Translate this page into:
A case of loose anagen hair syndrome associated with trichotillomania in a 14-year-old girl

*Corresponding author: Naveen Thomas, Department of Dermatology, Medical Trust Hospital, Kochi, Kerala, India. naveenthomas04@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Thomas N, Francis JV, Athira R. A case of loose anagen hair syndrome associated with trichotillomania in a 14-year-old girl. CosmoDerma. 2024;4:49. doi: 10.25259/CSDM_24_2024
Abstract
Loose anagen hair syndrome (LAHS) and trichotillomania (TTM) are two distinct conditions. LAHS is a rare condition characterized by easily removable anagen hair without any sensation of pain. It primarily affects young girls and is associated with a sparse hair growth and a delicate hair texture. LAHS can occur spontaneously or be inherited in an autosomal recessive manner. On the other hand, TTM, also known as hair pulling disorder, is an obsessive-compulsive disorder characterized by the recurrent, overwhelming urge to repeatedly pull out one’s hair. Hair pulling can occur anywhere on the body but is most common on the scalp, eyebrows, and eyelashes and subsequently results in bald patches. It is linked to psychosocial impairment and a decrease in the overall quality of life. We present a case of 14-year-old female with a longstanding history of sparse and disorderly hair since childhood due to LAHS associated with TTM. Treatment involved topical minoxidil and psychiatric counseling, resulting in significant improvement initially. However, a relapse was observed a year later, emphasizing the complexity of managing this dual pathology.
Keywords
Loose anagen hair syndrome
Trichotillomania
Hair pull test
Trichoscopy
Trichogram
INTRODUCTION
Loose anagen hair syndrome (LAHS) is a rare disorder of hair growth that affects mainly children, especially girls. It is characterized by easily pluckable anagen hair that do not grow in length and have abnormal morphology. The etiology of LAHS is unknown, but genetic factors, immunological abnormalities, and environmental influences have been suggested.[1,2]
Trichotillomania (TTM) is a psychiatric condition in which patients pull out their own hair compulsively, resulting in noticeable hair loss.[3]
The association of LAHS with TTM is very rare, with only a few cases reported in the literature.
CASE REPORT
A 14-year-old girl presented with complaints of sparse and unruly hair since childhood. She said that her hair was not growing in length, but there was no breaking of hair or patches with loss of hair. She also admitted that she had a habit of pulling her hair when she was stressed or bored. She denied any history of trauma, infection, medication use or family history of similar problems. On examination, she had sparse and lusterless hair [Figures 1a and b]. There was mild diffuse hair loss and thinning. Hair was easily pluckable with gentle traction. There were no clear patches of alopecia, no broken hair at different lengths, no exclamation mark hair, and no scaling or erythema. Teeth and nails were normal. Systemic examination was normal.

- Clinical picture of scalp and trichoscopy before treatment. (a and b) Note the sparse lusterless, unruly, and short hair. (c) Trichoscopy reveals very mild anisotrichosis, scaling, and occasional broken hair and black dots (Arrows). No exclamation mark hair.
The hair pull test was positive with more than ten hair obtained with gentle traction. Trichoscopy revealed very mild anisotrichosis (variation in hair diameter), scaling, 3–4 black dots (hair follicle openings filled with keratin or melanin), and occasional broken hair, and no exclamation mark hair (short, tapered, and broken hair) [Figure 1c]. Trichogram showed 90% anagen hair with absent inner and outer root sheath, ruffling of the cuticle, and distorted and twisted hair shaft close to the root. The hair bulb was at an acute angle to the shaft [Figure 2a]. Skin biopsy from the scalp showed clefting of the inner and outer root sheath with the absence of a hair shaft. The follicles were misshapen and dilated without any perifollicular inflammatory infiltrates [Figures 2b and c]. The above findings led to a diagnosis of loose anagen hair syndrome.
