Translate this page into:
Breaking out of acne beyond the face – A closer look at truncal acne

*Corresponding author: Hiba Fathimathul Harshiba, Department of Medicine, Tbilisi State Medical University, Tbilisi, Georgia. drhibabasheerofficial@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Fathimathul Harshiba H, Muhammed Rafi N, Asif S, Ahmad H, Korrapati N, Thangamuni A, et al. Breaking out of acne beyond the face – A closer look at truncal acne. CosmoDerma 2023;3:156.
Abstract
This article discusses truncal acne, a skin condition that is frequently misdiagnosed and disregarded since it affects the trunk of the body. While facial acne is commonly addressed and treated, truncal acne can also have significant physical and psychological effects on those who are affected. The purpose of this article is to provide information on the illness, its signs, causes, risk factors, diagnosis, and possible treatments. This paper also explores the psychological and societal repercussions of truncal acne and how it affects self-esteem and body image. In addition, it examines patient education and support for this ailment, highlighting the need for prompt and efficient treatment in enhancing patients’ quality of life. This article aims to explore truncal acne comprehensively, highlighting the need for early prevention and treatment. It is hoped that this article will serve as a foundation for future studies on truncal acne, leading to a better understanding and management of the condition.
Keywords
Truncal acne
Back acne
Breast acne
Acne
Facial acne
INTRODUCTION
Acne is a common skin ailment that can affect individuals of all ages, resulting in papules, pustules, skin discoloration, and scarring. Truncal acne is a subtype that appears on the chest, back, and belly. It is often concealed by clothing, which can cause individuals affected by it to remain unaware of their condition.[1] This can lead to discomfort and scarring if left untreated.[2] Hormonal imbalances, stress, poor diet, genetics, and environmental factors, have all been linked to the development of truncal acne.[3] Treatment includes topical medications such as retinoids, benzoyl peroxide (BPO), antibiotics, hormone therapies, and lifestyle adjustments such as trigger identification, a healthy diet, and regular exercise.[4] The aim of this article is to provide a comprehensive overview of truncal acne, including its clinical features, pathogenesis, diagnosis, and treatment.
MATERIALS AND METHODS
To gather data, a literature search was conducted across PubMed and Google Scholar using the keywords “acne,” “truncal acne,” “chest acne,” “breast acne,” “shoulder acne,” and “acne vulgaris.” Articles were taken from various English language journals published in the period of 2012–2022. The search was conducted from November 2022 to March 2023. It included clinical trials, meta-analyses, randomized controlled trials, observational studies, and reviews. Articles not relevant to trunk or chest acne were excluded from the study.
RESULTS
In our extensive literature search, we gathered data from 29 scholarly articles. Our findings from the articles are compiled in Table 1.
| Author | Study | Findings |
|---|---|---|
| Melnik et al., 2007 | Review Article | Sebocytes and follicle keratinocytes express receptors for androgens as well as other hormones |
| Bikowski, 2010 | Review | BPO 5.3% foam safe and effective for truncal acne |
| Sharquie et al., 2012 | Cross-sectional, out-patient-based study |
Malassezia responds to antifungal therapy while truncal acne is unresponsive to antifungal therapy |
| Palli et al., 2013 | Randomized double-blind clinical trial (single-center) | OC containing drospirenone/EE improves moderate truncal acne |
| Koo et al., 2014 | Meta-analysis | Antibiotics and OCPs both significantly reduce acne lesions. However, after 3 months, antibiotics outperform OCPs in terms of lowering the overall lesions. |
| Webster et al., 2014 | Phase III clinical trial (double-blind) | Isotretinoin is effective for severe nodular acne |
