Translate this page into:
Carboxytherapy in esthetic medicine – A review

*Corresponding author: Uwe Wollina, Department of Dermatology and Allergology, Städtisches Klinikum Dresden, Dresden, Germany. uwollina@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Zelenkova H, Wollina U. Carboxytherapy in esthetic medicine – A review. CosmoDerma 2023;3:108.
Abstract
Carboxytherapy is a minimally invasive method used not only in esthetic medicine. It is defined as the transcutaneous or subcutaneous application of carbon dioxide gas. The treatment exerts effects on various levels including improvement of tissue oxygenation, vasodilatation, stimulation of fibroblasts, and antimicrobial activity. In this review, we will focus on facial and neck esthetics, localized adiposities and cellulite, and scars and stretch marks. We discuss reported evidence for these indications and safety issues. We also mention possible combinations with other treatments. In general, a repeated application is necessary to achieve desired results.
Keywords
Esthetic medicine
Carboxytherapy
Indications
Safety
INTRODUCTION
Carboxytherapy (CT) is the transcutaneous or subcutaneous administration of carbon dioxide (CO2) gas for therapeutic purposes. It was invented in Royat, France, in 1932, were heated carbonated water baths or application of water-saturated CO2 directly to the skin was used. It was noted that these procedures can improve wound healing and restore disturbed vascular (arterial) functions such as in Raynaud’s syndrome.[1,2]
CO2 is capable to penetrate intact skin after topical application. CO2 dissociates in the presence of water. The primary effect of CO2 is the correction of tissue hypoxia due to the Bohr effect. CO2 improves tissue perfusion by dilatation of the precapillary arterioles. It also stimulates rhythmical vasomotion, with an increase in amplitudes. The magnitude of this effect is dependent on temperature and CO2-concentration. Furthermore, it has been demonstrated that CO2 exerts a direct action on both the vascular smooth muscles and the activity of thermoreceptors of the skin. In addition, CO2 gas has a minor role in antibacterial activity in open wounds.[3] It temporarily stimulates fibroblast activity and lipolysis.[4-7]
ANIMAL STUDIES
In an animal experiment with ten male Wistar rats, CO2 was injected into the dermis and subcutis. Histologic studies demonstrated an increased collagen turnover, which was more pronounced with dermal compared to subcutaneous injections.[8] Abramo et al. demonstrated vasodilatation by CT which subsequently increased skin surface temperature.[9]
CO2 is capable to decrease the density and size of adipocytes in the treated area.[10,11] In mice, CT markedly increased vessel numbers and expressions of VEGFa, FGF1, and UCP1 genes in adipose tissues, while expression of Fasn/Fabp4 genes was modestly reduced.[11]
TREATMENT VARIABLES
Treatment variables are mode of application (continuous infusion versus bolus injection), depth in application, velocity (for infusions), frequency of application and duration of CT, and volumes of CO2 used. [Table 1] summarizes available technical equipment for CT.
| Name | Company | Remarks |
|---|---|---|
| Carboxyd-therapy unit CAT® | Unitronic, Kieselbronn, Germany | I |
| CDT light cart | Carbossi Terapia Italiana, Milan, Italy | I |
| CO2-promed | Alvi Prague, Czech Republic | I |
| Modula carbiox | Wavemed, San Cesareo, Italy | I |
| Carbo2 HPX | DTA Medical, Milan, Italy | B |
| Carbo-jett | Jett Company International, Zittau, Germany | B |
| Carb-o-xygen | Oxxot Medical, Milan, Italy | B |
| Carbo-pen | AAMS BFP Electonique; Montredat; France | B |
| Carboxy dolormed K | Wolf Medical Esthetics, Gerlingen, Germany | B |
| Dolor med | Kastner, Rastatt, Germany | B |
| DTP Carbo | Dermoequipos, Buenos Aires, Argentina | B |
| Venusian CO2 therapy | G Trading, Padova, Italy | B |
I: Infusion; B: Bolus injection, CO2: Carbon dioxide
There is a broad range of possible applications in diseases such as lymphedema, Raynaud’s disease, alopecia, vitiligo, psoriasis, delayed wound healing, and improvement of skin flap survival.[12-16]
CT IN ESTHETIC MEDICINE
In esthetic dermatology, both vasodilatation and intradermal collagen production and three-dimensional arrangement are of particular interest when it comes to CT. Thereby, the tone of the skin is improved, an effect that usually becomes visible after two sessions of treatment. CT is used to treat double chin, neck, and décolleté. It can also be used to improve lax skin on the abdomen, arms (even after brachioplasty), and inner thighs as part of body contouring and in post-liposuction conditions. CT has also been used to treat stretch marks. Facial lines on the glabella, crow’s feet, and fine lines around the eyes may be improved by CT; however, here the application requires great experience.