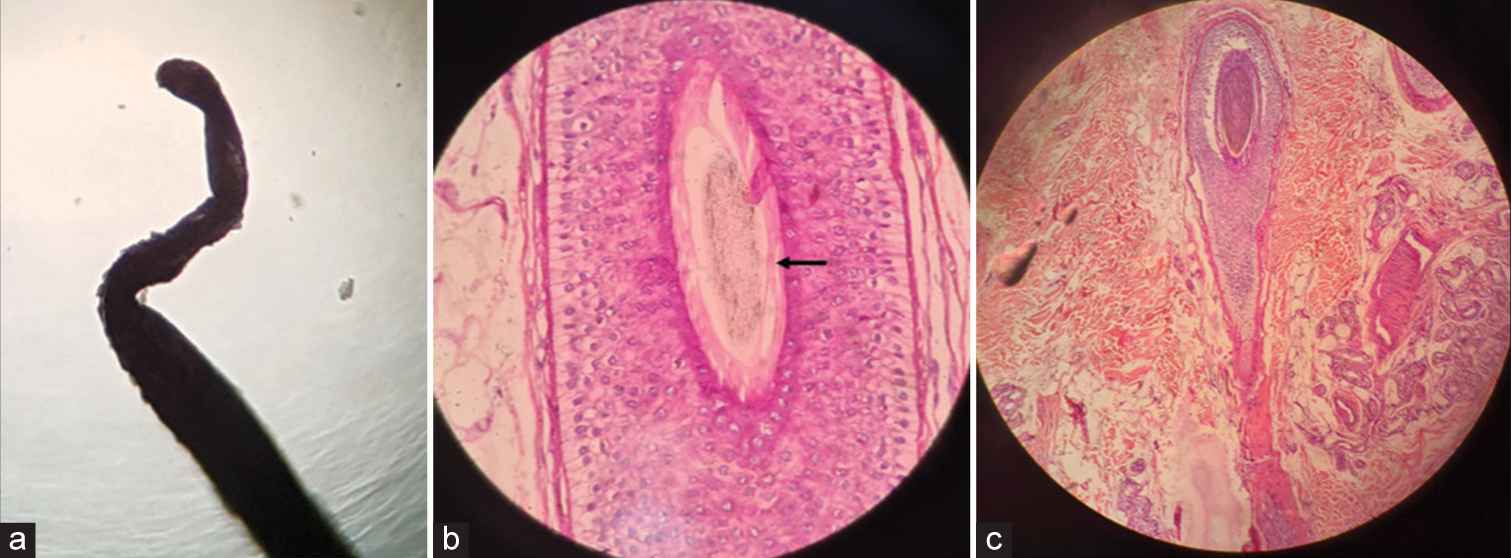
- (a) Trichogram showing anagen hair with absent inner and outer root sheath, ruffling of the cuticle, and distorted and twisted hair shaft. (b) Skin biopsy showing CLEFTING of the inner and outer root sheath with absence of hair shaft (black arrow) (H&E x200). (c) Misshapen follicles without any perifollicular inflammatory infiltrates (H&E x100).
She was prescribed topical minoxidil 2% solution twice daily and referred to a psychiatrist for further evaluation and management of TTM. After three months of treatment, there was good hair growth and improvement in hair density and texture [Figure 3a]. However, 1 year later, she came back with patchy hair loss on the right side of her scalp [Figure 3b]. Trichoscopy showed hair broken at different lengths, irregular coarse black dots, frayed tips, and mild anisotrichosis. She confessed that she was pulling her hair during times of examination and stress. Based on these findings, a diagnosis of LAHS with TTM was made. She was counseled about the nature of her condition and advised not to pull her hair.
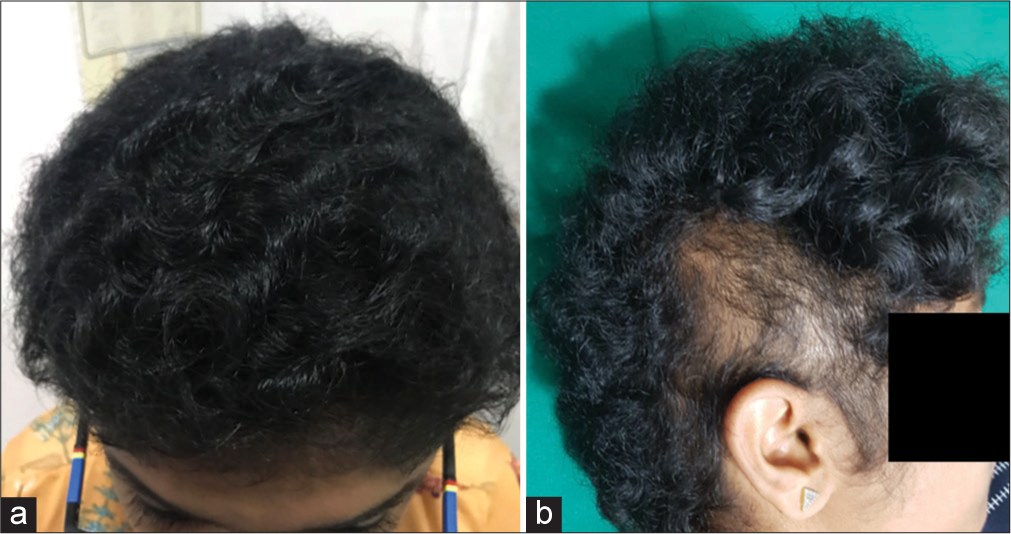
- (a) Three months after treatment with minoxidil. (b) One year later, patchy loss of hair on the right side due to trichotillomania, good hair growth in other areas.