| Ravisankar et al., 2015 | Article | Neglected truncal acne and its need for attention |
| Kim et al., 2015 | Observational | Lower sebum levels on the trunk than face in women; no correlation between truncal sebum and acne |
| Asai et al., 2016 | Guideline | Recommendations for treating comedonal, mild-to-moderate papulopustular, and severe acne |
| Yew et al., 2016 | Clinical Trial | PDT with 5-ALA is effective for truncal acne |
| Zaenglein et al., 2016 | Guideline | Guidelines for acne treatment, including truncal acne |
| Abanmi et al., 2016 | Review Article | Factors for truncal acne development |
| Gollnick et al., 2017 | Review Article | Truncal acne treatment |
| Liu and Tan 2017 | Review Article | CASS guides therapy for facial and truncal acne, Treatment recommendations |
| Nguyen and Tollefson, 2017 | Review Article | Increased androgen secretion such as that in PCOS, Cushing syndrome, or tumors is thought to contribute to the worsening of truncal acne by progestin contraceptives and IUDs, although no clear connection has been demonstrated |
| Kazandjieva and Tsankov, 2017 | Review Article | Increased androgen secretion conditions are thought to contribute to the worsening of acne |
| Castillo and Keri, 2018 | Review Article | Despite the lack of evidence supporting their efficacy for truncal acne, chemical peels are routinely utilized in clinical practice |
| Bosanac et al., 2018 | Review | Progestins may worsen acne, especially hormonal acne in women |
| Del Rosso et al., 2019 | Review | Review of truncal acne prevalence, pathogenesis, and treatment |
| Poli et al., 2020 | Review Article | Recommendations for better management considering the lesion progression. |
| Armstrong et al., 2020 | Systematic Review | Oral tetracyclines are effective for inflammatory acne vulgaris but not to be used as monotherapy due to antibiotic resistance concerns |
| Tan et al., 2021 | Review Article | Unsatisfied with current guidelines on truncal acne, benefits of having female nurses, teledermatology |
| Tan et al., 2021 | Modified Delphi Approach | Emphasizing the need for early diagnosis, tailored treatment plan, and recommendations |
| Leung et al., 2021 | Review Article | Acne causes follicular hyperkeratosis and activates immune system components |
| Woo and Kim 2022 | Review Article | Misdiagnosis and inadequate treatment of truncal acne, its impact on quality of life, factors contributing to its severity, and the importance of distinguishing it from other trunk lesions. |
| Tan et al., 2022 | Review Article | Comedones, cysts, and scarring are less prevalent in steroid folliculitis than they are in acne vulgaris. After the inflammation subsides, however, hyperpigmentation may develop |
| Daniele et al., 2023 | Review Article | Importance of distinguishing truncal acne from other disorders |
| Greco, 2023 | Article | Truncal acne often neglected due to its location |
PDT: Photodynamic therapy, CASS: Comprehensive acne severity scale, PCOS: Polycystic ovarian syndrome, 5-ALA: 5 Aminolevulinic acids, IUDs: Intrauterine devices, OCPs: Oral contraceptive pills, OC: Oral contraceptive, EE: Ethinyl estradiol, BPO: Benzoyl peroxide
DISCUSSION
Truncal acne is often misdiagnosed and treated such as facial acne, leading to inadequate reporting, and treatment.[5] Untreated truncal acne can cause painful deep lesions due to increased contact with clothing.[6]
In the PACE study,[6] a panel of 13 dermatologists used a modified Delphi approach to reach a consensus on truncal acne diagnosis and treatment. Most reported that only a few of their patients had truncal acne alone, while nearly half had combined facial and truncal acne. All dermatologists claimed that their patients were reluctant to expose truncal acne and rather preferred to talk about their facial acne. As a result, all the dermatologists who took part in the study concurred that recommendations are needed for doctors to encourage patients to talk about truncal acne without hesitation.
