Translate this page into:
Evolution and principles of dermoscopy

*Corresponding author: Ritu Mittal, Department of Skin and Venereal Diseases, Government Medical College and Rajindra Hospital, Patiala, Punjab, India. mittalritu023@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahu P, Mittal R. Evolution and principles of dermoscopy. CosmoDerma. 2025;5:41. doi: 10.25259/CSDM_222_2024
Abstract
Dermoscopy, also known as dermatoscopy or epiluminescence microscopy, is a non-invasive diagnostic technique that allows detailed visualization of skin structures invisible to the naked eye. The origin dates back to the Renaissance era; however, its clinical utility became evident in the 20th century, particularly for differentiating benign and malignant tumors. Today, the advancements in dermoscopic technology, such as the integration of polarized and non-polarized techniques, have enhanced its diagnostic precision and management of various inflammatory dermatoses, pigmentary disorders, infectious conditions, and diseases of the hair, scalp, and nails. Superficial structures are better visualized with non-polarized dermoscopic technique which requires a liquid interface and direct contact between the dermoscope and the skin. Polarized dermoscopic technique, on the other hand, enables visualization of structures in the deeper layers of epidermis and papillary dermis and can be used in contact or non-contact mode, with or without a liquid interface. Modern developments like ultraviolet reflectance dermoscopy further aid in the management of various pigmentary disorders, superficial infections, and porphyrias.
Keywords
Components
Dermoscopy
History
INTRODUCTION
Dermoscopy, also referred to as dermatoscopy, epiluminescence microscopy, or skin surface microscopy, dates back to the Renaissance era, predating dermatology as a science.[1] However, its clinical utility became evident in the 20th century, particularly for diagnosing and differentiating benign and malignant tumors.[1] Today, dermoscopy is widely applied in the evaluation of inflammatory dermatoses, pigmentary disorders, infectious conditions, and diseases of the hair, scalp, and nails.
HISTORICAL DEVELOPMENT
The origins of dermoscopy trace back to the 17th century when Dr. Pierre Borel first used a microscope to examine nail bed capillaries.[1] In 1663, Johan Kohlhaus and later Carl Hueter confirmed the diagnostic potential of magnification in capillary observation.[1] A major leap occurred in 1878 when Ernst Abbe and Carl Zeiss introduced the use of cedar oil in microscopy, improving image resolution through immersion microscopy.[1]
Paul Gerson Unna’s application of immersion oil in 1893 allowed better visualization of the epidermis, utilizing Brewster’s angle to reduce light reflection and illuminate skin lesions.[1] Between 1916 and 1920, Mueller introduced monocular microscopic examination, achieving magnifications up to 172 times, while Saphier developed binocular microscopy, using dermoscopy to distinguish syphilis from tuberculosis lesions.[1]
In 1922, Jeffrey Michael in the USA introduced the concept of dermatoscopy with a binocular microscope.[1] By 1950, Leon Goldman coined the term “dermatoscopy” and developed a portable monocular dermatoscope for differentiating skin tumors, though its weak light source limited its effectiveness.[1]
The pivotal moment in modern dermoscopy came in 1971 when Dr. Ronald Mackie demonstrated the advantages of surface microscopy in diagnosing pigmented lesions, particularly melanomas.[1] During the 1980s and 1990s, advances in portable binocular dermatoscopes emerged, with W. Stolz introducing the “ABCD rule” in 1989 for melanoma diagnosis. That same year, the Delta 10 dermatoscope, created by Heine, revolutionized skin lesion evaluation with a halogen lamp and ×10 magnification.
In 1991, Friedman et al. popularized the term “dermoscopy” while in 2001, the DermLite handheld device introduced polarized illumination, eliminating the need for immersion oil and enabling deeper visualization.[1,2]
PRINCIPLES AND OPTICAL COMPONENTS OF DERMOSCOPY
Dermoscopy is a non-invasive diagnostic technique that allows detailed visualization of skin structures invisible to the naked eye. Its functionality relies on key components:
Illumination System: First-generation dermatoscopes utilized halogen lamps, producing images with a yellowish hue. Modern devices incorporate white light-emitting diodes (LEDs), which offer energy efficiency and superior image clarity.[3]
Achromatic Lens: Typically, these lenses provide ×10 magnification, ensuring detailed observation of skin structures.[3]
Contact Plate: Made from multi-coated silicone glass, contact plates can be graduated (with inscribed measurement scales) or non-graduated.[3]
Power Supply: Advancements have improved energy consumption and device portability.[3]
UNAIDED SKIN EXAMINATION
Light interacting with the skin undergoes reflection, refraction, diffraction, and absorption.[3] The reflection (specular reflectance) from the stratum corneum, with its high refractive index (1.55 compared to air’s 1.0), limits visualization of deeper structures. Unaided examination primarily assesses the stratum corneum and, to a lesser extent, superficial dermal features.
