Translate this page into:
Acquired trichorrhexis nodosa of the beard

*Corresponding author: P. R. Akhil, Department of Dermatology, Government Medical College, Kollam, Kerala, India. akhilpr111@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Athira S, Akhil PR, Subramoniam L, Ashok P, Acquired trichorrhexis nodosa of the beard. CosmoDerma. 2024;4:50. doi: 10.25259/CSDM_28_2024
Dear Sir,
A male shopkeeper, 38 years of age with no known comorbidities, presented with complaints of multiple asymptomatic white dots on his beard. The patient reported an 8-month history of white dots in the central portion of his beard with breakage of hair limited to this area. There were no similar manifestations at other sites. There was no family history of skin or hair disorders. On clinical examination, white nodes were observed on the hair shafts of the central portion of the beard, with white nodes more on the mid and distal ends of the hair shaft [Figure 1]. No such lesions were observed in the hairs on the sides of the beard. The hair density of the beard was normal. The surrounding skin also appeared normal. No abnormalities were observed in the hair shaft of the scalp and eyebrows. The differential diagnosis considered were white piedra, hair casts, trichorrhexis nodosa (TN), trichorrhexis invaginata, and seborrheic dermatitis. Trichoscopy revealed a “thrust paint brush” appearance of the hair shaft [Figure 2]. Light microscopy of the hair shaft showed a “splayed paint brush bristle” appearance [Figure 3]. No lice, nits, peripilar scale or casts were identified on trichoscopy. Microscopic examination of the 10% potassium hydroxide (KOH) mount of the hair shaft did not show any fungal elements. Fungal culture was also negative.

- Clinical image showing white nods on the hair shaft of the central part of the beard.