Since CT is often used in a combined approach, optimal timing is warranted. Patients need to be informed about adequate home care after the procedure.
COMBINING TREATMENTS
The following combinations with CT are possible on the same day:
Before the CT treatment session, it is possible to perform mild microdermabrasion or hydroabrasion.
After CT, a soft laser application or platelet-rich plasma (PRP) mask are options.
After 2–10 days after CT chemical peels, injection lipolysis, mesotherapy, microneedling, cell stimulation, cryotherapy, dermal fillers, botulinum toxin, PRP, or threads may be used. Combining CT and fillers or PRP seems very promising.[17]
SAFETY ISSUES
CT is a non-toxic minimal invasive procedure. It has been reported that CO2 can be used safely with intravascular bolus injections of up to 100 mL and continuous flows between 20 and 30 mL/s.[10]
CT is associated with temporary moderate pain and discomfort. Local pain reaction during CT is considered the main limiting factor for its use in clinical practice. The major adverse event is the development of hematomas.[18]
A rare complication is the development of subcutaneous emphysema. A 43-year-old woman was treated with CO2 mesotherapy for her thighs. A day later, she developed severe abdominal pain and a massive subcutaneous emphysema of the abdominal wall and flanks. There was a complete resorption of CO2 after 10 days, but dysesthesia and muscle contracture persisted for 3 weeks.[19]
A 24-year-old woman reported acute bilateral orbital emphysema developing 1 day after cosmetic periorbital CT. Orbital computed tomography confirmed bilateral preseptal emphysema extending into orbital space through. She was treated with oral prednisolone 50 mg/day. Gradually, periorbital pain and swelling subsided, and the symptoms resolved within 1 week.[20]
Inadvertent lipolysis is another possible adverse event.[21] A higher flow rate (velocity) of subcutaneous infusion may result in more adverse events in sensitive areas such as periorbital skin.[22]
Strict hygienic regimes are necessary to prevent soft-tissue infections. In a survey from France, cases of non-tuberculosis mycobacterial infections had been observed after CT.[23] The authors reported a deficiency of standard hygiene precautions and tap water misuse for cleansing of injection equipment or skin disinfection to be responsible.
There are no long-term adverse events known.[12-17] However, CT has some contraindications that should be respected. They include severe ischemic heart disease, acute embolism, thrombophlebitis and phlebothrombosis, gangrene, renal failure, untreated high blood pressure, stroke, pregnancy, lactation, severe obesity, acute infectious disease, fever, and blood clotting disorders.[17]
FACIAL AND NECK REJUVENATION
In an open trial, 90 patients with moderate to severe periorbital wrinkles and/or periorbital hyperpigmentation (POH) underwent subcutaneous injections of CO2 once a week for 7 weeks. Assessment of patients was performed before and 2 months after CT. The authors used visual analog scales and photographic documentation. Patients reported a reduction of fine lines and wrinkles and a decrease in POH.[24] Furthermore, skin elasticity became improved after CT.[25]
Another study compared the efficacy and safety of intense pulse light (IPL), radiofrequency (RF), and carboxytherapy in facial rejuvenation among 60 patients with facial wrinkles. Patients were divided into three groups. The patients received four sessions with 3–4 weeks interval. The follow-up was 3 months. Digital photographs and skin biopsies were taken before and after treatment. All procedures reduced signs of facial aging. The clinical improvement and patient’s satisfaction was best with IPL, followed by CT and RF.[26]
Thirty-five patients with POH were treated with subcutaneous CT in the tear trough weekly for 3 weeks. There was a 6-months follow-up. Standardized photography revealed a significant reduction of hyperpigmentation without major side effects.[27]
In a comparative split-face trial, POH patient was treated on one side with CT once a week and on the other side with PRP every other week. Tolerance was better for CT, but clinical improvement of hyperpigmentation was comparable.[28]
A second split-face trial with 23 patients compared CT with PRP once a week for four sessions. Follow-up was 3 months. In this trial, PRP showed significant better response, shorter downtime, and tolerable adverse events than CT. The area reduction of hyperpigmentation was on average 46.6% after PRP versus 14.3% after CT.[29]
A comparable split-face approach was used for POH in 21 patients from Iran. CT was performed by intradermal injection of 5 cm3 CO2 once weekly for 6 weeks. PRP treatment was performed every other week for 3 times. Both treatments resulted in a significant and comparable reduction of hyperpigmentation.[30]
A split-face trial compared CT (8 sessions) with CT (6 sessions) plus fractional CO2 laser (2 sessions) for facial rejuvenation in 25 female patients. All patients were satisfied with the outcome. There was no statistically significant difference between both treatments. However, texture and pigmentation were less improved by CT alone versus combined treatment.[31]
A split-face trial compared CT with fractional CO2 laser in 30 patients (mean age: 38.22 ± 8.3 years). After the second therapy session, patients’ satisfaction was remarkably better with laser therapy than CT. The clinical improvement rate was higher after the 2nd and 6th week in the laser group. There were no significant adverse events reported.[32]
HOW TO TREAT FOREHEAD AND GLABELLA
The injection needle must be inserted very superficial. The gas is administered in an antegrade manner. It is recommended to start the treatment following a line approximately 1–2 cm above the upper eyelid, from one side of the forehead to the other, with a distance between single injection points of approximately 3 cm. The procedure is repeated in cranial direction. The distance between the lines is also 3 cm. The treatment of the glabella starts by injecting the wrinkle from above and heading toward the radix [Figure 1]. Sometimes the upper eyelid gets filled in the inner corner and the gas seems to flow toward the nose.