OPTICAL PRINCIPLES OF NON-POLARIZED DERMOSCOPY (NPD)
NPD employs a glass plate (refractive index: 1.52) and an interface fluid to minimize glare from specular reflectance, enabling better visualization of superficial layers of skin [Figure 1a]. Immersion fluids such as 70% alcohol, ultrasound gel, or mineral oil ensure optical matching with the skin. Notably, 70% alcohol is preferred for its antibacterial properties and image clarity, while ultrasound gel is ideal for nail examinations due to its viscosity.[4]
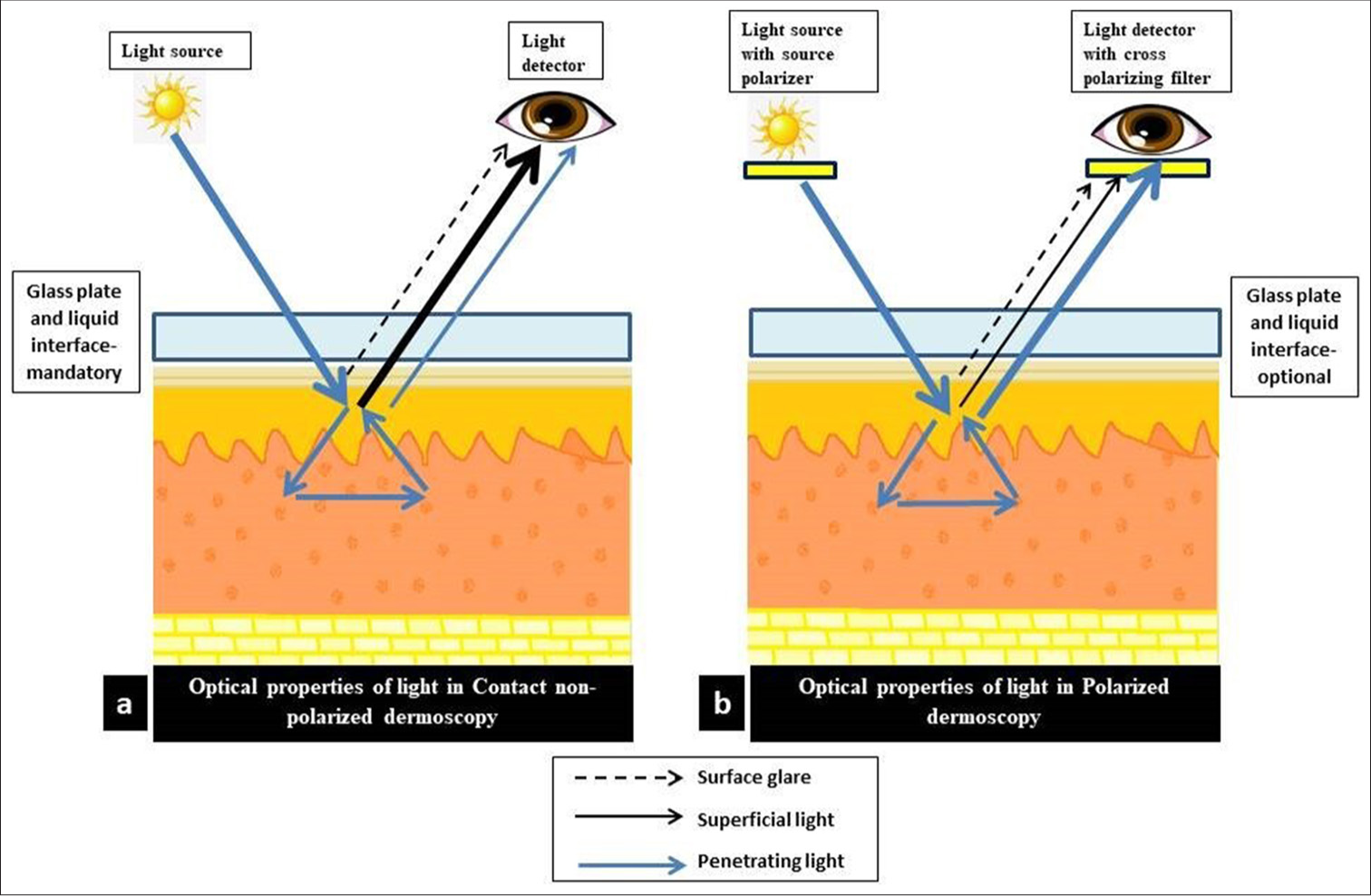
- (a) Most of the incident light is absorbed and reflected from the superficial layers of the epidermis after undergoing minimal scattering events (thick black line). Some of the light is reflected off the stratum corneum (dotted black line) which is the surface glare. A small fraction of the light penetrates more deeply and is absorbed and reflected back after multiple scattering events (thin blue line). (b) Light emitted from the dermoscopy unit (source) passes through a polarizer resulting in the generation of polarized unidirectional light. Light reflected from the stratum corneum or surface glare (dotted black line) maintains its original polarization, and light that is absorbed in the superficial layers of the epidermis (thin black line) does not undergo enough scattering events to result in randomization of polarization, hence cannot pass through the cross-polarizing filter. Only light penetrating more deeply (thick blue line) and/or undergoing multiple scattering events will result in randomization of polarization. When this light is reflected back, it will be able to pass through the cross-polarization filter, thus allowing the observer to visualize the deeper structures.
OPTICAL PRINCIPLES OF POLARIZED DERMOSCOPY (PD)
PD uses cross-polarization to overcome specular reflectance without requiring immersion fluids. Two orthogonally positioned polarizing filters allow light that loses polarization upon entering the skin to pass through while blocking reflected polarized light. This method enables visualization of structures within the dermo-epidermal junction and superficial dermis (60–100 microns depth), though it is less effective for observing superficial epidermal structures, such as milia-like cysts or comedo-like openings [Figure 1b].[4]
