Translate this page into:
Granulomatous cheilitis and lingua plicata – An incomplete triad of Melkersson–Rosenthal syndrome

*Corresponding author: Yogindher Singh, Department of Dermatology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India. yogindher@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vijay V, Arumugam I, David B, Singh Y. Granulomatous cheilitis and lingua plicata – An incomplete triad of Melkersson–Rosenthal syndrome. CosmoDerma. 2023;3:183. doi: 10.25259/CSDM_237_2023
Abstract
Granulomatous cheilitis is a rare granulomatous inflammatory disorder characterized by chronic swelling of the lips. It is an oligosymptomatic form or an incomplete form of Melkersson–Rosenthal syndrome, which comprises recurrent orofacial edema, facial nerve palsy, and fissured tongue. Here, we present a case of a 45-year-old female with persistent upper lip swelling for three months.
Keywords
Melkersson–Rosenthal syndrome
Granulomatous cheilitis
Lingua plicata
INTRODUCTION
Granulomatous cheilitis (GC) also known as Meischer cheilitis (named after Meischer, who first described it in 1945) is a rare idiopathic inflammatory disorder seen only in about 0.08% of general population. It is characterized by recurrent orofacial swelling and considered as a monosymptomatic form or incomplete variant of Melkersson–Rosenthal syndrome (MRS).[1] Melkersson in 1928 related facial palsy and facial edema. Rosenthal in 1931 finished the triad of MRS syndrome by adding fissured tongue (lingual plicata).
CASE REPORT
A 45-year-old woman presented with persistent painless swelling of the upper lip [Figure 1] for the past three months. No history of transient wheals elsewhere in the body. Patient denied any food or drug allergies. She gave history of being treated with steroid injections and antihistamines in the past, with no improvement. She was not a known case of systemic hypertension and was not on any antihypertensives. She did not have any abdominal pain, diarrhea, blood in stools, loss of weight or loss of appetite. There was no history of deviation of angle of mouth, dribbling of saliva, inability to close the eyes, dry eyes, blurred vision or excessive tears. There was no history of headache, tinnitus, giddiness, hard of hearing, dryness in the mouth or difficulty in swallowing. There were no similar complaints in other family members. On examination, there was swelling of the upper lip with few linear fissures. Multiple fissures were present over the dorsum of the tongue [Figure 2]. No deviation of angle of mouth or loss of nasolabial fold or inability to close the eyes was seen on examination. No lymphadenopathy was present. Complete hemogram was normal. Mantoux and AFB staining were negative. Peripheral blood smear was normal. Chest radiography was normal. A 4 mm punch biopsy was taken from the upper lip and sent for histopathological examination. Hematoxylin and eosin-stained section showed ill formed granulomas composed of epithelioid histiocytes with surrounding dense inflammatory infiltrate [Figures 3 and 4]. Special stains for acid fast bacilli were negative, and no fungal elements were seen in the biopsy specimen. From these findings, the diagnosis of incomplete variant of MRS was made, and patient was started on minocycline 100 mg daily for four weeks. The patient is currently on follow-up.
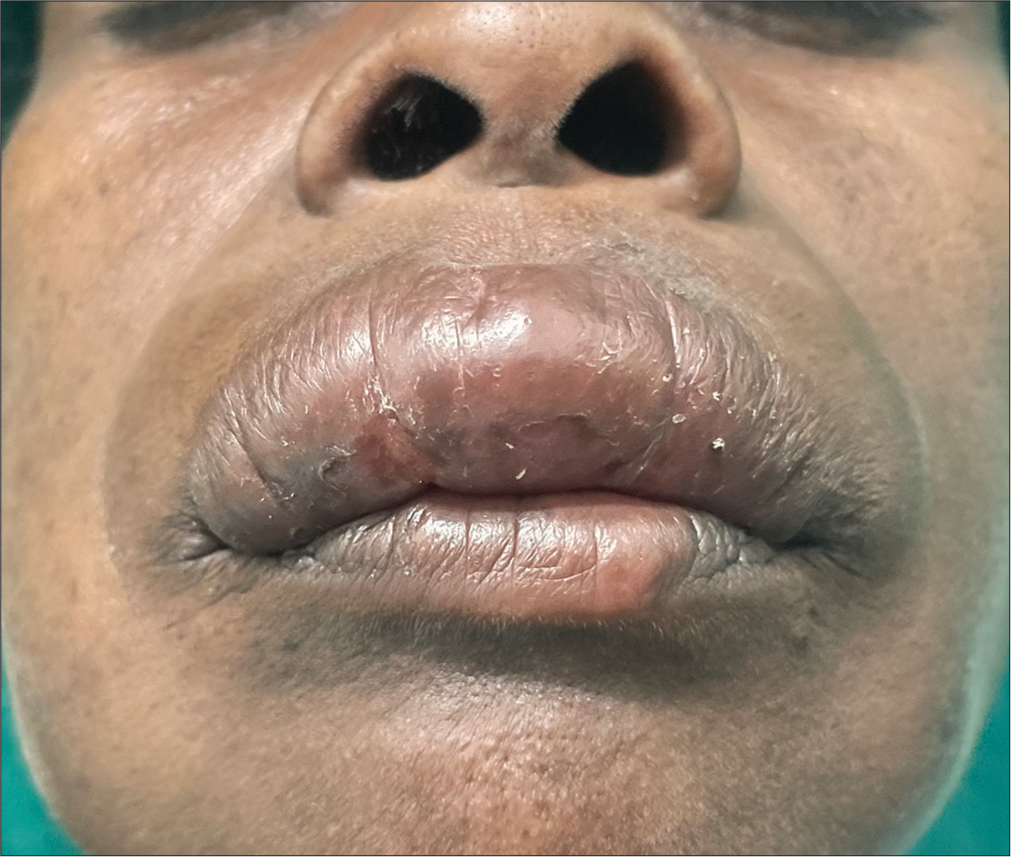
- Swelling of the upper lip.

