Translate this page into:
Dermoscopy in primary and secondary syphilis: A report of three cases

*Corresponding author: Balachandra Suryakant Ankad, Professor and Head, Department of Dermatology, S Nijalingappa Medical College, Bagalkot, Karnataka. drbsankad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ankad BS, Hurakadli SS, Nikam BP. Dermoscopy in primary and secondary syphilis: A report of three cases. CosmoDerma 2023;3:163.
Abstract
Dermoscopy is non-invasive tool as a diagnostic adjunctive in clinical dermatology. It demonstrates definitive features in infective and inflammatory dermatoses. Syphilis is emerging again as newly diagnosed cases are being reported and treated across the country. There is a sparsity in the dermoscopic reports in syphilis. It shows characteristic patterns in primary and secondary syphilis. However, dermoscopic monitoring of syphilitic lesions is lacking in the literature. Here, we report cases of syphilis with treatment monitoring by dermoscopy.
Keywords
Dermoscopy
Syphilis
Treatment
Brownish-yellow globules
INTRODUCTION
Syphilis is a chronic infectious disease caused by Treponema pallidum. It is an uncommon sexually, blood contracted, or congenitally transmitted disease. Untreated syphilis infection has a triphasic natural history that usually progresses through three stages primary, secondary, and tertiary. The cutaneous lesions of secondary syphilis include macular, papular or pustular, lichenoid, psoriasiform lesions. Although the clinical features are characteristic for the diagnosis in most cases, sometimes, it is difficult to differentiate it from other annular maculopapular dermatosis with scaling.[1] Dermoscopy used to improve the diagnosis accuracy in the skin lesions including syphilis wherein it demonstrates characteristic findings.[2] Although dark ground microscopy and serological testing remain gold standard for diagnosis of syphilis, there is an opportunity to explore newer diagnostic non-invasive techniques to improve upon the diagnosis of syphilis. Here, we report three cases of syphilis where in dermoscopy and histopathological features were correlated and treatment response was monitored by dermoscopy.
CASE REPORTS
Case 1
A 22-year-old unmarried male presented with asymptomatic skin rashes for 6 months. Examination showed bilaterally symmetrical multiple erythematous macules and papules over the upper limbs, back [Figure 1a], and trunk. Oral examination was normal. He had a history of unprotected penovaginal intercourse with 2 unknown partners over period of last 2 years with genital lesions. Buschke-Ollendorff sign was negative. Dermoscopy of papules on back revealed ill-defined brownish-yellow globules with linear and dotted vessels in addition to hemorrhagic crust. Scaling was seen in annular and diffuse patterns. Pigment network was distorted [Figures 1b and 2a]. A 4-mm punch biopsy showed epidermal hyperplasia and superficial and deep periappendageal and perivascular wedge-shaped granulomatous infiltrate. Superficial infiltrate consisted of lymphohistiocytosis and many plasma cells and few interstitial neutrophils [Figure 2b]. Serology revealed that venereal disease research laboratory (VDRL) was reactive with 1:32 dilution and T. pallidum hemagglutination assay (TPHA) was positive. The patient received single intramuscular injection of 2.4 million units of benzathine penicillin. After 3 weeks of treatment, erythema and scaling were resolved [Figure 3a]. Dermoscopy showed reduction in the scales, brownish-yellow globules, and vascular structures [Figure 3b].
