Translate this page into:
Guidelines based management of androgenetic alopecia

*Corresponding author: Ravi Kumar Chittoria, Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. drchittoria@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Chittoria RV, Reddy JB. Guidelines based management of androgenetica alopecia. CosmoDerma. 2023;4:1. doi: 10.25259/CSDM_177_2023
Abstract
Androgenetic alopecia as the name suggests androgenetic hair loss is the most common type of hair loss disorder that affects men and women. Androgenetic hair loss usually starts during puberty followed by a gradual progression of hair loss. The incidence of androgenetic hair loss increases with age affecting up to 80% of men and 42% of women. Patients with androgenetic alopecia can have a significant impact on their quality of life. A systematic literature review was conducted to evaluate the effectiveness of current treatment options. The therapist’s recommendations were endorsed by consensus conferences. The aim of this guideline is to give plastic surgeons an evidence-based tool to select an effective and safe remedy.
Keywords
Alopecia
Guidelines
Management
INTRODUCTION
Although Orentreich coined the term “Androgenetic alopecia (AGA)” in 1960, the same male condition has also been referred to as “male pattern alopecia,” “male alopecia,” “male pattern hair loss,” or “male pattern hair loss or MPHL,”[1] [Figure 1]. Androgen dependence and heredity factors are less apparent in affected women than men, so pattern hair loss, a more general term, is preferable for women. AGA is the most common hair loss that occurs in both men and women after puberty. Asian men with AGA have distinct characteristics compared to men from other ethnicities. Asian patients with AGA show more apical hair loss and less frontal hair loss compared to Caucasians. The prevalence increases with age equally in all Asian groups studied. The reason for the higher prevalence of Asian patients with AGA compared to Caucasians remains unknown.

- Patient with alopecia.
There are not many published guidelines available right now for Asian individuals with AGA. Japanese guidelines were released not too long ago. The prevalence, type, family history, and other characteristics of Asians differ from those of other races, so recommendations for the treatment of AGA must be developed. This is because there is little data comparing the reactions of different races to different AGA treatments.[2,3]
MATERIAL AND METHODS
This review was carried out in a South Indian tertiary care hospital’s plastic surgery department. A number of public resources, including Google and the Internet, were searched for the literature. Before writing the rules in our paper, existing guidelines were examined.
RESULTS
Previously published guidelines based on pre-existing classifications of AGA cannot easily classify the patterns of AGA that are more frequently seen in Asians. The BASP classification not only facilitates the development of a unified and simplified algorithm but also overcomes the disadvantages of previously reported classification systems.
DISCUSSION
Different classification schemes have been put out to characterize AGA. Beek published a classification system in 1950 that used frontal and frontal baldness, two factors of development, and was based on 1000 Caucasian men. Hamilton developed a systematic AGA classification the very following year. Based on frontoparietal and frontal receding and terminal thinning,[4] Hamilton categorized baldness patterns [Figure 2]. He then examined a sizable population of men and women to determine whether any particular pattern of hair loss existed from birth to age ten. Hamilton’s classification was improved in 1975 by Norwood,[5] who focused primarily on the temporal, frontal, and vertex subclasses. Among 1000 adult Caucasian men of varying ages, seven distinct forms of hair loss including variation A and male pattern baldness, were observed.[2,6]

- Hamilton Norwood classification of alopecia.
Ludwig Classification to describe female pattern hair loss.
Type I is minimal thinning that can be camouflaged with hair styling techniques.
Type II is characterized by decreased volume and noticeable widening of the midline part.
Type III describes diffuse thinning with a see-through appearance on the top of the scalp.
Recently, a number of reviews on AGA have been published along with recommendations for diagnosis and treatment. The pathophysiology, consequences, and medication lists of AGA are the main topics of several published reviews.[7,8] Furthermore, it should be emphasized that whereas previously published standards are applicable to Caucasians, their applicability to Asians is limited. Regrettably, there are currently insufficient clinical trials comparing Asians and Caucasians with AGA.[3] To compare the clinical symptoms of Asians and Caucasians, more research is required. These factors make it crucial to create gender-neutral and acceptable guidelines for the management of AGA for Asians.