- Swelling of upper lip with fissures in the dorsum of the tongue.

- Hematoxylin and eosin stained section-scanner view (×40 magnification) shows ill formed granulomas (black circle) composed of epithelioid histiocytes with surrounding dense inflammatory infiltrate.

- Hematoxylin and eosin stained section (×100 magnification) shows magnified image of ill formed granuloma (black circle) with epithelioid cells (red arrow) and surrounding dense inflammatory infiltrate (yellow arrow).
DISCUSSION
The GC is a chronic disorder, which presents with persistent swelling of the lips due to granulomatous inflammation. It is considered as a subset of orofacial granulomatosis (OFG) and an incomplete variant of MRS syndrome. [1] The exact cause of GC is unknown. However, various theories have been proposed regarding the cause of GC, which includes – genetic (chromosome 9p11), infectious (Peptostreptococcus, Streptococcus, Mycobacterium tuberculosis, and Mycobacterium leprae), dietary (food and food additives), allergens, and dental materials such as amalgam, gold, mercury, and zinc, as a part of Crohn’s disease.[2] Wiesenfeld et al., in 1985, first described OFG as idiopathic persistent enlargement of the lips, oral ulcers, and other orofacial features in the absence of any systemic associations.[3] It has a slight preponderance to young females.[4] Histopathology of GC reveals non-caseating granulomas.[1]
The MRS syndrome is a neurocutaneous syndrome with an incidence of 0.08%.[2] It has an autosomal dominant inheritance. The classical presentation of MRS with the triad of persistent orofacial edema, fissured tongue, and facial nerve palsy is seen only in 8–25%.[2] Recurrent lip/orofacial edema is the most common presenting feature of MRS syndrome.[5] The facial edema is usually unilateral and mostly seen in upper lip in majority of patients.[4] Fissured tongue is seen in 40% of MRS patients.[6] Orofacial edema in combination with facial nerve palsy was seen only in 22% of cases by Chan et al.[7] The combination of GC with fissured tongue as seen in our case is a rare occurrence. Differential diagnoses of GC include sarcoidosis, tuberculosis, leprosy, Crohn’s disease, and non-Hodgkin lymphoma. Treatment for GC includes intralesional corticosteroids with or without immunomodulators as first-line therapy and systemic corticosteroids as second-line therapy.[2] Relapse can occur after steroid therapy. Other treatment modalities include antibiotics such as metronidazole and immunomodulators. Cheiloplasty can be done in cases with lip deformity. Prophylactic facial nerve decompression can be done in patients with frequent facial nerve palsy to prevent progression and future attacks.[4]
CONCLUSION
The GC is not a condition that is commonly seen in practice. This results in significant discomfort to the patient with persistent lip swelling. Patients are also psychologically affected, as lips are of significant cosmetic concern. We report this case for its rarity and to emphasize the importance of thinking about GC as a differential diagnosis when a patient presents with persistent/recurrent lip swelling.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cheilitis granulomatosa: A case report with review of literature. Indian J Dermatol. 2013;58:242.
- [CrossRef] [PubMed] [Google Scholar]
- Granulomatous cheilitis of Miescher: A rare entity. BMC Womens Health. 2023;23:118.
- [CrossRef] [PubMed] [Google Scholar]
- Oro-facial granulomatosis-A clinical and pathological analysis. Q J Med. 1985;54:101-13.
- [Google Scholar]
- Melkersson-Rosenthal syndrome misdiagnosed as recurrent Bell's palsy: A case report and review of literature. Allergy Asthma Clin Immunol. 2021;17:8.
- [CrossRef] [PubMed] [Google Scholar]
- Melkersson-Rosenthal syndrome: Case report of a 30-year misdiagnosis. J Oral Maxillofac Surg. 2005;63:1035-9.
- [CrossRef] [PubMed] [Google Scholar]
- Melkersson-Rosenthal syndrome revisited as a misdiagnosed disease. Am J Otolaryngol. 2009;30:33-7.
- [CrossRef] [PubMed] [Google Scholar]
- Melkerrson-Rosenthal syndrome with cardiac involvement. J Clin Neurosci. 2004;11:309-11.
- [CrossRef] [PubMed] [Google Scholar]