- Glabellar injection.
HOW TO TREAT CHEEKS AND CHIN
The needle must be inserted very superficial. The gas is administered in an antegrade manner. Injections are parallel to the line of the face and mandible, the distance between single injection points is approximately 3–4 cm. This is followed by one injection along the outer lines of the zygomatic bone and one injection centrally into the cheek.
To elevate, drooping corners of the mouth injections are given approximately 1 cm below the corner of the mouth. The correction of the nasolabial fold requires two injections – in the middle of the nasolabial fold and above the corner of the mouth. The gas is administered in a retrograde linear manner [Figure 2].
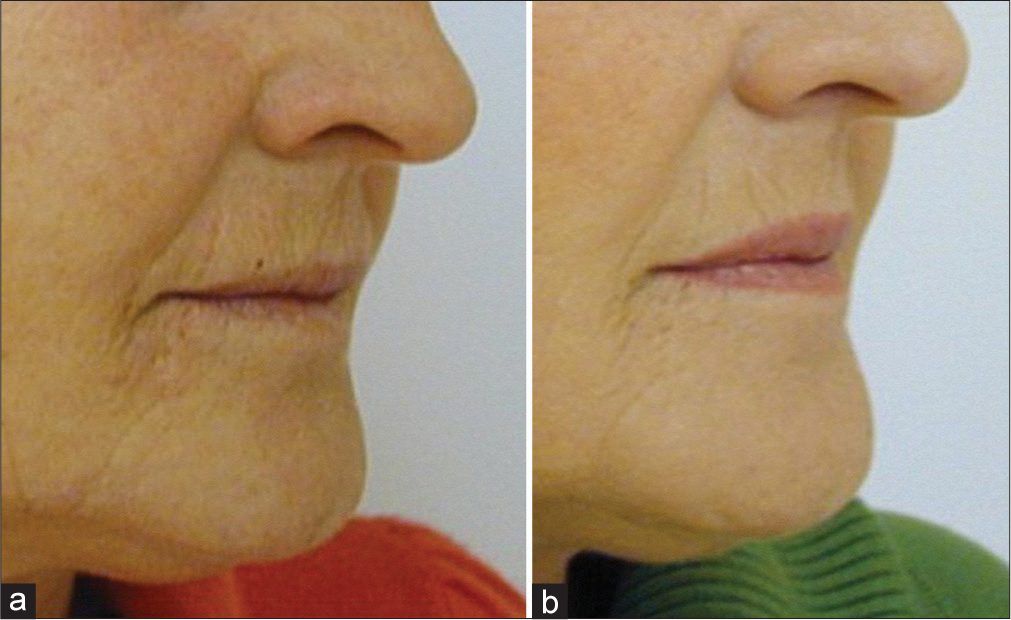
- Treatment to elevate drooping corners of the mouth. (a) before treatment, (b) after 4 carboxytherapy sessions.
The chin can be treated with one or two injections as well.
HOW TO TREAT DARK CIRCLES UNDER THE EYES
Injections into the zygomatic area and the lower eyelid must be very superficial. The gas is administered in an antegrade manner. It is recommendable to limit the number of injections to minimize tissue traumatization.