Modern PD devices offer both contact and non-contact options. Contact PD, when combined with immersion fluids, enhances image clarity by further reducing surface glare.[4] While PD and NPD provide comparable images for most lesions, subtle differences exist, making them complementary techniques in dermoscopy [Table 1, Figures 2-4].
| Non-polarized | Polarized | |
|---|---|---|
| Factor | Classic contact dermoscopy | Contact and non-contact dermoscopy |
| Technique | Requires a liquid interface and direct contact between the dermoscope and the skin | Can be used in contact or non-contact mode, with or without a liquid interface. Direct contact and liquid interface provide better image quality |
| Skin layers | Superficial layers are better visualized | Deep layers of epidermis and papillary dermis are better visualized |
| Colors and structures | • Blue-white veil due to orthokeratosis- more conspicuous • Milia-like cysts and comedo-like openings are more conspicuous • Steel blue color in blue nevi appears more homogeneous • Regression structures (peppering, blue-white areas, and grey color) are more conspicuous • Ability to visualize vascular structures depends on the amount of pressure applied to the skin • White shiny structures cannot be visualized adequately |
• Pink and red colors are more conspicuous • Milia-like cysts and comedo-like openings are less conspicuous • Blue color in blue nevi will appear darker, with different hues • White scar-like areas are more conspicuous • Vascular structures and collagen are more conspicuous • White shiny streaks also known as crystalline structures are more conspicuous |
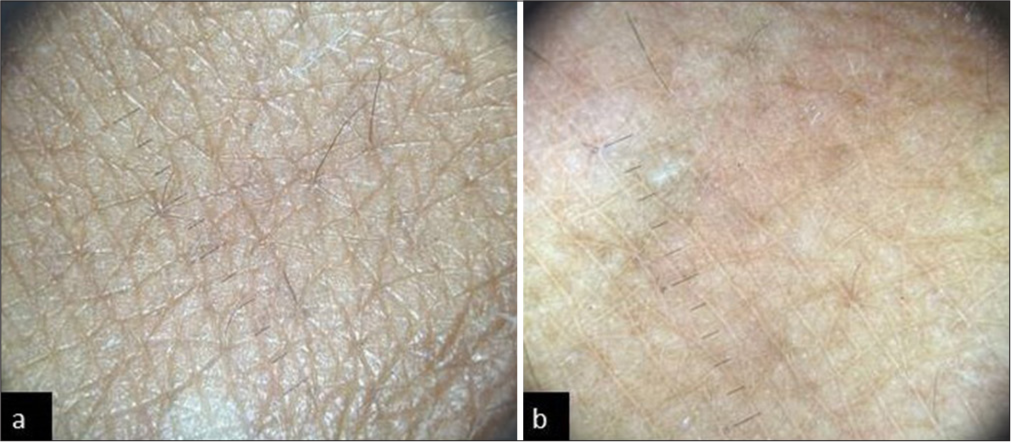
- (a) Non-polarized dermoscopy showing normal skin markings. (b) Polarized dermoscopy showing light brown reticular pattern of normal skin.