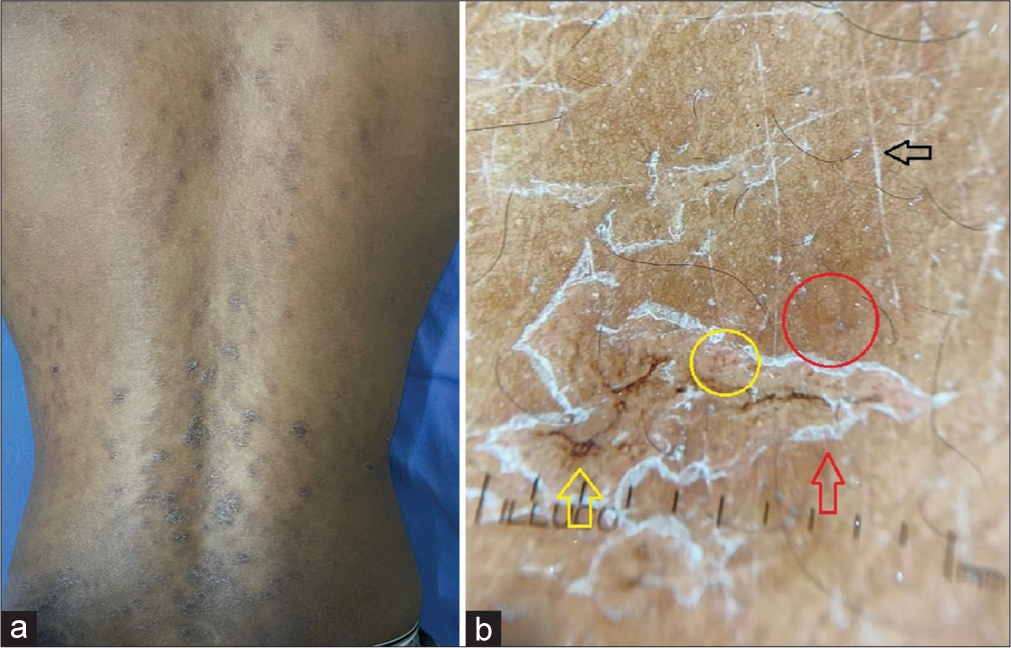
- (a) Clinical image of secondary syphilis showing scaly plaques on the back. (b) Dermoscopy shows dotted (yellow circle) and linear (yellow arrow) vessels, brownish-yellow globules (red circle) with diffuse scales (red arrow). Note the scales in the skin lines (black arrow) and distorted pigment network.
![(a) Dermoscopy shows dotted (yellow circle) and linear (yellow arrow) vessels, brownish-yellow globular structures (yellow star) with scales (yellow box). Pigment network is distorted. (b)Histopathology shows epidermal hyperplasia, superficial, and deep periappendageal and perivascular wedge-shaped granulomatous infiltrate [× 100, H and E].](/content/130/2023/3/1/img/CSDM-3-163-g002.png)
- (a) Dermoscopy shows dotted (yellow circle) and linear (yellow arrow) vessels, brownish-yellow globular structures (yellow star) with scales (yellow box). Pigment network is distorted. (b)Histopathology shows epidermal hyperplasia, superficial, and deep periappendageal and perivascular wedge-shaped granulomatous infiltrate [× 100, H and E].
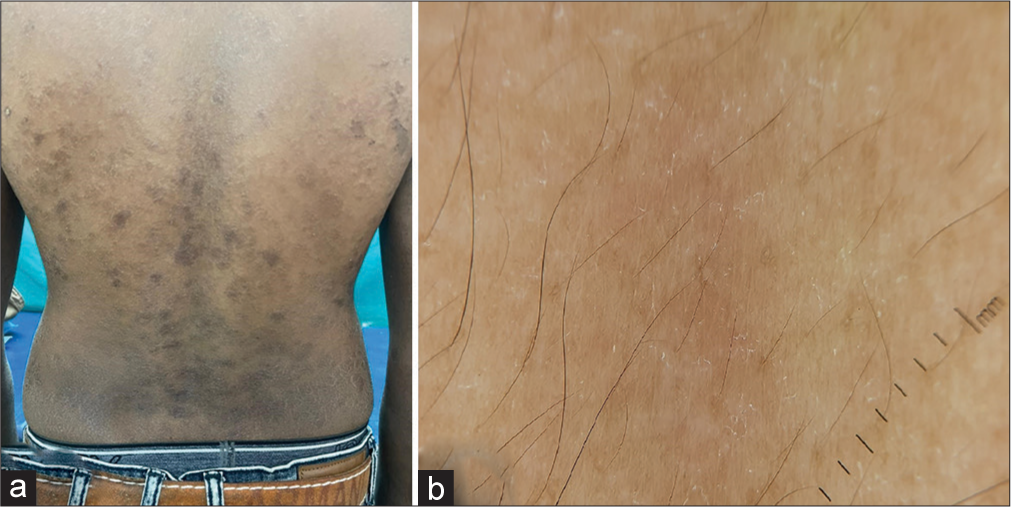
- (a) Clinical image after treatment shows reduction in the scales and fading of patches and plaques. (b) Dermoscopy after treatment shows a faint pinkish hue with minimal scales.