The treatment starts at the inner corner of the eye, approximately 1 cm below the lower eyelid and proceeds toward the outer corner of the eye. The distance between single injection points is 1–1.5 cm. Two to three lines are injected at a distance of 1 cm. Small papules develop thereby but resolve very quickly [Figure 3].
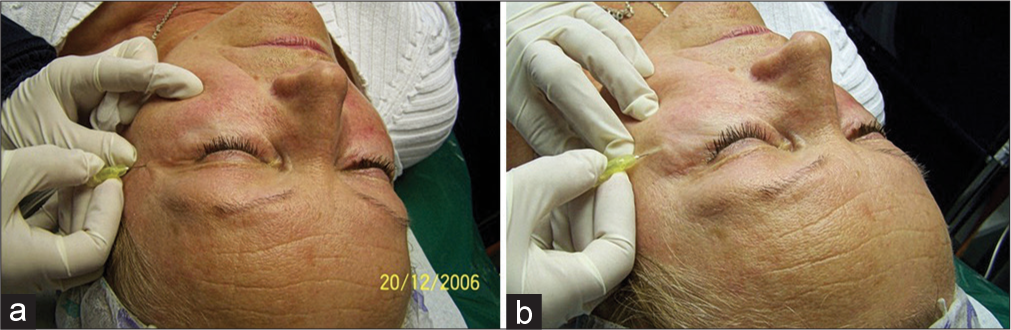
- Injection in the upper eyelid (a) and the lower eyelid (b).
Another approach is a linear antegrade technique approximately 1 cm below the lower eyelid, with one injection approximately 1 cm below the inner corner of the eye, the second injection below the outer corner of the eye, and the third one approximately 1.5 cm below in between the two injection points.
HOW TO TREAT THE NECK
The needle must be inserted very superficial at an angle of 15–30°, at a gas from flow of 5–10 mL/min. The length of the needle should be 4–6 mm. With the “popcorn” technique, small papules occur. Injections are made 2–3 cm apart at a flow rate of 5 mL/min in two to three lines approximately 3 cm from each other. The starting point is above the mastoid process, then it goes toward the clavicle.
With the “linear technique,” 2–3 injections are given directly into deep wrinkles. The length of the needle is 12 mm [Figure 4].[33]
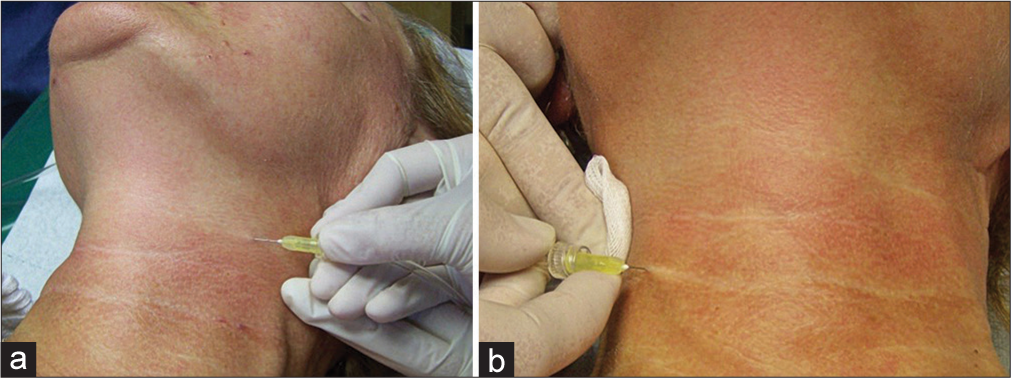
- Treatment of the neck with gas administration outside the wrinkle (a) and along the wrinkle (b).