The basic and specific classification (BASP) classification, on which this guide is based, not only makes the process of developing a unified and simplified algorithm easier, but it also gets rid of the drawbacks of previously published classification methods [Figure 3]. Physician involvement and education in the diagnosis and treatment of Asian patients’ AGA is crucial. The more prevalent AGA patterns among Asians are difficult to classify using previously published recommendations based on current AGA categories.[8] Of course, other races, regardless of age or gender, can also use this new rule, not just Asian people. In addition to assisting medical professionals in managing and selecting suitable therapies for patients with AGA, this guideline will dispel myths and provide false information to the general population.
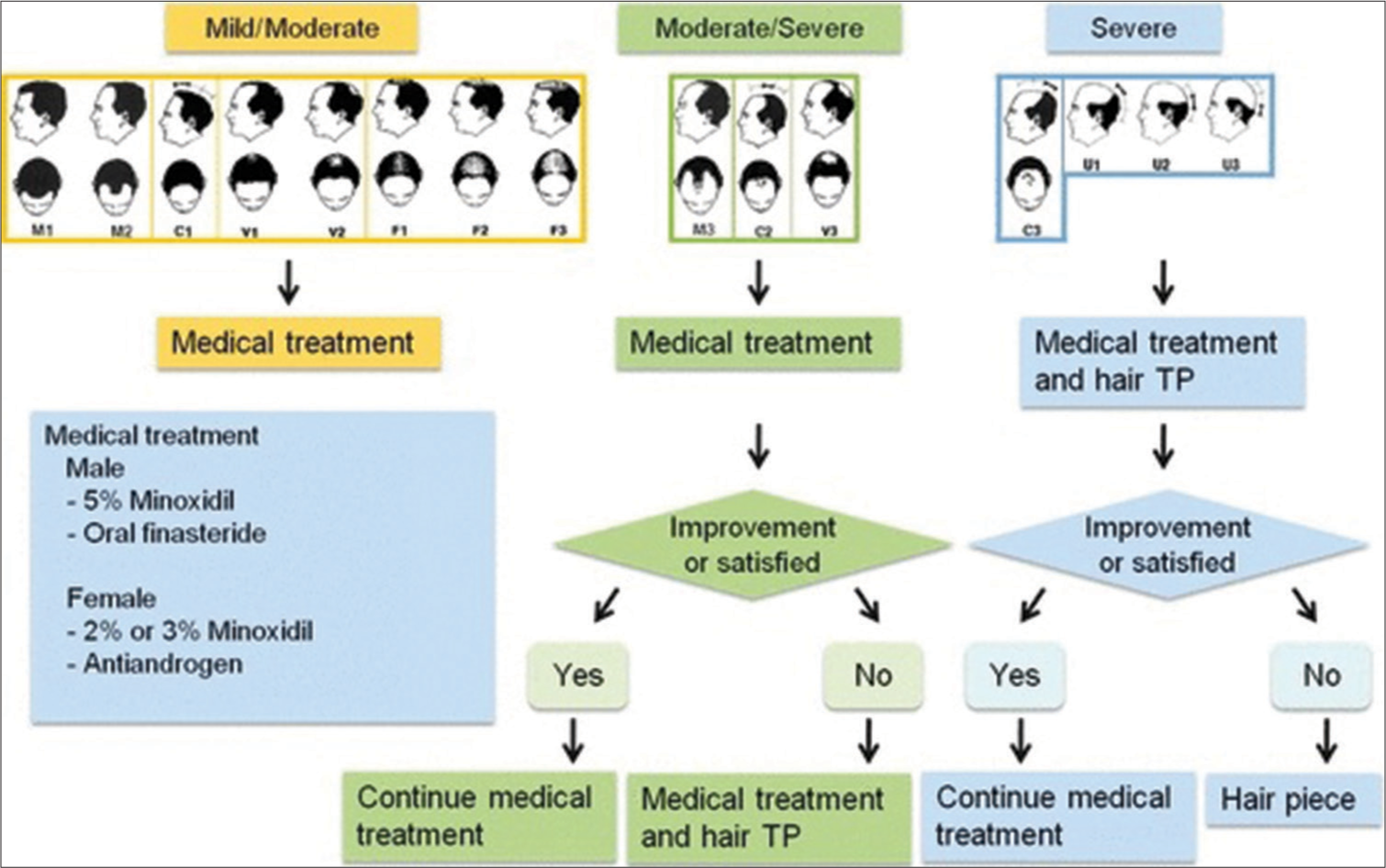
- Algorithmic guideline for the management of androgenetic alopecia (AGA). Mild/moderate androgenetic = BASP type M1-2, C1, F1-3 or V1-2; moderate/severe AGA = BASP type M3, C2-3, U1-3 or V3; severe AGA = BASP type C3 or U1-3.