Case 2
A 31-year-old married male presented with multiple erythematous lesions all over the body for 5 months. He was married for 3 years and has had history of unprotected penovaginal intercourse with 3 unknown partners over period of last 2 years. He was taking antiretroviral treatment for human immunodeficiency virus infection for 2 years. He had a history of genital lesion in past. Cutaneous examinations showed diffuse, non-confluent, and erythematous maculopapular rash over the trunk, back [Figure 4a], and extremities. BuschkeOllendorff sign was positive. Dermoscopy of erythematous lesion showed pinkish hue and distorted pigment network with dotted vessels. Scales were scanty and located in skin furrow [Figure 4b]. VDRL was reactive with 1:8 dilution and TPHA was weakly positive. The patient received single intramuscular injection of 2.4 million units of benzathine penicillin. At a follow-up visit 3 weeks after treatment, there clinical improvement [Figure 5a] and pinkish hue and dotted vessels were not seen in dermoscopy [Figure 5b].
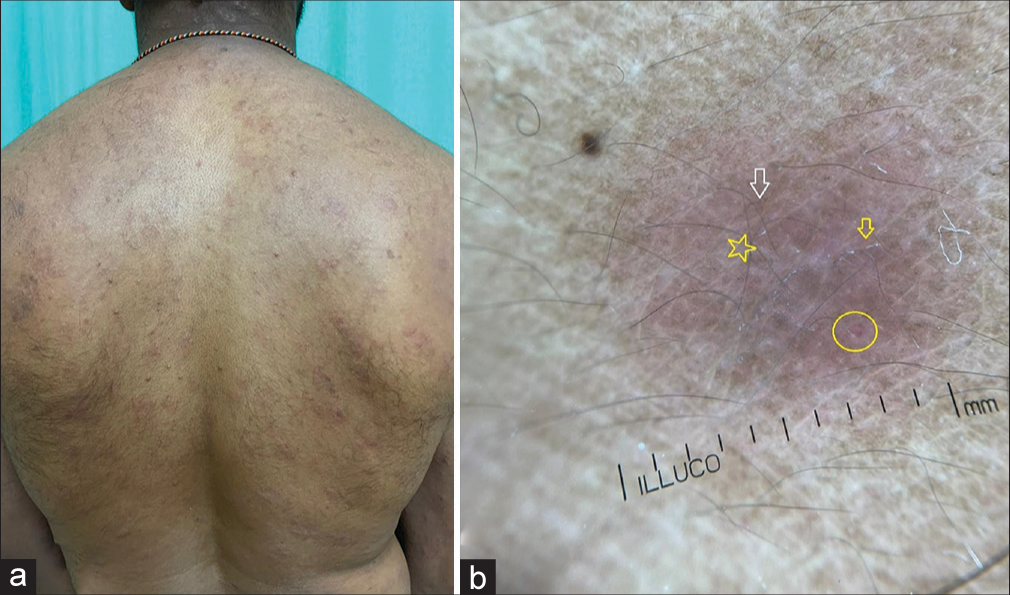
- (a) Clinical image of secondary syphilis showing coppery red nodules and plaques on the back. (b) Dermoscopy shows dotted vessels (yellow circle), faint brownish-yellow globular structures (white arrow) on pinkish background (yellow star). Note the scales in the skin lines (yellow arrow).