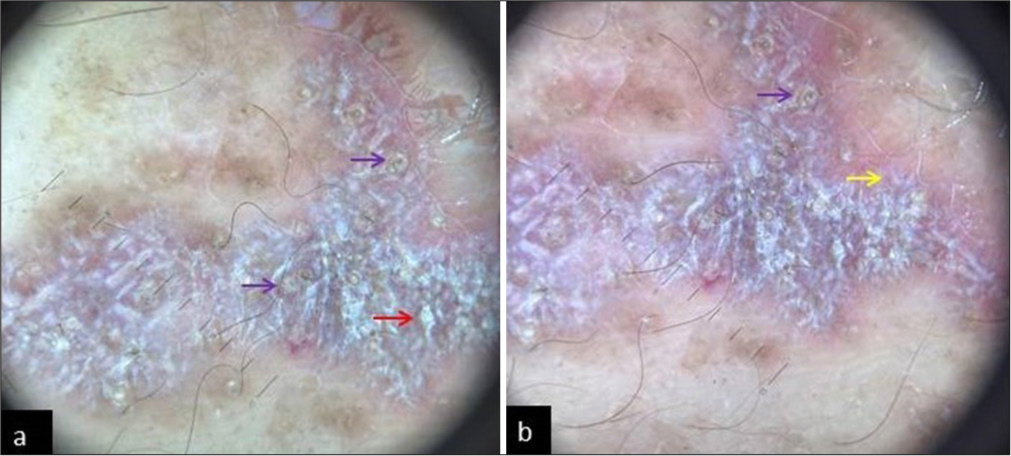
- (a) Non-polarized dermoscopy of Lichen Planus showing patchy scaling (red arrow) and comedo-like openings (purple arrows). (b) Polarized dermoscopy of the same lesion showing Wickham striae (yellow arrow) and comedo-like openings (purple arrow).
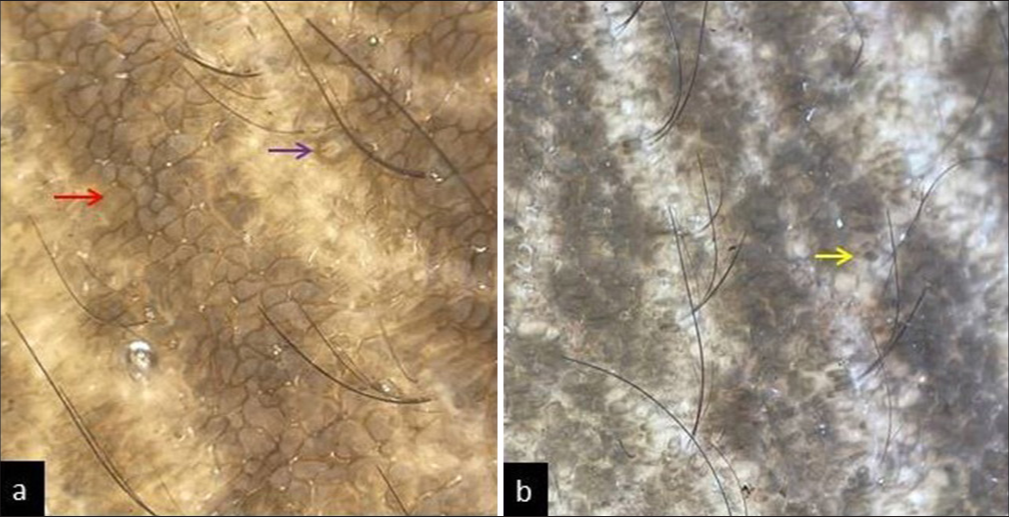
- (a) Non-polarized dermoscopy of acanthosis nigricans showing exophytic papillary structures (red arrow), linear crista cutis, sulcus cutis, and perifollicular hyperpigmentation (purple arrow). (b) Polarized dermoscopy of the same site showing linear crista cutis and sulcus cutis with irregular brown globules (yellow arrow).