HOW TO TREAT DOUBLE CHIN
The treatment aims to induce lipolysis of fat deposits and to improve skin tone. The area is quite small, requiring only 2–4 subcutaneous (subdermal) gas injections administered at the angle of 45° in an antegrade manner. The length of the needle is 12 mm with a flow rate of 5–10 mL/min.[33]
CT IN LOCALIZED ADIPOSITIES AND CELLULITE
Brandi et al. used CT (Carbomed programmable automatic CO2 therapy apparatus; Carbossiterapia Italiana S.R.L, Via Zanella, MI, Italy) with 30G 0.3 × 13-microlance needles for the subcutaneous application of CO2. They performed a trial on 42 patients with adipose tissue hypertrophy on the thighs and knees, either alone or as an adjunct to liposuction and observed a reduction of circumferences.[34]
Lee used CT with the same technology with a depth of infusion between 10 and 13 mm to improve abdominal irregularities (Cellulite) in 101 females and ten males, aged 20–50 years. The infusion was administered at a flow rate of 50–100 mL/min 2–4 times a month for at least five treatments. The infused volume was 500–1,000 mL for the abdomen and 800–1,000 mL for each thigh applied over 20–30 min. Circumferences and weight were measured before and during treatment in this retrospective single-center trial. Infraumbilical thickness of adipose tissue was also analyzed by ultrasound. Circumferences decreased by 1.1–2.6 cm on average. This corresponds to a weight loss between 0.9 kg and 1.6 kg. No safety issues were reported.[35]
In another prospective trial, ten women (mean age 29 ± 6.1 years) were treated with subcutaneous CT 8 times once a week for cellulite of the gluteal region and thighs.[36] Standardized digital photographs and ultrasound were used to assess the effects before and 1 week after cessation of CT. Body fat percentage was measured with Biodynamics (Model 310E; TBW, SP, Brazil). Injection depth was about 10 mm. They used an ARES Car-boxytherapy (IBRAMED, Indústria Brasileira de Equipamentos Médicos EIRELI, ANVISA 10360310032) equipment. The authors reported a significant decrease in severity of cellulite measured by the Nürnberger and Müller scale,[37] while body weight, body mass index, and percentage of body fat remained unchanged.
Eldsouky and Ebrahim investigated the efficacy of CT versus mesolipolysis with phosphatidylcholine (PPC) in the treatment of cellulite on thighs after 6 sessions once a week. Forty-eight female patients received either subcutaneous infusion of CT or mesolipolysis using PPC. Standardized photography and circumference measurements were performed before and after treatment with a follow-up of 6 months. Both cellulite grading and circumference decreased significantly without significant differences between both groups.[38]
In a randomized trial, 16 adults with a normal body mass index between 22 kg/m2 and 29 kg/m2 were treated with 5 weekly infusions of 1,000 cm3 of CO2 to one side of the abdomen and compared to 5 sham treatments on the other side. Circumference measurements and ultrasound measurements of abdominal adipose tissue were performed before and after treatment. While the thickness of the adipose tissue was reduced 1 week after treatment session, the effect was lost within 28 weeks. Circumference was reduced, but this did not reach statistical significance.[39]
Oliveira et al. investigated the effect of a single CT treatment on skin laxity. Nine patients were included in the study. They got a CT in the infraumbilical region with a flow rate (velocity) of 100 mL/min and 0.6 mL/kg weight over an area of 25 cm2. Sixty days later, a skin biopsy was taken for histological evaluation. There was a statistically significant increase in collagen on tissue sections but not elastic fibers.[40]
STRETCH MARKS AND SCARS
CT treatment fosters rejuvenation, lifting, and regeneration of connective tissue and stimulates the formation of new collagen. We use the “popcorn” technique (when small papules are formed) at first, with the needle inserted very superficial at an angle of 15–30°. At a flow, 5–10 mL/min CO2 gas is administered in an antegrade manner. The length of the needle should range from 4 mm to 6 mm. One injection is given every 3 cm along the finer stretch marks. The penetration of CO2 is very rapid. In the second stage, the more prominent, wider, and longer stretch marks are injected by a retrograde technique. The distance between single injection points depends on the length of the lesion. During a single treatment session, both techniques can be used, but it is recommended to use the one that fits best. The clinical effect on stretch mark appearance (redness and thickness) is good but stretch marks cannot completely be removed [Figure 5]. It is possible use of a comb applicator for larger areas [Figure 6].[33,41]

- Effect of injection carboxytherapy on a fresh hypertrophic scar: (a) Before treatment and (b) after five sessions – flattening of the lesion and complete remission of erythema.
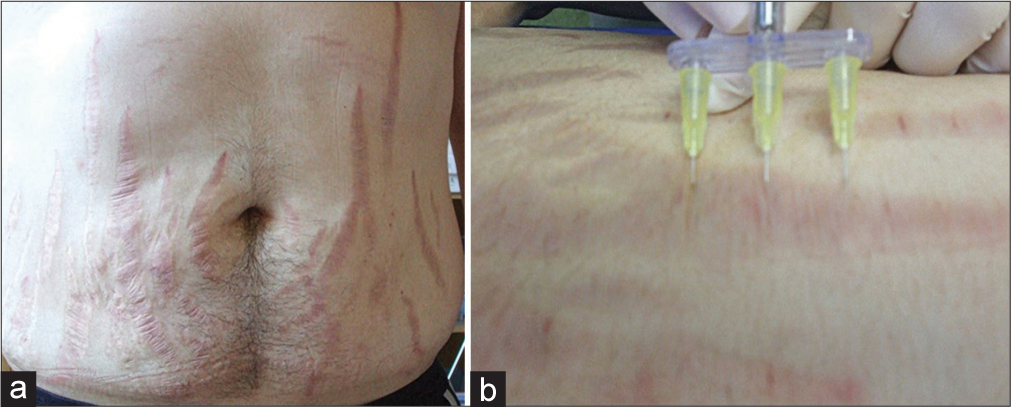
- Possible use of a comb applicator in stretch mark treatment. (a) Multiple abdominal stretch marks. (b) Use of a comb applicator.