- (a) Clinical image after treatment, showing disappearance of nodules and plaques. (b) Dermoscopy after treatment, shows a faint pinkish hue with minimal scales.
Case 3
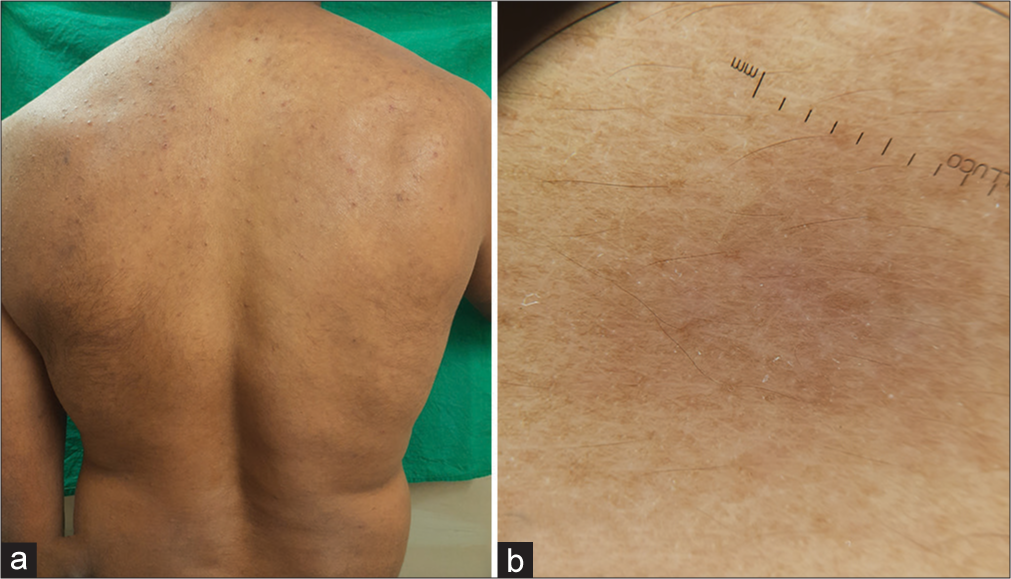
A 40-year-old married male presented with asymptomatic ulcerative lesion over the prepucial skin in the past 1 month.
He developed it 10 days after unprotected sexual contact with unknown person. Examination revealed punched-out ulcer with erythematous edges [Figure 6a]. Dermoscopy showed glomerular, linear looped, and numerous dotted vessels with linear white structure in an annular pattern at the periphery. Center of the lesion showed white structureless area with adherent fabric fibers [Figure 6b]. VDRL was reactive with 1:16 dilution and TPHA was positive. The patient received single intramuscular injection of 2.4 million units of benzathine penicillin. This patient could not come for follow-up. Faceplate of the dermoscope was cleansed with isopropyl alcohol each time in all three cases.