MANAGEMENT
General considerations
Patients should avoid hair care products that can damage the scalp and/or hair. Patients should also maintain a proper diet, especially a diet with adequate protein. The National Institutes of Health recommended daily consumption of protein is 0.8 g/kg.
Treatment
There are several treatment methods [Table 1].
| Males |
| Topical minoxidil |
| Oral finasteride |
| Females |
| Topical minoxidil |
| Oral anti-androgens |
| Surgical treatment |
| Hair transplantation |
| Miscellaneous medical therapy |
| Oral dutasteride |
| Topical 0.025% alfatradiol |
| Evolving therapy |
| Bimatoprost and latanoprost |
| Ketoconazole |
| Non-medical aesthetic aids |
| Wigs, hair pieces, and hair extensions |
| Topical powder makeup |
Topical minoxidil solution
Ten milliliter is applied twice a day to the affected area. Regardless of the source, the elongation of the anagen phase and hair shaft diameter appears to be the primary advantage; its mode of action is uncertain. A 5% minoxidil solution might work better than a 2% or 3% one. The creation of a 5% topical foam is a recent advancement in the use of minoxidil to treat hair loss. Patients find the foam to be safe, effective, and esthetically pleasing.
Oral minoxidil (OM)
Male- and female-patterned hair loss (MPHL and FPHL) are two hair disorders that can be safely and effectively treated with low-dose OM.[9] Enhanced cosmesis, financial savings, and the ability to cotreat with different topical formulations or topicals used for camouflage are just a few of the practical benefits of OM over its topical counterpart. Patients who cannot tolerate topical minoxidil or other systemic therapies may benefit most from this course of treatment. For FPHL, daily doses of 0.25–1.25 mg and for MPHL, daily doses of 2.5–5 mg are typically used.[10] Minoxidil has the potential to trigger the release of β-catenin signaling pathway and vascular endothelial growth factors (VEGF). β-catenin is involved in the regeneration of hair follicles (HFs) and functions as a transcriptional factor. Adverse effects include pleural effusion, electrocardiogram abnormalities, fluid retention, abrupt pulmonary edema, and pulmonary hypertension at high doses used for hypertension.[11] Reflex tachycardia is the most common cardiac issue linked to the medicine. Pericardial effusion and congestive heart failure in people with advanced renal impairment are less common side effects.
Oral finasteride
A daily dose of 1 mg of oral finasteride, a strong type II 5-alpha-reductase inhibitor, should be given. The majority of the time, finasteride is well tolerated, has moderate side effects, and does not normally need to be stopped. Erectile dysfunction and decreased libido are uncommon side effects. Finasteride and dutasteride are inhibitors of the enzyme 5-alpha-reductase, which inhibits the conversion of testosterone to dihydrotestosterone (DHT). Dutasteride inhibits both type I and type II 5-alpha-reductase while finasteride inhibits only the type II enzyme. As both isoenzymes are present in HFs, it is likely that dutasteride is more effective than finasteride.[12]
Oral antiandrogens
Flutamide, spironolactone, and cyproterone acetate can be used in place of minoxidil solution; however, most antiandrogen therapies have not been thoroughly examined in FPHL patients. Generally speaking, women who have hyperandrogenism experience better outcomes.[13,14] The side effects of spironolactone and cyproterone acetate are typically more severe. Some minor studies have looked into the efficacy of antiandrogens in AGA, although this strategy is typically not taken into account.
