Translate this page into:
Ultraviolet fluorescence dermoscopy in dermatology

*Corresponding author: Sheetanshu Kumar, Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. kumar.sheetanshu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sivakumar A, Arora K, Kumar S. Ultraviolet fluorescence dermoscopy in dermatology. CosmoDerma. 2025;5:4. doi: 10.25259/CSDM_198_2024
INTRODUCTION
Ultraviolet (UV) imaging, including Wood’s lamp and UV photography, has long been used in dermatology.[1] Modern dermatoscopes now incorporate real-time UV imaging with magnification. This article outlines the applications of UV fluorescence dermoscopy (UVFD) to assist residents and practicing dermatologists in its effective use, particularly for patients with skin of color.
PRINCIPLE
Dermoscopes equipped with UV sources, typically light-emitting diodes, illuminate the skin. The incident light undergoes scattering and absorption, while the remaining reflected UV light is filtered out by the UV filter. When the incident light interacts with chromophores, it excites them from a ground state to an excited state, leading to the emission of a photon as they return to the ground state. This emitted photon, which has a longer wavelength, appears as fluorescent visible light, a phenomenon known as the Stokes effect [Figure 1].
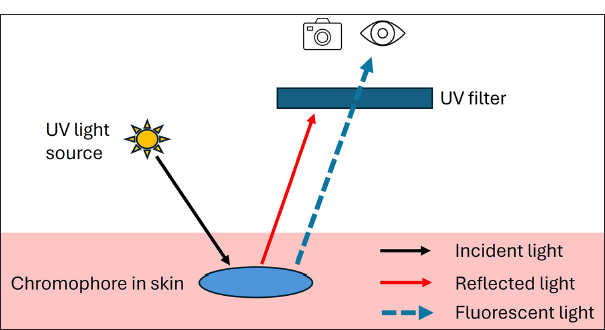
- Principle of ultraviolet (UV) fluorescence dermoscopy.
CLINICAL APPLICATIONS
The clinical applications of UVFD can be classified as follows,
Infectious dermatoses
-
Scabies: Under UVFD, the burrows in the stratum corneum are highlighted (Scabies sign), appearing bluish-green due to the presence of exudates [Figure 2a].[2] This technique can also reveal the mite at the end of the tunnel (Ball sign) and fecal pellets (Glittering tail sign).[3,4]
![(a) Under Ultraviolet fluorescence dermoscopy (UVFD), scabies burrows appear as bright bluish serpiginous lesions (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) The larval tracks of cutaneous larva migrans are more clearly visualized under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode).](/content/130/2025/5/1/img/CSDM-5-4-g002.png) Figure 2:
Figure 2:- (a) Under Ultraviolet fluorescence dermoscopy (UVFD), scabies burrows appear as bright bluish serpiginous lesions (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) The larval tracks of cutaneous larva migrans are more clearly visualized under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode).
Cutaneous larva migrans: The larval tracks are more clearly visualized using UVFD [Figure 2b].
Trichobacteriosis axillaris: UVFD reveals yellowish-green concretions resulting from unknown chromophores present in bacterial concretions and sweat retention.[5]
Pitted keratolysis: UVFD accentuates the plantar pits, which appear coral red, accompanied by a parallel ridge pattern with coral red dots and clods in the eccrine and perieccrine regions.[6]
Pseudomonal infections: Greenish fluorescence observed in pseudomonal skin and nail infections under UVFD is attributed to the bacterial by-product pyoverdine.
Pityrosporum folliculitis: Follicular bluish fluorescence results from fungal enzyme production, hyperkeratosis, and inflammation, contrasting with truncal acne, which shows no fluorescence and presents as follicular blackouts (absent cutibacterial reddish fluorescence).[7]
Molluscum contagiosum: The umbilicated papules of molluscum become more pronounced with central whitish fluorescence under UVFD.[8]
Demodicosis: UVFD aids in identifying Demodex mites, which exhibit bright bluish fluorescence, likely due to ingested sebum.[9]
Inflammatory dermatoses
-
Psoriasis: Pinkish-red fluorescence is observed due to protoporphyrin IX [Figure 3a]. The intensity of this fluorescence correlates with disease severity, aiding in the monitoring of disease activity. In inverse psoriasis, peripapillary reddish fluorescence helps differentiate it from erythrasma.[10,11]
![(a) Psoriasis vulgaris exhibits a pinkish-red fluorescence under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Wickham’s striae in lichen planus are visible under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) In acne vulgaris, follicular reddish fluorescence (indicating cutibacterial colonization) manifests as follicular blackouts (Dermlite DL5, ×10 magnification; Polarized and UV mode). (d) The peripheral collarette of pityriasis rosea is observed under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode).](/content/130/2025/5/1/img/CSDM-5-4-g003.png) Figure 3:
Figure 3:- (a) Psoriasis vulgaris exhibits a pinkish-red fluorescence under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Wickham’s striae in lichen planus are visible under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) In acne vulgaris, follicular reddish fluorescence (indicating cutibacterial colonization) manifests as follicular blackouts (Dermlite DL5, ×10 magnification; Polarized and UV mode). (d) The peripheral collarette of pityriasis rosea is observed under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode).