Severe truncal acne can greatly affect the quality of life, causing body image issues, low self-confidence, and negative impacts on daily activities and mental well-being.[5] Limitations to understanding truncal acne include time constraints during consultations, a focus on treating facial acne, and a hesitance to expose the truncal area.[7] To overcome these, female nurses can be present during consultations with male practitioners to protect patient privacy and encourage openness about their condition. Teledermatology can also help by reducing physical exposure. Implementing these recommendations is crucial for better management of truncal acne, considering the high number of unreported cases and the need for advancements in medical treatments. Equal attention and focus on truncal acne, alongside facial acne, can improve patient outcomes and quality of life.[8]
EPIDEMIOLOGY
Comparable rates of truncal acne were seen in both sexes.[9] Adults are not immune to getting acne, despite popular belief. According to Tan et al.,[6] truncal acne tends to manifest earlier and be more severe than other forms of acne. Table 2 provides more information on epidemiology and risk factors.[10]
| Epidemiology and Risk Factors | Reasons |
|---|---|
| AGE | Risk increases with onset of pubertal age. 12-24 years of age – 85%. Not limited to adolescence and by age 50, both men and women will still have acne. (5% of them at least). |
| RACE & HERITAGE | North American whites , African Americans as well as ethnicities with darker skin. |
| SEX | Adolescence : common in male. Adulthood : common in female. Men are marginally more likely to be to be affected than women. |
| REPRODUCTIVE FACTORS | Pubertal age when more androgens are released. Pregnancy. |
| OBESITY | Elevated IGF-I and androgen levels. |
| PRE EXISTING ACNE | Individuals suffering from facial acne also suffer from truncal acne – 48-52%. |
| ENVIRONMENTAL INFLUENCES | Diet, meat, fruits and vegetables, dairy, caffeine and alcohol, irradiation, hypertension, diabetes, infection and stress. |
Epidemiology and risk factors. Adapted from Rao J.[28]
PATHOPHYSIOLOGY
Acne commonly occurs due to excessive sebum production and/or imbalances in the skin and gut flora. Increased androgen levels during adolescence are linked to the development of acne, suggesting that human hormones influence the pilosebaceous unit’s biological activity. Sebocytes and follicle keratinocytes express receptors for androgens as well as other hormones.[11]
Staphylococcaceae and Propionibacteriacea are the most common bacteria responsible for face acne, whereas Enterococcaceae are primarily responsible for truncal acne.[5] Truncal acne may be influenced by the mycobiota of some fungi.[5] Acne has recently been shown to cause follicular hyperkeratosis and activate immune system components [Figure 1].[12]
![Pathogenesis of truncal acne. Adapted from Rao J.[28]](/content/130/2023/3/1/img/CSDM-3-156-g001.png)
- Pathogenesis of truncal acne. Adapted from Rao J.[28]
Increased androgen secretion, such as that in polycystic ovarian syndrome, cushing syndrome, or tumors, is thought to contribute to the worsening of truncal acne by progestin contraceptives and intrauterine devices (IUDs), although no clear connection has been demonstrated.[5,13,14]
Patients with truncal acne had their sebum secretion measured at both facial and truncal sites in a study by Kim et al., but no significant association was found between sebum production and breakouts on the trunk, suggesting that additional variables may play a more significant role in the onset of truncal acne.[15] According to a recent study, those who used subdermal implanted contraceptives with etonogestrel or levonorgestrel were more likely to experience acne breakouts in contrast to those who used a nonhormonal copper IUD.[16]
CLINICAL FEATURES
Truncal acne often manifests on the upper back, upper chest, lower back, shoulders, upper limbs, and neck as non-inflammatory breakouts or inflammatory papules, pustules, and nodules. Acne lesions typically progress through four stages: Microcomedones, comedones, inflammatory papules or pustules, and nodulocystic acne [Figure 2].[8] Microcomedones are the earliest stages of acne lesions. Comedones develop into erythematous papules and pustules as they grow more inflammatory. Deep pustules, nodules, and/or cysts may form when it is severe [Figure 3].[5]
![Clinical features of truncal acne. Adapted from Woo and Kim.[5]](/content/130/2023/3/1/img/CSDM-3-156-g002.png)
- Clinical features of truncal acne. Adapted from Woo and Kim.[5]
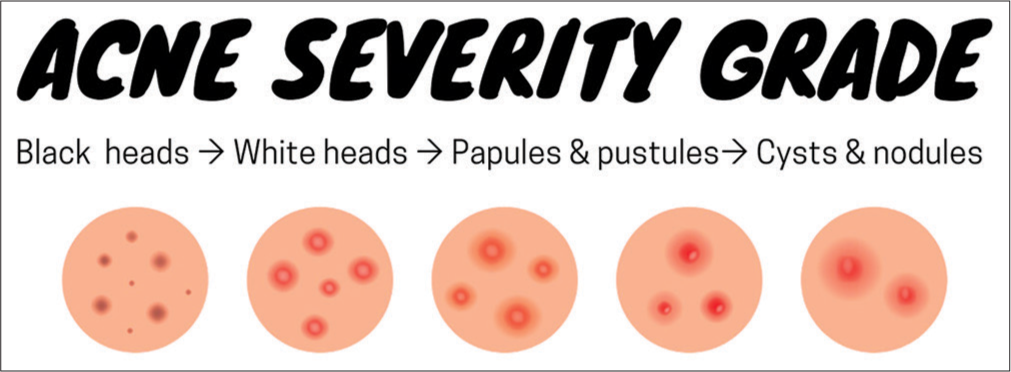
- Acne severity grade: It ranges from mild-to-moderate-to-severe, respectively, Illustrated by Asif S.