Microneedling
It involves the use of a skin roller with small needles that cause minor skin injuries. Aside from collagen production in the skin, which is thought to underlie one of the reasons, it may be beneficial for alopecia, it is thought that microneedling can also help induce stem cells in the HFs that may lead to hair growth. Microneedling may also promote the absorption of products used to treat your hair loss, such as minoxidil, topical steroid, and platelet-rich plasma. Microneedling itself may cause bruising, oozing from the wounds, redness, swelling, and pain.[15]
Cyclic nutritional therapy
Strengthening the hair roots, giving the cells a non-toxic environment, and encouraging hair development are scientifically more advantageous than addressing possible but unproven reasons for hair loss. Vitamins, minerals, and dietary supplements that support well-being, good health, and hair growth can help strengthen hair and encourage growth. The primary cause of hair loss is the scalp’s natural hair roots, which gradually deteriorate. By fortifying these roots, additional hair loss can be stopped. This would, in a sense, lessen hair loss every cycle. DHT production can be stopped by antioxidants. We anticipate a more natural alternative answer due to the hair care program’s long-term practical use. Hair follicle metabolism and cell turnover are correlated with the functions of the intestinal epithelium and bone marrow, thus multiple nutrients including antioxidants, amino acids, vitamins, minerals, and fatty acids are necessary for hair growth.[13] It has been noted in nutrient study that taking many supplements concurrently can affect how well they are absorbed and function together. Iron and calcium can chelate one another when taken together, which decreases absorption.[14] Frequent iron consumption can result in mucosal obstructions to iron absorption, and iron excess can undergo the Fenton reaction and turn into a prooxidant.[16,17] Cell apoptosis can be brought on by an excess of calcium in the cell.[18] Increased blood levels of vitamin C are not a guarantee from a high intake. Antioxidants that are consumed in excess counteract these advantages and become pro-oxidants. To optimize the positive effects of dietary supplements and reduce the negative effects of supplement interactions, efficient cyclic nutritional therapy has been devised.
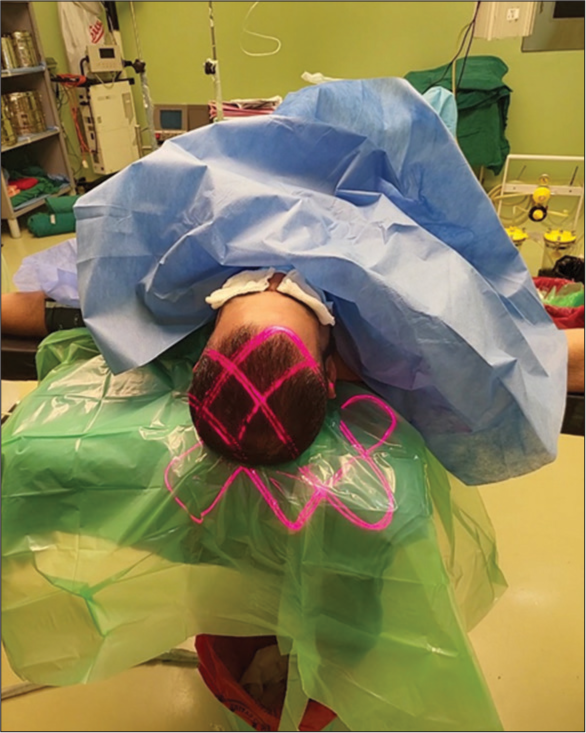
Surgical management
In cases of severe AGA, hair transplantation continues to be the only permanent hair restoration option, despite advancements in medical care. Patients with systemic conditions such as diabetes mellitus, hypertension, and heart disease, should not get hair transplantation unless these conditions are under control. Before hair transplantation, local conditions such as scalp folliculitis, morphea, cutaneous lupus erythematosus, and hair loss must be completely resolved for a minimum of six months. Ingrown hairs and foreign body reactions, infection, cobblestones, graft paralysis, epidermal cysts, bleeding, headaches, scarring (keloid and hypertrophic scars), poor hair growth, arteriovenous fistula, osteomyelitis, wound dehiscence, telogen effluvium, and alopecia are among the complications associated with hair transplantation. The conversion of androstenedione to estrone and the conversion of testosterone to 17-b-estradiol were both boosted when 0.025% alfatradiol with 17-estradiol (alpha-estradiol) was applied topically to promote hair growth. Although there are conflicting results on the efficacy of topical alfatradiol in Caucasian trials, it might be a viable choice. In a recent Asian study conducted in Korea, hair volume and diameter after four and eight months following therapy significantly improved when treated with 17α-estradiol solution compared to baseline. In studies, dutasteride showed a noticeably higher level of efficacy.