In a prospective trial, 15 women (age 22–40 years) were treated for stretch marks with CT 3 time once a week. Assessment of the effects was realized by standardized photography and cutometry. CT significantly improved skin elasticity and visibility of lesions.[42]
In another study, 20 patients received eight sessions of CT injection (carboxy-gun) at 2-week intervals. Standardized 3D photography and skin biopsies were taken before and after 4 months of therapy. There was a significant clinical improvement combined with an increased epidermal thickness. Rete ridges reappeared, and histology demonstrated an improved organization of curled and fragmented elastic fibers. The collagen content increased.[43]
In a prospective trial, CT and PRP were compared for the treatment of stretch marks. Twenty patients with striae alba were included in the study. Half-side treatment with CT was done every 3–4 weeks (total four sessions), while PRP injections were performed contralateral. There was a significant clinical improvement in stretch marks for both treatments without significant differences between these methods. Histology demonstrated an increase in fibronectin-stained area.[44]
In a comparative trial for stretch marks with either CT, PRP, or tripolar RF (n = 45 females), all three procedures showed a significant improvement with a better patient’s satisfaction with CT or RF compared to PRP.[45]
A split body trial compared fractional CO2 laser with carboxytherapy for stretch marks (n = 30). Six sessions were performed once a month. The width of the striae decreased significantly with both approaches. Global esthetic improvement scale, satisfaction scale, and ultrasound measurements were in favor of CO2 laser versus CT.[46] CT seems to be effective in the improvement of atrophic acne scars although lesser than PRP with fractional CO2 laser.[47]
Another trial with either CT or fractional CO2 laser demonstrated comparable efficacy but different safety profiles. While the laser resulted more frequently in hyperpigmentation, CT caused more bruising.[48]
Hypertrophic scars and keloids represent an esthetic and mental problem and may severely limit patients at work and in social life. A scar that looks bad and limits the patient in any activity requires efficient therapy. An ideal scar is a scar that appears on the skin level and heals without visible manifestations, while a hypertrophic or keloid scar is elevated above the surrounding skin. Whenever CT is selected as a therapeutic modality, improved elasticity of the rigid scar tissue fibers and improved appearance of scars can be considered good effects in keloid scars.
The treatment may be carried out in one or two stages according to the size of the keloid scars:
One-phase treatment: CO2 is usually administered via intradermal injections directly into the scar. Two-phase treatment: The needle is inserted under the scar. The number of injections depends on the length of lesion. Positive effects occur after 5–8 treatment sessions, the recommended number of CT treatment sessions is 5–20. According to the sensitivity of the patient, it is possible to increase the flow rate of CO2. After the treatment, we recommend mild massage and silicone dressing applied overnight.
Atrophic scars are treated with the intradermal blanching technique. The onset of the effect is quite rapid, and the result looks good in most patients already after 4–8 treatment sessions. It is also possible to combine the treatment with the administration of PRP (once in 2–3 weeks).[33] CT showed a comparable efficacy in atrophic acne scar treatment as microneedling.[49]
A comparative trial in atrophic non-acne scars with either CT or PRP had been conducted in 40 patients. Each treatment was performed for four sessions once a month. Clinical improvement and patients satisfaction were better for CT than PRP. Histopathological examination demonstrated a significant expression of metalloproteinase-1 (CT > PRP).[50]
In a Polish study on scar treatment with CT, 12 mature scars were infused with heated, medical CO2 at a flow rate of 100 mL/min until the moment a scar turned white. They used the Carboxytherapy Dual MC4 device. The treatment was repeated 4 times every other week. There was a reduction in the size of lesions and an improvement in skin elasticity and hydration.[51]
CONCLUSION
The advantages of carboxytherapy in adequate indications are its versatility and safety. The action is selective, the technique is minimal invasive covering a very broad therapeutic range. The method is not expensive and thus very affordable for the patient. The disadvantage is the necessity to repeat the application to obtain the desired results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Karboxyterapie-nová neinvazivní metoda estetické medicíny [Carboxytherapy--a new non-invasive method in aesthetic medicine] Cas Lek Cesk. 2006;145:841-3.