According to Sharquie et al., Malassezia folliculitis is a hair follicle infection that occurs commonly in men whereas truncal acne is more common in women.[17] Truncal acne lesions may be more inflammatory and severe than facial lesions.[18] Young adults with trunk papulopustular eruptions may have Malassezia folliculitis, which may be distinguished from truncal acne by its clinical and histological characteristics.[17]
ASSESSMENT
Although many different acne grading scales have been created, none of them are recommended for widespread use. Acne severity should be evaluated based on several characteristics including, the kind of lesion, its size, distribution, and the existence of scars or dyspigmentation. To get a full picture of the situation, the patient’s face, chest, and back should be evaluated during the physical examination.
Unless there is a clear clinical indication, laboratory tests are unnecessary. Bacterial folliculitis, acneiform drug eruptive events, and other disorders should all be distinguished from acne. The location of lesions, size, and location determine acne severity. Women of reproductive age can have their hormone levels tested for hyperandrogenism, and a pelvic ultrasound can be used to screen for polycystic ovary syndrome.[12]
The comprehensive acne severity scale, which may be used separately for the face, chest, and back, is one example of a grading system that has been authorized for use with facial and truncal acne [Table 3].[19]
| Category | Description |
|---|---|
| Clear | From completely symptom-free to somewhat afflicted. Comedones and papules are quite rare. |
| Almost clear | The difference is marginal at 2.5 m. Comedones, little papules, and barely any pustules are dispersed over the skin. |
| Mild | Easily identifiable, with less than half of the target region impacted. There are a lot of bumps and pimples on your skin. |
| Moderate | Involvement of more than half the impacted area. Acne, papules, and pustules proliferate in large numbers. |
| Severe | There is a regional impact. Plagued by comedones, along with a plethora of other skin lesions. |
| Very severe | Acne with severe inflammation, including nodules and cysts, covers the afflicted region. |
DIFFERENTIAL DIAGNOSIS
It is vital to recognize the differences between truncal acne and other papulopustular lesions on the trunk. Pityrosporum folliculitis is a skin ailment commonly misdiagnosed as truncal acne. It affects the trunk, neck, and upper arms and is characterized by pruritic, monomorphic, small follicular papules and pustules, with or without perifollicular erythema. It can be distinguished from truncal acne by its lack of comedones, its resistance to topical and oral medicines, and the presence of irritating skin sores.[5]
Medications such as glucocorticoids, phenytoin, lithium, isoniazid, high-dose Vitamin B complex, halogenated compounds, cyclosporine, epidermal growth factor receptor inhibitors, and BRAF inhibitors can all lead to acneiform eruptions, which doctors always consider when diagnosing truncal acne.[5]
Acneiform eruptions caused by drugs typically appear as a diffuse homogeneous rash of follicular papules on the trunk. However, several weeks after continuous steroid use, inflammatory papules and pustules appear on the upper arms, shoulders, and trunk, a condition known as steroid folliculitis. Comedones, cysts, and scarring are less prevalent in steroid folliculitis than they are in acne vulgaris. Although, hyperpigmentation may develop after the inflammation subsides.[20]
TREATMENT
More than 75% of individuals with facial acne desire therapy for their truncal acne since it might cause scarring. Acne may have a devastating effect on some parts of the body, but scarring can be avoided with early diagnosis and tailored treatment plans. Decisions on therapy should be based on the patient’s illness burden.[6] Table 4 provides summary of treatment options.