DISCUSSION
The diagnosis of LAHS is based on clinical features, a positive hair pull test, and characteristic findings on trichogram and histopathology.[2,4,5]
Trichogram is the microscopic examination of the plucked hair that enable the assessment of the hair cycle and morphology. It can help in the diagnosis of LAHS by showing a predominance of anagen hair (>90%) with abnormal features, such as absent inner and outer root sheath, ruffling of the cuticle, distorted and twisted hair shaft close to the root, and acute angle of the hair bulb to the shaft. These features can help to differentiate LAHS from other causes of anagen effluvium, such as chemotherapy-induced alopecia or loose anagen hair associated with ectodermal dysplasia.[2,5,6]
Histopathology is the gold standard for the diagnosis of LAHS. It shows clefting of the inner and outer root sheath with the absence of a hair shaft. The follicles are misshapen and dilated without any perifollicular inflammatory infiltrates. These features can help to differentiate LAHS from other causes of scarring alopecia, such as lichen planopilaris or discoid lupus erythematosus.[4,6,7]
TTM is classified as an impulse control disorder or a body-focused repetitive behavior disorder. The prevalence of TTM ranges from 0.6% to 4% in the general population, with a female predominance.[3,8] The onset of TTM usually occurs in childhood or adolescence and is often triggered by stress or boredom. The diagnosis of TTM requires the presence of the following criteria: (a) Recurrent and compulsive hair-pulling that leads to noticeable alopecia; (b) repeated unsuccessful attempts to reduce or cease the hair-pulling behavior; (c) clinically significant distress or functional impairment caused by the hair pulling; and (d) exclusion of other medical or psychiatric conditions that could account for the hair loss.[3,8] The treatment of TTM involves pharmacotherapy and psychotherapy, such as cognitive behavioral therapy, habit reversal training, and acceptance and commitment therapy.
Trichoscopy can also help in the diagnosis of TTM by showing features such as hair broken at different lengths, irregular coarse black dots, frayed tips, coiled hair (hair that curl around themselves), flame hair (hair that taper abruptly at both ends), V-sign (two hair emerging from a single follicle), tulip hair (hair with bulbous ends), and trichoptilosis (split ends). These features can help to differentiate TTM from other causes of patchy alopecia in children, such as alopecia areata or tinea capitis.[3,8]
The association of LAHS with TTM is very rare, with only a few cases reported in the literature.[6-8] The possible mechanisms for this association are not clear. One hypothesis is that LAHS may predispose to TTM by making the hair more easily pluckable and less resistant to traction.[5,6] Another hypothesis is that TTM may aggravate LAHS by causing more damage to the already fragile anagen hair. A third hypothesis is that both LAHS and TTM may share some common genetic or environmental factors that affect the hair growth cycle.[8-10]
The treatment of LAHS with TTM involves topical minoxidil and psychiatric counseling. Topical minoxidil may improve hair density and length in children with LAHS by stimulating the hair growth cycle and enhancing hair quality.[3,4,6] Psychiatric counseling may help patients with TTM to identify and modify the triggers, emotions, and cognitions associated with hair pulling, and to learn alternative coping skills and strategies to reduce the urge and frequency of hair pulling.[5]
The prognosis of LAHS with TTM is variable, depending on the severity and duration of both conditions. Some cases may improve spontaneously or with treatment over time, while others may persist or relapse. The combination of LAHS and TTM may pose a greater challenge for the management and outcome of both conditions.
CONCLUSION
The comprehensive diagnostic approach, which includes clinical examination, hair pull tests, trichoscopy, and histopathology, is crucial for confirming the dual pathology of LAHS associated with TTM. The management of LAHS and TTM requires a tailored therapeutic approach, which combines dermatological treatments like topical minoxidil with psychological interventions to address the behavioral aspects of TTM. The prognosis depends on several factors, including the severity, duration, and patient adherence to treatment protocols. This rare dual condition necessitates increased clinical awareness and ongoing research to elucidate the underlying pathophysiological mechanisms and optimize long-term outcomes for affected individuals.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Trichotillomania: A current review. Clin Psychol Rev. 2010;30:181-93.
- [CrossRef] [PubMed] [Google Scholar]
- Loose anagen hair syndrome: An underdiagnosed condition in males. Pediatr Dermatol. 2010;27:408-9.
- [CrossRef] [PubMed] [Google Scholar]
- Loose anagen hair syndrome and loose anagen hair. Arch Dermatol. 2002;138:521-2.
- [CrossRef] [PubMed] [Google Scholar]
- Loose anagen hair syndrome. Indian Dermatol Online J. 2014;5:548-9.
- [CrossRef] [PubMed] [Google Scholar]
- Trichotillomania (hair pulling disorder) In: Psychodermatology in clinical practice. Cham: Springer International Publishing; 2021. p. :197-213.
- [CrossRef] [Google Scholar]
- Low-dose oral minoxidil improves global hair density and length in children with loose anagen hair syndrome. Br J Dermatol. 2021;184:977-8.
- [CrossRef] [PubMed] [Google Scholar]
- Loose anagen syndrome: A retrospective chart review of 37 cases. Pediatr Dermatol. 2016;33:507-10.
- [CrossRef] [PubMed] [Google Scholar]






