Translate this page into:
Resolution of Zoon’s balanitis following topical mupirocin application: A case report

-
Received: ,
Accepted: ,
How to cite this article: Narayanan A, Balasundaram MK, Thappa DM. Resolution of Zoon’s balanitis following topical mupirocin application: A case report. CosmoDerma 2022;2:40.
Dear Sir,
Zoon’s balanitis is an idiopathic condition affecting the glans penis. It is also known as balanitis circumscripta plasmacellularis or plasma cell balanitis. We report a case of Zoon’s balanitis with good improvement following topical mupirocin application.
A 32-year-old male patient presented with well-defined, erythematous, moist patches as kissing lesions involving the areas of glans penis and the inner surface of prepuce on either side of the coronal sulcus [Figure 1a] for the past six months. He experienced an occasional burning sensation over the lesion. There was no regional lymphadenopathy, phimosis, or paraphimosis present. There were no lesions elsewhere on the body suggestive of lichen planus or psoriasis. Side lab investigations, including tzanck smear, potassium hydroxide mount, and gram stain, didn’t reveal any abnormality. Dermoscopic examination (DermLite DL200 Hybrid, non-contact dermoscopy, polarized, ×10 magnification) of the lesion under revealed a focal orange-yellow structureless area with dilated linear-irregular and serpentine vessels [Figures 1c and 1d]. Few dotted vessels and chalice-shaped vessels were seen occasionally. Based on the clinical and dermoscopic features, a diagnosis of Zoon’s balanitis was made. The patient was treated with twice daily application of topical mupirocin 2% ointment and asked to review after a week. However, the patient came for review after 1 month. He had continued the application of mupirocin since he noticed he had significant improvement in the lesion [Figure 1b].
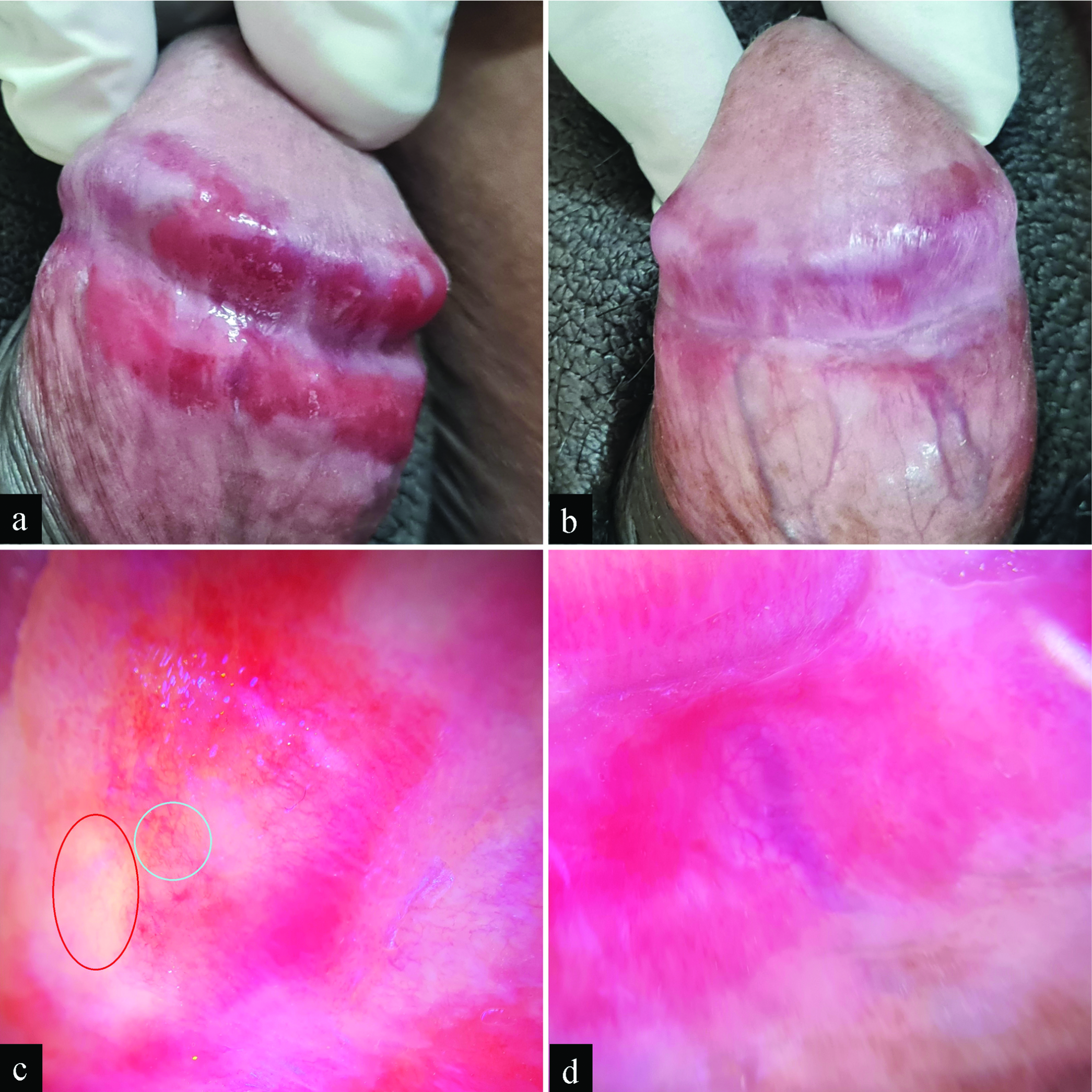
- (a) Well-defined, erythematous, moist patches in the form of kissing lesions involving the areas ofglans penis and the inner surface of prepuce on either side of the coronal sulcus with (b) significant improvement in the lesion following topical mupirocin 2% ointment application for 1 month. Dermoscopy of the (c) glans penis and (d) inner surface of prepuce revealed a few orange-yellow structureless areas (red circle) with dilated linear-irregular and serpentine vessels (blue circle). (DermLite DL200 Hybrid, non-contact dermoscopy, polarized, ×10 magnification)
Zoon’s balanitis classically presents in uncircumcised middle-aged men. It presents as a well-demarcated, moist, glistening, erythematous lesion with a “cayenne pepper” speckled. While the lesions are commonly observed over the glans penis, they can also involve the inner surface of the prepuce or coronal sulcus. Kissing lesions may also be seen. Zoon’s balanitis is usually asymptomatic. However, few patients may develop pruritus or tenderness.