| Treatment type | Examples | Properties | Recommendations |
|---|---|---|---|
| Topical therapy | Retinoids, benzoyl peroxide, and azelaic acid cream | Antibacterial, anti-inflammatory, and anti-hyperkeratinization properties | Acne of the truncal region is treated first. This therapy option can stand alone or be combined with other topical treatments. |
| Dapsone | Medication that reduces inflammation and is useful for treating papules and pustules. |
||
| Topical and oral antibiotics | Antibacterial properties, reduce inflammation, and hyperkeratinization processes. | Controlling Propionibacterium acnes using topical antibiotics like erythromycin and clindamycin is possible, but not advised due to the risk of bacterial resistance. Combinations with other topical treatments using clindamycin are common. Individuals with mild-to-severe acne should only take oral antibiotics for the shortest time possible. |
|
| Systemic therapy | Tetracyclines | First-line antibiotics with antibacterial properties | To reduce the likelihood of bacteria becoming resistant, treatment durations should be short (no more than 3–4 months). Pregnant women, those with allergies, and children younger than 8 years old should not use tetracyclines. Due to the possibility of narcotic-induced hepatitis and lupus, minocycline should be used when other therapies are available. Because of the possibility of antibiotic resistance, erythromycin is not recommended. We do not know enough about the efficacy and risk of bacterial resistance to prescribe any other antibiotics currently. |
| Erythromycin, azithromycin, and other macrolide antibiotics | Antibacterial agents as a second line of defense | The potential of bacterial resistance makes erythromycin a poor choice, although it can be administered when tetracyclines are not an option. |
|
| Hormonal therapy | COCs | Anti-androgenic effects through negative feedback mechanisms | Can be used by females with inflammatory acne who want to use contraception, but not advised for pregnant women, heavy smokers, women over 35, or those with migraines, hypertension, diabetes, or a history of DVT/PE. Better First line in long-term therapy for women than Antibiotics. |
| Spironolactone | Antiandrogenic properties with limited high-quality evidence |
||
| Oral isotretinoin | Isotretinoin | Reduces inflammation, hyperkeratinization, bacterial growth, and sebum production. | Physicians and female patients who might become pregnant should adhere to the criteria established by the pregnancy prevention program, even though the treatment is suggested for moderate-to-severe acne and those refractory to alternative medications. Should not be used by nursing mothers. |
| Procedural therapies | LEDs, light-emitting devices, Treatments such as chemical peels (including salicylic acid, glycolic acid, lactic acid, mandelic acid, retinoic acid, trichloroacetic acid, Jessner’s |
Limited research on the effectiveness of truncal acne, may cause skin irritation or scarring | Consider severe or refractory acne, which may require a multidisciplinary approach. |
| PDT | solution, kojic acid, pyruvic acid, azelaic acid, and combination peels), Injections given under guidance 5-Aminolevulinic acid topical solution (5%). |
Proven to reduce the number of inflamed and uninflamed lesions in Asian individuals with truncal acne | Consider for truncal acne, especially for inflammatory lesions, may require further studies in other populations |
PDT: Photodynamic therapy, COCs: Combined oral contraceptives, DVT: Deep venous thrombosis, PE: Pulmonary embolism, LEDs: Light-emitting diodes
The four processes that cause acne – sebum generation, bacterial colonization, ductal blockage, and inflammation – should all be addressed in the course of treatment. Therapeutic combinations are sometimes the most efficient treatment options. Truncal acne treatment options are determined by the patient’s clinical condition, its severity, their medical history, and their personal preferences.