Follicular unit extraction (FUE)
FUE hair transplantation uses a different extraction technique than follicular unit transplantation (FUT), but the implantation process is the same. This sutureless hair restoration technique involves using tiny micropunches to remove HFs from the back of the head under local anesthesia, then implanting them in the bald spot. There have been several developments in the realm of FUE; a quick summary of them is provided here.
Follicular isolation technique (FIT)
Bansod et al.[19] first used the term “follicular isolation technique” to describe an FUE technique that limits the depth of penetration with a punch that has a “stop.” If the unit is not being collected in its entirety, FIT may be a more appropriate name than FUE, even though the necessity of a depth stop in the extraction procedure remains a controversial matter. We believe that the name FIT is more appropriate when the objective is simply hair extraction rather than intact follicular units.
Automated FUE hair transplantation
An automated hair transplant device called the FUE Matic aims to help the physician carry out a FUE hair transplant procedure.[20,21] It is said to provide a quicker rate of graft extraction in a constrained amount of time. Grafts are being pulled and twisted more, which increases the chance of injury and increases transection.
Robotics in hair transplantation
Apart from their obvious advantages, robots often enhance and increase human capabilities.[21] They could be able to repeat and obtain sub-millimeter accuracy. Robots can be designed to complete tasks that call for a high level of precision rapidly, independently, and consistently, which will increase productivity and efficiency. Regarding performance, their production is dependable and steady. They might be suitable for several hair transplantation procedures, including FUE, due to their technological benefits. Using robots has drawbacks, including expense, lack of adaptability, inability to handle qualitative data, and lack of judgment. These hair transplant robotics are under development, and it is expected that the people will soon have access to them.
Advantages of FUE include
Quicker healing time.
Less pain after surgery.
Does not cause a significant scar.
Hair from other body parts can be used.
Can be used even if you have poor hair density.
Disadvantages include
FUE follicular units are harvested from a much wide donor area than in traditional micrografting.
Graft quality is lower than in traditional micrografting.
Maximum yield is lower than in traditional micrografting. Grafts of lower quality do not grow as well.
At each transplant session, new scarring occurs.
The number of grafts in a single session is limited.
FUE is generally more expensive than traditional micrografting.
FUT
In FUT (sometimes also known as the “strip method”) a long, thin piece of tissue is removed from the back of the scalp. Individual follicular units are then removed from the strip using stereomicroscopic dissection.
Advantages of FUT include
Maybe a better option if you need a large number of HFs grafted.
Shorter operation time.
Cheaper surgery.
Disadvantages include
The procedure involves risk of scarring and a longer recovery period per treatment session, as it is invasive.
Leaves a linear scar at the site where the donor strip is excised.
It can result in stretching of the scalp.
The scars can become large sized and localized, which make them slightly more visible.
The same FUE procedure is used for body hair transplant (BHT) and hence, there is no stitching involved. The reason it is termed BHT is that this technique uses another body part as the donor place for hair rather than the back of the scalp. It can affect the arms, legs, stomach region, back, chest, and beard. Grafts are harvested from any of these bodily parts and then placed over the balding portion of the head.