Histopathological examination typically reveals a dense lichenoid infiltrate with a predominance of plasma cells. In addition, “lozenge-shaped” keratinocytes, vascular proliferation, hemosiderin deposition, and erythrocyte extravasation may be seen. Dermoscopic examination reveals focal/diffuse orange-yellowish structureless areas with vascular dilatation/proliferation. The vessels may be curved, serpentine, convoluted, or chalice-shaped. In addition, linear-irregular vessels, dotted vessels, or spermatozoa-like vessels may be seen. The epidermal thinning seen in Zoon’s balanitis makes the dermal vessels appear sharper and brighter.
Educating the patient regarding genital hygiene is an easy and beneficial action. Patients might also require counseling and reassurance regarding their cosmetic appearance. Circumcision will almost always cure the disease. Traditionally, potent topical corticosteroids or topical calcineurin inhibitors were used to provide symptomatic relief to the patient. Petersen et al. demonstrated suppression or cure of Zoon’s balanitis following treatment with 2% fusidic acid cream.[1] Chessa et al. demonstrated improvement in Zoon’s balanitis following treatment with betamethasone plus fusidic acid combination cream.[2] Lee et al.[3] and Bari et al.[4] observed improvements in Zoon’s balanitis following treatment with topical mupirocin ointment. There was a significant improvement in these lesions within 2 weeks of treatment with topical mupirocin.[5] Our patient also noticed significant improvement with mupirocin, which resulted in the continuation of the treatment on his own.
Erythematous lesions in the glans penis and prepuce might require a histopathological examination to make a diagnosis. However, many patients are not comfortable with the mucosal biopsy procedure in the genitalia. There is a prompt response to mupirocin in patients with Zoon’s balanitis. Dermatologists may consider a therapeutic trial with topical 2% mupirocin ointment before proceeding to a biopsy when Zoon’s balanitis is being considered. This would establish the diagnosis and simultaneously treat the condition.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
Author Devinder Mohan Thappa is the Editor-In-Chief of the journal.
References
- Fusidic acid cream in the treatment of plasma cell balanitis. J Am Acad Dermatol. 1992;27:633-4.
- [CrossRef] [PubMed] [Google Scholar]
- Zoon’s plasma cell balanitis: Clinical and dermoscopic features in pediatric patients. Int J Dermatol. 2018;57:e142-4.
- [CrossRef] [PubMed] [Google Scholar]
- Zoon balanitis revisited: Report of balanitis circumscripta plasmacellularis resolving with topical mupirocin ointment monotherapy. J Drugs Dermatol. 2017;16:285-7.
- [PubMed] [Google Scholar]
- Successful management of Zoon’s balanitis with topical mupirocin ointment: A case report and literature review of mupirocin-responsive balanitis circumscripta plasmacellularis. Dermatol Ther (Heidelb). 2017;7:203-10.
- [CrossRef] [PubMed] [Google Scholar]
- Topical mupirocin 2% ointment for diagnosis of Zoon’s balanitis and monotherapy of balanitis circumscripta plasmacellularis. Int J Dermatol. 2019;58:e114-5.
- [CrossRef] [PubMed] [Google Scholar]