The most important parameters that should be assessed when applying dermoscopy in general dermatology include background color, pigment pattern, vascular structures (including morphology and distribution), scales (including color and distribution), follicular structures, and specific clues.[5] The different colors observed on dermoscopy can be attributed to chromophores. These include − dirt/dust on hair or skin (black/brown), keratin (brown), sebum (yellow), blood (black or red), and collagen (white). Melanin is another chromophore that can ascribe various colors depending on the depth of pigment − stratum corneum (black), stratum malpighii (light to dark brown), papillary dermis (gray), and reticular dermis (blue).[6]
JOURNEY OF DERMOSCOPY IN SKIN OF COLOR
Dermoscopy has been extensively used not only in light phototype patients (I–III) but also in diagnosing, managing, and monitoring diseases in the skin of color patients. The dermoscopic patterns in these patients differ due to the darker background color, absence of key findings such as erythema, lesion shade, or surface changes (e.g., pigmentation and telangiectasias), and specific reactions characteristic of skin of color (e.g., pigment lability and a tendency toward follicular or sclerotic reactions). The literature on dermoscopy in the skin of color is most extensive in inflammatory and infectious dermatoses, reflecting their high prevalence in dark-skinned populations. While trichoscopy has been well-studied, providing more reproducible data, research on skin tumors remains limited, with few studies and lower levels of evidence, likely due to their lower prevalence in skin color. Continued research in this area is essential to enhance diagnostic accuracy and improve patient outcomes.[7]
MODERN DEVELOPMENTS
Recent innovations include the DermLite DL5 (2022), which allows toggling between cross-polarized, nonpolarized, parallel, and linear polarization modes for detailed visualization of superficial and deep skin structures. In addition, computer-assisted (digital) dermoscopy and confocal microscopy have provided complementary tools for analyzing lesions. These dermoscopes with high-resolution image capture and analytical capability are used for serial evaluation of various lesions with the help of artificial intelligence.[5]
Multispectral dermoscopes and ultraviolet (UV) dermoscopes enable better visualization of specific structures. For example, surface pigmentation is better viewed under blue light, superficial vascularity under yellow light, and deeper pigmentation and vascularity with red light which penetrates deeper.[5] UV reflectance dermoscopy, a newer advancement, combines traditional dermoscopy with UV light to assess pigmentary disorders such as vitiligo and melasma, as well as superficial infections and porphyrias. Modern dermatoscopes now feature smartphone compatibility, enhanced magnification, improved charge times, and user-friendly designs, making them indispensable tools for dermatologists worldwide.
CONCLUSION
Initially, it was developed as a tool for diagnosing malignant skin lesions. Now, in the present era, advancements not only improve early detection but also enhance patient outcomes by enabling therapeutic monitoring of general dermatological conditions. One of the most exciting aspects of contemporary dermoscopy is its growing application in skin color. The advancements in dermoscopic technology, such as the integration of polarized, cross-polarized, and UV dermoscopes, have enhanced its diagnostic precision and management of various dermatological conditions. As technological advancements continue, dermoscopy remains an indispensable tool in dermatology, offering an unparalleled window into the microstructures of the skin. Thus, the authors hope this article serves as a valuable resource for dermatologists, and researchers, by bridging historical advancements with modern innovations.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required, as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Dermoscopy saga-a tale of 5 centuries. Indian J Dermatol. 2021;66:174-8.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant melanoma in the 1990s: The continued importance of early detection and the role of physician examination and self-examination of the skin. CA Cancer J Clin. 1991;41:201-26.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy: Physics and principles. Indian J Dermatopathol Diagn Dermatol. 2017;4:27-30.
- [CrossRef] [Google Scholar]
- The scope of the dermoscope. Indian Dermatol Online J. 2016;7:359-63.
- [CrossRef] [PubMed] [Google Scholar]
- Role of dermoscopy in the assessment of difficult to diagnose cases of pigmentary dermatoses: Study from a tertiary care hospital. Pigment Int. 2022;9:93-106.
- [CrossRef] [Google Scholar]
- Dermoscopy in skin of color: The journey so far. Dermatol Pract Concept. 2023;13:e2023305S.
- [CrossRef] [PubMed] [Google Scholar]