- Trichoscopy (dino-lite AM2111) showing “thrust paint brush” appearance (blue arrows) of the hair shaft (×20).
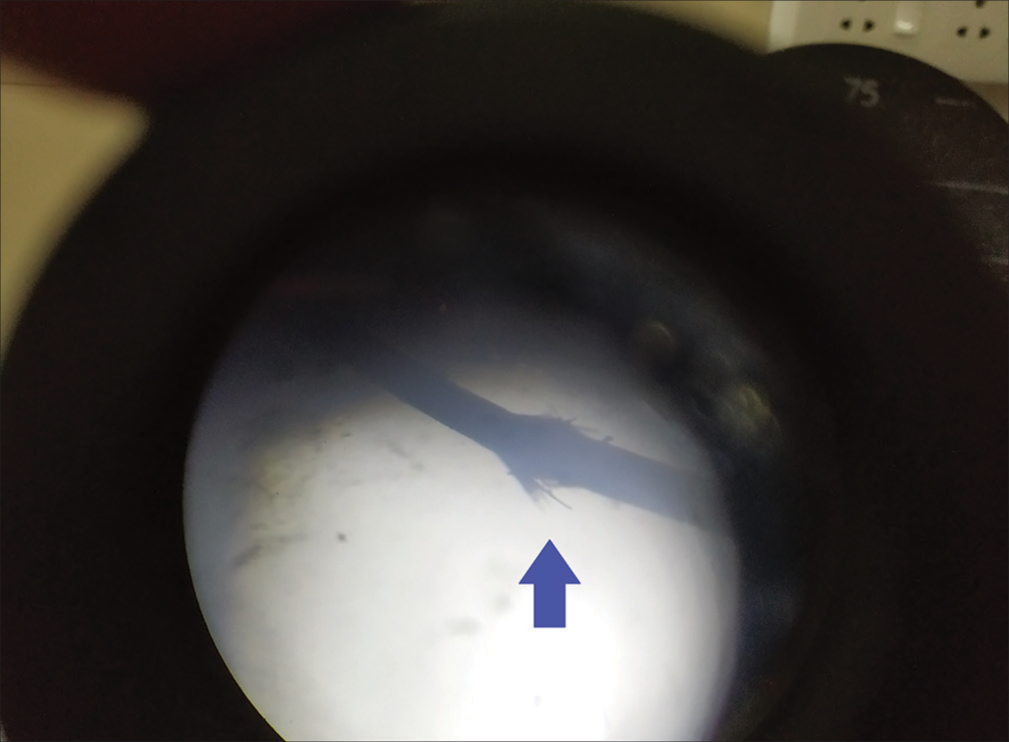
- Light microscopy showing “Splayed paint brush bristle” appearance (blue arrows).
Based on the clinical and dermoscopic features, a negative KOH test for fungus, lack of signs of perifollicular inflammation, the diagnosis of localized TN of the beard was made. The patient gave a history of excessive rubbing and habitual pulling of the beard hair. There was no history of excessive heat exposure or chemical treatments. He gave a history of regular use of face mask while going outdoor.
The patient was subjected to a blood hemogram, serum ferritin estimation, and thyroid function test, all of them were normal. Thus, we concluded that TN localized to the mid portion of the beard in this patient could be due to rubbing and pulling of the hair, and friction from regular use of face mask must have contributed to the condition. The patient was counseled to avoid rubbing of beard, trimming his beard short, and he was reassured that the condition is benign. Psychiatry evaluation could not be done for habitual pulling of beard hair as he was not willing for the same.
TN is the most common hair shaft disorder associated with hair fragility. TN presents as brittle easily broken and lustreless hair with white nodular swellings at irregular intervals along the hair shaft. The diagnosis is typically made with trichoscopy, the characteristic finding is a “splayed paint brush bristle” appearance, which is caused by a breach of the cuticle leading to exposure of the fibers and increasing their susceptibility to fracture. It can either be inherited or acquired. Acquired TN is caused by trauma, which can be chemical, mechanical or thermal injury. In patients with pre-existing defects such as monilethrix, pseudomonilethrix, and ringed hair, trivial trauma such as combing and brushing can itself induce TN.Localized TN is a type of acquired TN in which localized patches of TN occur in response to repeated frictional trauma often due to trichoteiromania. Trichoteiromania means “compulsive rubbing of hair,” is a disease grouped under the compulsive hair disorder group along with diseases such as trichophagia and trichotilomania.[1-3]
Hair casts/pseudonits can be differentiated from TN by cylindrical, freely movable tubular structures that encircle the hair shafts of the scalp and are not associated with hair fragility. Dermoscopy shows multiple peripilar casts as amorphous tubular or cylinder-shaped structures encircling the hair shaft with length greater than width. White piedra is a superficial fungal infection of hair caused by Trichosporon species presenting as white nodules encircling the hair shaft and typically do not cause hair fragility and is soft in consistency. Trichoscopy shows white amorphous material encasing the hair. Trichorrhexis invaginita (bamboo hair) is commonly associated with Netherton syndrome and is characterized by the invagination of the distal hair shaft into the proximal portion and can occur as an isolated disease entity. Clinically, hair has a dry lustreless, brittle appearance with increased fragility. Trichoscopy shows intussusception of the distal hair shaft into the proximal portion leading to a golf tee appearance. Trichoschisis refers to the localized absence of cuticle that leads to exposure and a clean transverse fracture of the hair shaft. Trichoschisis is associated with low sulfur-containing hair seen in trichothiodystrophy, but it can also occur due to external trauma such as heat, chemicals, and excess brushing. Dermoscopy shows tiger tail deformity and clean transverse fractures.[1,4,5]
Among the acquired TN cases, the most rare form is the localized TN. It seems to be under reported probably due to its benign and inconspicuous nature. It is usually seen associated with underlying pruritic dermatoses. Fowler and Tosti reported a similar case of TN as a result of frictional alopecia in a young girl subsequently diagnosed as trichoteiromania. Another case by Jindal et al. on a 20-year-old girl with anxiety who presented with an area of partial hair loss over the left sideburn associated with Trichorrhexis nodosa was reported in India. A similar case was reported by Gangal et al. as a mask-associated acquired TN of the beard where trauma and friction from frequent mask wearing resulted in TN.[6-8]
Acquired TN of the beard is probably an under-reported entity. The peculiarity of the present case is that the lesions were localized to the mid portion of the beard, suggesting trauma and friction being the probable cause of TN. Trichoscopy is one simple and non-invasive, bedside tool that aids in prompt diagnosis. Although history is important in identifying the etiology, it could be subject to bias since it relies on the recall of the patient.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Fitzpatrick’s dermatology In: Fitzpatrick’s dermatology (9th ed). New York, NY: McGraw-Hill Education; 2019. Available from: https://accessmedicine.mhmedical.com/content.aspx?aid=1160945490 [Last accessed on 2024 Feb 18]
- [Google Scholar]
- Psychotrichology: Psychosomatic aspects of hair diseases. J Dtsch Dermatol Ges. 2013;11:125-35.
- [CrossRef] [PubMed] [Google Scholar]
- White piedra: An uncommon superficial fungal infection of hair. Skin Appendage Disord. 2022;8:34-7.
- [CrossRef] [PubMed] [Google Scholar]
- A case of friction alopecia in a healthy 15-year-old girl. Skin Appendage Disord. 2019;5:97-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired trichorrhexis nodosa secondary to trichoteiromania: Prompt diagnosis using trichoscopy. Int J Trichology. 2022;14:34-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mask-associated acquired trichorrhexis nodosa of the beard. JAAD Case Rep. 2022;21:101-2.
- [CrossRef] [PubMed] [Google Scholar]