Only those with extreme baldness, very little reserve or extremely thin hair in the rear of their scalp are candidates for BHT. Thus, even people with severe (type VI and VII) hair loss have a great deal of hope, thanks to this procedure. Although BHT yields are not as high as those from traditional scalp transplants, body hair remains a good source of donor HFs for hirsute people in need of hair restoration. In the transplanted area, beard hair has great optical density and is the easiest to harvest. In addition, body hair can be used to disguise scars from past surgeries or medical conditions and soften hairlines.[21]
Low-level laser therapy
Low-level laser treatment (LLLT) is the use of low-intensity light to stimulate tissue cellular activity. It is connected to a spectrum of laser light that supports tissue regeneration and repair, ranging from red to infrared.[22] We refer to the entire physiological effect of LLLT as photobiomodulation [Figure 4]. It is thought to lengthen the anagen phase, promote anagen phase re-entry in telogen HFs, and boost rates of proliferation in anagen HFs that are active in the anagen phase.[23] Furthermore, it aids in the promotion of physiological regeneration, which takes place during the hair cycle and is strongly dependent on cell proliferation as well as reparative regeneration, which happens during wound healing [Figure 5].
The hair-stimulating effect of fractional photothermolysis laser treatment depended on the energy level, frequency, and irradiation interval. A pilot study in humans showed a gradual improvement in hair density and growth rate in both Asians and Caucasians.
- Low-level laser therapy.

- After treatment with low-level laser therapy, autologous platelet-rich plasma therapy.
Growth factor concentrate (GFC) treatment
To provide better natural results, GFC therapy or GFC treatment uses a concentrated growth factor formulation made from the candidate’s blood cells that are extremely safe and devoted. Blood platelets include a variety of growth factors that aid in tissue regeneration and repair as well as stem cell migration, proliferation, and differentiation. Consequently, the role that each GFC plays in combating hair loss varies [Figure 6].

- Autologous platelet-rich plasma therapy.
Platelet-derived growth factor: This growth factor promotes angiogenesis and vascularization while also aiding in the growth of hair. In addition, it aids in the proliferation and chemotaxis of fibroblasts as well as the mitogenesis of endothelium and mesenchymal stem cells.
VEGF: During the anagen phase of hair, hair follicle dermal papilla cells express VEGF, which controls perifollicular angiogenesis in the hair. To facilitate the process, it also enlarges the perifollicular vessels during the anagen growth phase.
Epidermal growth factor (EGF): EGF increases mesenchymal and epithelial cell mitogenesis and encourages hair cell proliferation and regeneration. In addition, it also costimulates angiogenesis.
Insulin-like growth factor-1 (IGF-1): IGF-1 functions as an angiogenesis stimulant, preserves HF growth, and enhances total hair growth.
Algorithmic guideline for the management of AGA
Figure 6 suggested a strategy for the therapeutic management of AGA, and lists a number of AGA therapies. For mild-to-moderate AGA, first follow-up visits should occur 6 and 12 months with men receiving BASP-type finasteride and women receiving 2% or 3% minoxidil or antiandrogens for 6 to 12 months. It is necessary to take a pretreatment photo to track the patient’s progress.
Patients with AGA (BASP type M3, C2 or V3) are advised to get treatment for a minimum of one year. Drug therapy along with hair transplantation is advised for those who do not observe stabilization or improvement after a year of treatment. It is advised to combine medication therapy and hair transplantation for a minimum of one year in patients with severe AGA (BASP type C3 or U1-3). Hair extensions or cosmetic augmentation may be explored for people with severe AGA, who do not show significant improvement or stabilization after a year of treatment. This algorithmic guideline can also be used for Caucasians, although the committee developed it specifically for Asians because the classification used in the BASP guidelines properly classifies the more common AGA patterns.