- [Google Scholar]
- Carboxytherapy-a novel noninvasive method in aesthetic medicine. J Japan Soc Aesthet Surg. 2008;45:267-6.
- [Google Scholar]
- Transdermal CO2 application in chronic wounds. Int J Low Extrem Wounds. 2004;3:103-6.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide therapy in the treatment of localized adiposities: Clinical study and histopathological correlations. Aesthetic Plast Surg. 2001;25:170-4.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effects of carboxytherapy and radiofrequency on skin rejuvenation. J Cosmet Laser Ther. 2015;17:156-61.
- [CrossRef] [PubMed] [Google Scholar]
- Karboksiterapiia-odno iz innovatsionnykh napravlenii v kurortologii [Carboxytherapy-an innovative trend in resort medicine] Vopr Kurortol Fizioter Lech Fiz Kult. 2018;95:72-6.
- [CrossRef] [PubMed] [Google Scholar]
- Carboxytherapy as an alternative off lable method for diabetes mellitus treatment: A review. Pharmacol Online. 2021;1:447-55.
- [Google Scholar]
- Increase in collagen turnover induced by intradermal injection of carbon dioxide in rats. J Drugs Dermatol. 2008;7:201-6.
- [Google Scholar]
- Elevação da temperatura cutânea após a infusão controlada de dióxido de carbono [Increase of the skin temperature after infusion-controlled carbon dioxide] Rev Bras Cir Plást. 2009;24:257-61.
- [Google Scholar]
- Estudo angiográfico de fístula arteriovenosa utilizando gás carbônico como meio de contrante [Arteriovenous fistula angiography using carbon dioxide as contrast medium] Radiol Bras. 2004;37:397-403.
- [CrossRef] [Google Scholar]
- Carboxytherapy-induced fat loss is associated with VEGF-mediated vascularization. Aesthetic Plast Surg. 2018;42:1681-8.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of the role of carboxytherapy in dermatology. J Cosmet Dermatol 2023 doi: 10.1111/jocd.15741
- [CrossRef] [PubMed] [Google Scholar]
- The antioxidant action of CO2-one of the universal mechanisms of carboxytherapy. Pharmacol Online. 2021;2:158-66.
- [Google Scholar]
- Vasomotor effects of transcutaneous CO2 in stage II peripheral occlusive arterial disease. Angiology. 1995;46:785-91.
- [CrossRef] [PubMed] [Google Scholar]
- The mechanism of action of carboxytherapy. Pharmacol Drug Toxicol. 2016;6:12-20.
- [CrossRef] [Google Scholar]
- Staged combined therapy of poor healing lower leg wounds due to chronic venous insufficiency. J Clin Cell Immunol. 2016;7:33.
- [Google Scholar]
- Carboxytherapy-a non-invasive method in aesthetic medicine and dermatology, and the combined usage of carboxytherapy and PRP in the periorbital area. Glob Dermatol. 2017;4:1-5.
- [CrossRef] [Google Scholar]
- Effects of transcutaneous electrical nerve stimulation on pain intensity during application of carboxytherapy in patients with cellulite: A randomized placebo-controlled trial. J Cosmet Dermatol. 2018;17:1175-81.
- [CrossRef] [PubMed] [Google Scholar]
- Massive subcutaneous emphysema after carbon dioxide mesotherapy. Aesthetic Plast Surg. 2013;37:194-7.
- [CrossRef] [PubMed] [Google Scholar]
- Post periorbital carboxytherapy orbital emphysema: A case report. Orbit. 2022;41:123-6.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized comparative study of the effect of two different flow rates of carboxytherapy in the treatment of infraorbital dark circles. J Cosmet Dermatol. 2022;21:4020-7.
- [CrossRef] [PubMed] [Google Scholar]
- Infections à mycobactéries atypiques liées à des soins esthétiques en France, 2001-2010 [Non-tuberculous mycobacterial infections related to esthetic care in France, 2001-2010] Med Mal Infect. 2011;41:379-83.
- [CrossRef] [PubMed] [Google Scholar]
- Periorbital area rejuvenation using carbon dioxide therapy. J Cosmet Dermatol. 2012;11:223-8.
- [CrossRef] [PubMed] [Google Scholar]
- Objective, measurable assessment of the elasticity of the skin around the eyes following the carboxytherapy treatment. J Cosmet Dermatol. 2023;22:1560-4.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of radiofrequency, intense pulsed light and carboxytherapy in facial rejuvenation. J Cosmet Laser Ther. 2020;22:256-64.