Common acne antibiotics include oral tetracyclines.[21] Patients can avoid tight-fitting clothing, reducing perspiration, and keep up with regular hygiene routines to reduce the severity of truncal acne.[6] The following treatment recommendations are based on the latest recommendations for acne care and contain helpful guidance.[19]
TOPICAL THERAPY
When treating minor truncal acne, topical treatment is the best course of action. Retinoids, BPO, azelaic acid, dapsone, and antibiotics are some examples of effective topical treatments. These drugs can delay hyperkeratinization and have antibacterial and anti-inflammatory effects. Dapsone heals papules and pustules, while azelaic acid lessens acne and hyperpigmentation. Due to probable bacterial resistance, topical erythromycin and clindamycin are not advised as monotherapies.[19] Truncal acne vulgaris can be successfully treated with BPO (5.3%) emollient foam, particularly when used in conjunction with other treatments. It is extremely bioavailable and highly powerful against Propionibacterium acnes, and has a skin-friendly formulation.[22] Truncal acne can be effectively treated with a topical lotion that contains mineral oil, glycerin, soluble collagen, sodium hyaluronate, and tretinoin (0.05%). Topical tretinoin (0.05% lotion) and azelaic acid (15%) foam should be applied twice daily for best effects. Asian people with truncal acne may benefit from photodynamic therapy (PDT) with 5% topical 5-aminolevulinic acid (ALA).[23]
SYSTEMIC THERAPY
Moderate-to-severe acne as well as acne with inflammation may require systemic care when topical therapies fail. Antibiotics, isotretinoin oral contraceptives, or spironolactone may be prescribed in addition to topical or systemic treatments in such circumstances.[24]
Shorter treatments (no more than 3–4 months total) are preferable to avoid the development of bacterial resistance. Although tetracyclines are commonly used, minocycline should be avoided due to the risk of side effects. Those who are allergic, pregnant, or <8 years old have the option of using macrolides as a second-line therapy option. However, because of the danger of bacterial resistance, erythromycin should not be used. Due to the lack of data on the efficacy and resistance potential of other antibiotics, they are not advised.[19] Isotretinoin is the medication of choice for treating severe, long-lasting acne on the body’s trunk.[25]
HORMONAL THERAPY
In women with inflammatory acne, combined oral contraceptives have anti-androgenic benefits, although they are not advised for pregnant women, heavy smokers, people over 35, those with migraines, high blood pressure, diabetes, or a history of deep venous thrombosis or pulmonary embolism. Despite being used often, there isn’t much support for spironolactone’s antiandrogenic efficacy.[19] A combination of 3 mg drospirenone and 0.02 mg ethinylestradiol, when administered to 25 people with mild trunk acne, demonstrated success rates of 53.3% [investigator global assessment (IGA)] and 60% [subject global assessment (SGA)] at 24 weeks, indicating clinical improvement and good tolerability. The anti-mineralocorticoid and anti-androgenic characteristics of drospirenone can aid in acne management.[26] According to a meta-analysis of 32 randomized controlled studies, antibiotics and oral contraceptive pills (OCPs) both significantly reduce acne lesions. However, after 3 months, antibiotics outperform OCPs in terms of lowering the overall lesions.[27]
ORAL ISOTRETINOIN
Isotretinoin reduces sebum production, bacterial growth, inflammation, and hyperkeratinization.[28] Even though it’s prescribed for severe or treatment-resistant acne, pregnancy prevention guidelines must be followed by female patients and prescribers due to its teratogenic effect. It is not recommended for breastfeeding women.[19] Isotretinoinlidose, a newer form of isotretinoin, has 50% higher bioavailability due to micronized particles. In a 20-week study of 925 severe nodular acne patients, isotretinoin-lidose and traditional isotretinoin showed equal effectiveness in reducing nodules on the face and trunk.[14]
PROCEDURAL THERAPIES
Procedural therapy such as peels with chemicals, lasers, and injections may be necessary to treat truncal acne. Salicylic acid, glycolic acid, lactic acid, mandelic acid, retinoic acid, trichloroacetic acid, Jessner’s solution, kojic solution, pyruvic solution, azelaic solution, and combinations of these acids have all been used in chemical peels. Despite the lack of evidence supporting their efficacy for truncal acne, chemical peels are routinely utilized in clinical practice.[29] Research on 15 Asian patients with truncal acne treated with PDT and with 5% 5-ALA found that both inflammatory and non-inflammatory lesion counts decreased significantly after a single PDT session and 12 weeks of follow-up.[23]
CONCLUSION
Truncal acne can result in scarring and other major health problems if it is left undetected and untreated. A holistic approach that considers physical and psychological factors is necessary for effective management. There are several treatment possibilities, including combination therapy, hormone therapy for women, and topical and systemic medicines. Ensuring a comfortable atmosphere during appointments and using teledermatology can encourage reporting as well as improve the management of cases. Education and improved patient-practitioner communication are also needed.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Review sheds light on understudied truncal acne vulgaris. 2023. Yale School of Medicine. Available from: https://medicine.yale.edu/news-article/review-sheds-light-onunderstudied-truncal-acne-vulgaris [Last accessed on 2023 Oct 04]
- [Google Scholar]
- Acne-causes and amazing remedial measures for acne. Indo Am J Pharm Res. 2015;5:2512-22.