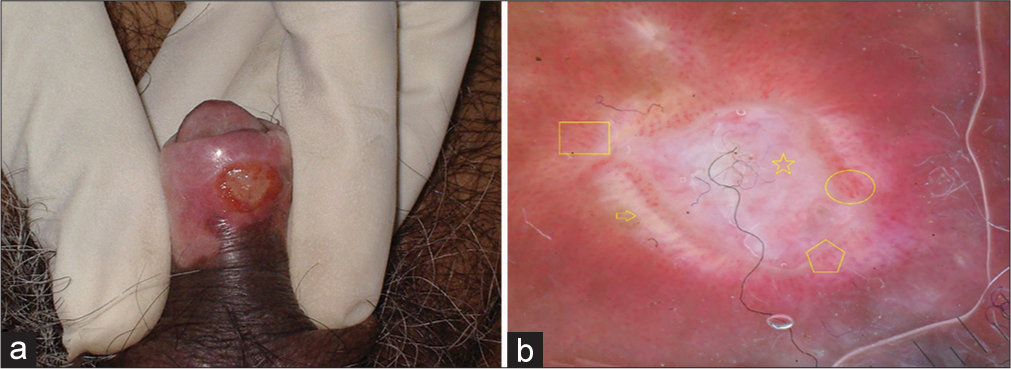
- (a) Clinical image of primary syphilis showing well defined punched-out ulcer with erythematous edge on the ventral aspect of penis. (b) Dermoscopy shows dotted (yellow pentagon), glomerular (yellow circle) and linear looped (yellow box) vessels, with central white area (yellow star) and peripheral whitish linear structure (yellow arrow). Note the adherent fabric fibers.
DISCUSSION
Primary syphilis is characterized by painless ulcers, called as chancre, that disappear within 6 weeks. If it is untreated, secondary stage appears within 10 weeks. Skin lesions are the most common presentation that can mimic a variety of dermatoses, including pityriasis rosea, psoriasis, drug eruption, and erythema multiforme.[1] The most consistent dermoscopic features in secondary syphilis include diffuse orange or yellowish-red background with vascular structures.[2] Macular lesions reveal pale-pink background. Dotted or linear vessels are noted rarely. In contrast, papules show orange background with dotted or linear vessels.[3] In this report, papular lesions demonstrated diffuse brownish-yellow structures with dotted and linear vessels. The second case with papules showed pinkish background with subtle brownish-yellow structures. The vascular blush may obscure the visibility of brown structures. Thus, dermoscopic features vary based on the clinical morphology of the lesions and skin phototype as well. In skin of color, yellow or orange structures appear as brownish-yellow structures.
Scales are also important features in secondary syphilis. Macular lesions show fine scales even in the absence of visible scales clinically. Papular lesions reveal scales in diffuse or annular fashion. The latter is termed as Biett’s collarette. Annular scales are particularly seen in palmoplantar lesions.[4] In this study, scales were seen markedly in a diffuse pattern and in skin lines in truncal lesions. Dermoscopically, primary chancre shows reddish area in the center with white border at periphery. Linear and irregular serpentine vessels are found in the white border.[5] However, dotted, glomerular, and linear looped (hair-pin) vessels were noted in this case in addition to central whitish-red area and white border at periphery. Morphology and arrangement of vessels could be related to the duration of lesions and location of primary chancre. Hence, there is discrepancy of vascular structures in this case and previous description.
CONCLUSION
Dermoscopy assists in the diagnosis of primary and secondary syphilis as an adjunctive to clinical acumen. Furthermore, it also clarifies the response to the treatment by showing defining patterns. Importantly, the dermoscopic images are documented which are compared before and after the treatment that plays a significant role in convincing the patient. Thus, dermoscopy is recommended in daily clinical practice. This report highlights the definitive diagnosis and analysis of therapeutic response by dermoscopy and ascertains the variability in the dermoscopic features according to skin phototypes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The biett collarette as an important dermoscopic finding of secondary syphilis. Skin J Cutan Med. 2022;6:445-7.
- [CrossRef] [Google Scholar]
- Syphilis, the great imitator-clinical and dermoscopic features of a rare presentation of secondary syphilis. Int J Environ Res Public Health. 2023;20:1339.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of Biett's sign and differential diagnosis with annular maculo-papular rashes with scaling. Indian J Dermatol Venereol Leprol. 2017;83:270-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy is a useful tool in the diagnosis of nodular secondary syphilis. BMJ Case Rep. 2022;15:e252200.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of skin infestations and infections (entomodermoscopy) part-1: Dermatozonoses and bacterial infections. An Bras Dermatol. 2021;96:735-45.
- [CrossRef] [Google Scholar]