- [CrossRef] [PubMed] [Google Scholar]
- Carboxytherapy, subcutaneous injections of carbon dioxide in the management of infraorbital dark circles: A reliable and effective procedure. J Craniomaxillofac Surg. 2021;49:670-4.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of carboxytherapy and platelet-rich plasma in treatment of periorbital hyperpigmentation: A comparative clinical trial. J Cosmet Dermatol. 2018;17:1000-7.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma versus carboxytherapy in the treatment of periorbital dark circles: A split-face study. J Cosmet Dermatol. 2022;21:4332-8.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma versus carboxytherapy for the treatment of periocular hyperpigmentation; which approach is superior? Dermatol Ther. 2021;34:e14980.
- [CrossRef] [Google Scholar]
- The use of carboxytherapy alone or in combination with fractional CO2 laser for facial rejuvenation: A split-face comparative study. J Cosmet Dermatol. 2020;19:1648-55.
- [CrossRef] [Google Scholar]
- Comparison of the efficacy of carboxytherapy versus fractional CO2 laser therapy for the treatment of periorbital dark circles: A randomized clinical trial. J Cosmet Dermatol. 2023;22:512-6.
- [CrossRef] [PubMed] [Google Scholar]
- Carboxytherapy In: New Findings. Bratislava: Vydavatelstvo Publishing House Anna Nagyova; 2019.
- [Google Scholar]
- Carbon dioxide therapy: Effects on skin irregularity and its use as a complement to liposuction. Aesthetic Plast Surg. 2004;28:222-5.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide therapy in the treatment of cellulite: An audit of clinical practice. Aesthetic Plast Surg. 2010;34:239-43.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of carboxytherapy in the treatment of cellulite in healthy women: A pilot study. Clin Cosmet Investig Dermatol. 2016;9:183-90.
- [CrossRef] [PubMed] [Google Scholar]
- So-called cellulite: An invented disease. J Dermatol Surg Oncol. 1978;4:221-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and efficacy of carbon dioxide therapy (carboxytherapy) versus mesolipolysis in the treatment of cellulite. J Cosmet Laser Ther. 2018;20:307-12.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous infiltration of carbon dioxide (carboxytherapy) for abdominal fat reduction: A randomized clinical trial. J Am Acad Dermatol. 2018;79:320-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of carboxytherapy on skin laxity. J Cosmet Dermatol. 2020;19:3007-13.
- [CrossRef] [PubMed] [Google Scholar]
- Striae cutis distensae and the therapeutic opportunities. Kosmet Med. 2010;31:140-5.
- [Google Scholar]
- Cutometric assessment of elasticity of skin with striae distensae following carboxytherapy. J Cosmet Dermatol. 2018;17:1170-4.
- [CrossRef] [PubMed] [Google Scholar]
- Carboxytherapy for striae distensae: A promising modality. J Cosmet Dermatol. 2021;20:546-53.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and immunohistochemical comparative study of the efficacy of carboxytherapy vs platelet-rich plasma in treatment of stretch marks. J Cosmet Dermatol. 2018;17:1008-15.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study between: Carboxytherapy, platelet-rich plasma, and tripolar radiofrequency, their efficacy and tolerability in striae distensae. J Cosmet Dermatol. 2019;18:788-97.
- [CrossRef] [PubMed] [Google Scholar]
- Split body comparative clinical and radiological study of fractional CO2 laser versus carboxytherapy in treatment of striae distensae. Dermatol Ther. 2022;35:e15668.
- [CrossRef] [Google Scholar]
- Comparative study of the efficacy of platelet-rich plasma combined with carboxytherapy vs its use with fractional carbon dioxide laser in atrophic acne scars. J Cosmet Dermatol. 2019;18:150-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser versus carboxytherapy in treatment of striae distensae. Lasers Surg Med. 2021;53:1173-9.
- [CrossRef] [PubMed] [Google Scholar]
- Carboxytherapy versus skin microneedling in treatment of atrophic postacne scars: A comparative clinical, histopathological, and histometrical study. Dermatol Surg. 2018;44:1332-41.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of platelet-rich plasma vs carboxytherapy in the treatment of atrophic scars: A comparative clinical and histopathological study. Dermatol Ther. 2020;33:e13942.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of carboxytherapy on scar reduction. Clin Cosmet Investig Dermatol. 2022;15:2855-72.
- [CrossRef] [PubMed] [Google Scholar]