CONCLUSION
Despite the fact that the clinical features of AGA are widely known in both genders, there is still much to learn about the best course of treatment given the genetics and pathophysiology of these prevalent illnesses. The psychological health of AGA patients must also be taken into account by the cosmetic surgeon since this could result in the wrong course of therapy. For certain men and women with AGA, there are currently effective medication or surgical treatments available. Asian individuals with AGA have a distinct family history and history of hair loss than other ethnic groups, which could affect how well they respond to treatment. Therefore, the Asian AGA’s treatment recommendations may be helpful for the region’s plastic surgeons. There is a need to develop an AGA treatment guideline based on the BASP classification for Asians, who may have a different presentation of AGA compared to other races. However, this new guideline is not limited to Asian patients and can be universally applied to everyone regardless of race or gender.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Male-pattern hair loss in Norwegian men: A community-based study. Dermatology. 2000;200:219-22.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical and biological guide for understanding chemotherapy-induced alopecia and its prevention. Oncologist. 2018;23:84-96.
- [CrossRef] [PubMed] [Google Scholar]
- Patterned loss of hair in man; types and incidence. Ann N Y Acad Sci. 1951;53:708-28.
- [CrossRef] [PubMed] [Google Scholar]
- Male pattern baldness: Classification and incidence. South Med J. 1975;68:1359-65.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of male pattern hair loss in 18-49 year old men. Dermatol Surg. 1998;24:1330-2.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative damage control in a human (mini-) Organ: Nrf2 activation protects against oxidative stress-induced hair growth inhibition. J Invest Dermatol. 2017;137:295-304.
- [CrossRef] [PubMed] [Google Scholar]
- Investigative guidelines for alopecia areata. Dermatol Ther. 2011;24:311-9.
- [CrossRef] [PubMed] [Google Scholar]
- Oral minoxidil treatment for hair loss: A review of efficacy and safety. J Am Acad Dermatol. 2021;84:737-46.
- [CrossRef] [PubMed] [Google Scholar]
- Safety of low-dose oral minoxidil treatment for hair loss. A systematic review and pooled-analysis of individual patient data. Dermatol Ther. 2020;33:e14106.
- [CrossRef] [Google Scholar]
- Superiority of dutasteride over finasteride in hair regrowth and reversal of miniaturization in men with androgenetic alopecia: A randomized controlled open-label, evaluator-blinded study. Indian J Dermatol Venereol Leprol. 2017;83:47-54.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men. J Dtsch Dermatol Ges. 2011;9(Suppl 6):S1-57.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia areata: Review of epidemiology, clinical features, pathogenesis, and new treatment options. Int J Trichology. 2018;10:51-60.
- [CrossRef] [PubMed] [Google Scholar]
- Combined microneedling with topical Vitamin D3 or bimatoprost versus microneedling alone in the treatment of alopecia areata: A comparative randomized trial. J Cosmet Dermatol. 2023;22:1286-96.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of a bidirectional association between major depressive disorder and alopecia areata. JAMA Dermatol. 2019;155:475-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of pediatric alopecia areata: A systematic review. J Am Acad Dermatol. 2022;86:1318-34.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective comparative study of two concentrations of intralesional triamcinolone acetonide in the treatment of patchy alopecia areata on the scalp. Clin Cosmet Investig Dermatol. 2020;13:795-803.
- [CrossRef] [PubMed] [Google Scholar]
- History of follicular unit excision. Indian J Dermatol Venereol Leprol. 2021;87:315-8.
- [CrossRef] [PubMed] [Google Scholar]
- Automation of hair transplantation past, present and future In: Harahap M, ed. Innovative techniques in skin surgeon. New York: Marcel Dekker, Inc.; 2002. p. :489-502.
- [CrossRef] [Google Scholar]
- Hair transplantation for men. J Cosmet Laser Ther. 2008;10:154-60.
- [CrossRef] [PubMed] [Google Scholar]
- Body hair transplant by follicular unit extraction: My experience with 122 patients. Aesthet Surg J. 2016;36:1101-10.
- [CrossRef] [PubMed] [Google Scholar]
- A critical assessment of the evidence for low-level laser therapy in the treatment of hair loss. Dermatol Surg. 2017;43:188-97.
- [CrossRef] [PubMed] [Google Scholar]






