There is no history of itching, burning, or oozing. These lesions had been present for the past 6 months. Genital examination revealed a single well-circumscribed shiny orange-red moist slightly raised plaque over the glans penis with multiple bright red speckled spots, “cayenne pepper spots” seen in the background were noted [Figure 1a and b]. Dermoscopy showed a reddish-orange structureless area and curved vessels [Figure 2]. Based on the clinical examination and the characteristic dermoscopy findings, Zoon balanitis was diagnosed.

- (a and b) Single well-circumscribed shiny orangered moist slightly raised plaque over the glans penis with multiple bright red speckled spots, “cayenne pepper spots.”
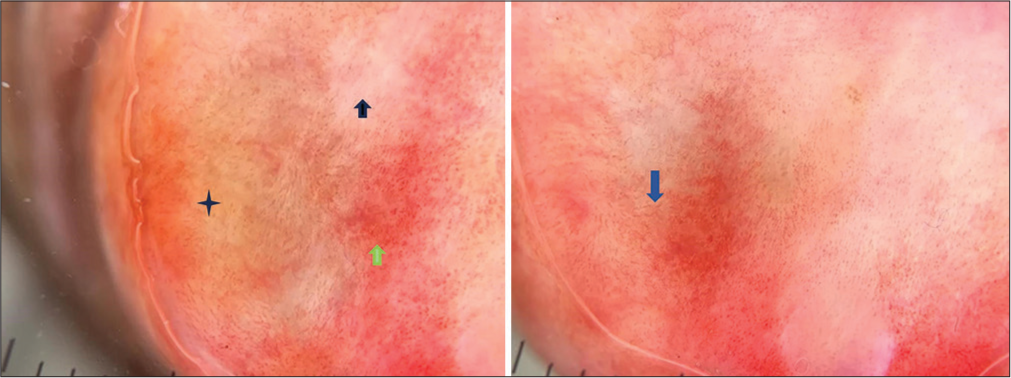
- Reddish-orange structureless (black asterix), curved vessels (green arrow), yellow-white areas (black arrows), and serpentine vessels (blue arrows).
Zoon balanitis/plasma cell balanitis of Zoon is an idiopathic chronic benign inflammatory mucositis of genitalia. It presents as a single well-defined, orange-red, shiny, moist macule to slightly raised plaque, with multiple pinpoint bleeding spots resembling cayenne pepper spots.[1] Dermoscopy of the lesion demonstrates the presence of focal reddish-orange structureless areas [Figure 2] corresponding to the combination of underlying vascular dilation, red cell extravasation, and hemosiderin deposition in the dermis in histology. The curved vessels, serpentine in orientation [Figure 2], correspond to the vascular proliferation and overlying epidermal atrophy. Yellow-white areas represent areas of dermal fibrosis, indicating a chronic nature of the lesion.[2] Given the presence of distinct dermoscopic features, it can add as a rapid tool in the diagnosis of Zoon balanitis. The sterility was maintained by placing an ice cap on the contact surface of the dermoscope. It can be particularly beneficial in averting the need for invasive procedures like biopsy, as such procedures can add to the anxiety of the patient, especially given the sensitive area involved.
Declaration of patient consent
Patient’s consent was not required as patients identity was not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Zoon balanitis: A comprehensive review. Indian J Sex Transm Dis AIDS. 2016;37:129-38.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic characterization of Zoon balanitis: First case series from Asia. Indian Dermatol Online J. 2022;13:86-9.
- [CrossRef] [PubMed] [Google Scholar]