- [Google Scholar]
- Progress and problems with acne management in the Middle East. Gulf J Dermatol Venereol. 2016;23:1-7.
- [Google Scholar]
- Managing acne in the Middle East: Consensus recommendations. J Eur Acad Dermatol Venereol. 2017;31:4-35.
- [CrossRef] [PubMed] [Google Scholar]
- Gaps and recommendations for clinical management of truncal acne from the Personalising Acne: Consensus of Experts panel. JAAD Int. 2021;5:33-40.
- [CrossRef] [PubMed] [Google Scholar]
- A new era for truncal acne: Emerging from a legacy of neglect. Dermatol Ther (Heidelb). 2021;11:665-8.
- [CrossRef] [PubMed] [Google Scholar]
- Truncal acne, what do we know? J Eur Acad Dermatol Venereol. 2020;34:2241-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of acne: Canadian clinical practice guideline. CMAJ. 2016;188:118-26.
- [CrossRef] [PubMed] [Google Scholar]
- Acne Vulgaris. 2022. Medscape. Available from: https://emedicine.medscape.com/article/1069804-overview [Last accessed on 2023 Oct 04]
- [Google Scholar]
- Abuse of anabolic-androgenic steroids and bodybuilding acne: An underestimated health problem. J Dtsch Dermatol Ges. 2007;5:110-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatology: How to manage acne vulgaris. Drugs Context. 2021;10:1-18.
- [CrossRef] [PubMed] [Google Scholar]
- Endocrine disorders and hormonal therapy for adolescent acne. Curr Opin Pediatr. 2017;29:455-65.
- [CrossRef] [PubMed] [Google Scholar]
- Sebum secretion of the trunk and the development of truncal acne in women: Do truncal acne and sebum affect each other? Dermatology. 2015;231:87-93.
- [CrossRef] [PubMed] [Google Scholar]
- Progestins and acne vulgaris: A review. Dermatol Online J. 2018;24:13030/qt6wm945xf.
- [CrossRef] [Google Scholar]
- Malassezia folliculitis versus truncal acne vulgaris (clinical and histopathological study) J Cosmet Dermatol Sci Appl. 2012;2:277-82.
- [CrossRef] [Google Scholar]
- Truncal acne and scarring: A comprehensive review of current medical and cosmetic approaches to treatment and patient management. Am J Clin Dermatol. 2023;24:199-223.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding truncal acne: A practical guide to diagnosis and management. Skin Ther Lett. 2017;12
- [Google Scholar]
- Prevalence and demographics of truncal involvement among acne patients: Survey data and a review of the literature. J Clin Aesthet Dermatol. 2022;15:62-7.
- [Google Scholar]
- Oral tetracyclines and acne: A systematic review for dermatologists. J Drugs Dermatol. 2020;19:s6-13.
- [Google Scholar]
- A review of the safety and efficacy of benzoyl peroxide (5.3%) emollient foam in the management of truncal acne vulgaris. J Clin Aesthet Dermatol. 2010;3:26-9.
- [Google Scholar]
- Photodynamic therapy with topical 5% 5-aminolevulinic acid for the treatment of truncal acne in Asian patients. J Drugs Dermatol. 2016;15:727-32.
- [Google Scholar]
- Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-73.e33.
- [CrossRef] [PubMed] [Google Scholar]
- A single-center, randomized double-blind, parallel-group study to examine the safety and efficacy of 3mg drospirenone/0.02 mg ethinyl estradiol compared with placebo in the treatment of moderate truncal acne vulgaris. J Drugs Dermatol. 2013;12:633-7.
- [Google Scholar]
- Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne vulgaris. J Am Acad Dermatol. 2014;71:450-9.
- [CrossRef] [PubMed] [Google Scholar]
- Results of a Phase III, double-blind, randomized, parallel-group, non-inferiority study evaluating the safety and efficacy of isotretinoin-Lidose in patients with severe recalcitrant nodular acne. J Drugs Dermatol. 2014;13:665-70.
- [Google Scholar]
- Chemical peels in the treatment of acne: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:365-72.
- [CrossRef] [PubMed] [Google Scholar]