Lichen planus: No fluorescence is observed in lichen planus; however, poorly demarcated white lines corresponding to Wickham’s striae can be seen [Figure 3b].[12]
Acne vulgaris: Comedonal lesions may exhibit orangishred fluorescence due to coproporphyrin III produced by Cutibacterium acnes. In inflammatory papulopustular lesions, this fluorescence is disrupted, resulting in follicular blackout areas [Figure 3c].[12]
Pityriasis rosea: Under UVFD, the peripheral collarette displays bright bluish fluorescence [Figure 3d].[12]
Eczema: Bluish or yellowish-green fluorescence may be observed due to bilirubin in exuded serum and crusting.[12]
Cutaneous collagenous vasculopathy: UVFD reveals thick linear vessels with alternating constrictions and dilations, described as the “sausage string appearance,” corresponding to hyalinized vessel walls.[13]
Pigmentary dermatoses
-
Vitiligo: Under UVFD, vitiligo reveals bluish-white autofluorescence from the underlying dermal collagen, enhancing the visibility of lesion borders [Figure 4a]. Stable vitiligo typically exhibits defined borders with perifollicular depigmentation, while progressive vitiligo presents poorly defined borders with perifollicular repigmentation.[14]
![(a) The borders of lesions in vitiligo are better delineated under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Tinea versicolor displays a greenish fluorescence under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) Erythrasma is characterized by a coral red diffuse and perifollicular fluorescence (Dermlite DL5, ×10 magnification; UV mode). (d) Bluish chalky white fluorescence is seen in terra firmaforme dermatosis under UVFD (Dermlite DL5, ×10 magnification; UV mode).](/content/130/2025/5/1/img/CSDM-5-4-g004.png) Figure 4:
Figure 4:- (a) The borders of lesions in vitiligo are better delineated under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Tinea versicolor displays a greenish fluorescence under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) Erythrasma is characterized by a coral red diffuse and perifollicular fluorescence (Dermlite DL5, ×10 magnification; UV mode). (d) Bluish chalky white fluorescence is seen in terra firmaforme dermatosis under UVFD (Dermlite DL5, ×10 magnification; UV mode).
Pityriasis versicolor: Greenish fluorescence, resulting from the fungal metabolite butyrolactone, is observed in pityriasis versicolor. This fluorescence may occur along skin creases, in perifollicular areas, and as single or double-edged scales [Figure 4b]. In achromic cases, follicular blackouts may occur due to the antibacterial effects of azelaic acid, and a darker rim surrounding hypopigmented macules, known as the “contrast halo sign,” can also be present.[15]
Erythrasma: UVFD displays coral red fluorescence due to coproporphyrin III produced by Corynebacterium [Figure 4c]. This fluorescence can appear diffusely, in a polygonal distribution, or peripilar areas, aiding in the differentiation from candidal intertrigo (which shows no fluorescence) and pseudomonal intertrigo (which exhibits green fluorescence).[5]
Progressive macular hypomelanosis: Reddish folliculocentric fluorescence is evident under UVFD, helping to differentiate this condition from tinea versicolor and vitiligo.[12]
Terra firma-forme dermatosis: Bluish plaques with a mosaic distribution are observed under UVFD, assisting in distinguishing this condition from ichthyosis and acanthosis nigricans [Figure 4d].[16]
Neoplastic and hyperplastic conditions
-
Seborrheic keratosis: The comedo-like openings and milium-like cysts exhibit bright bluish-white fluorescence, known as the “UV blink sign” [Figure 5a].[8]
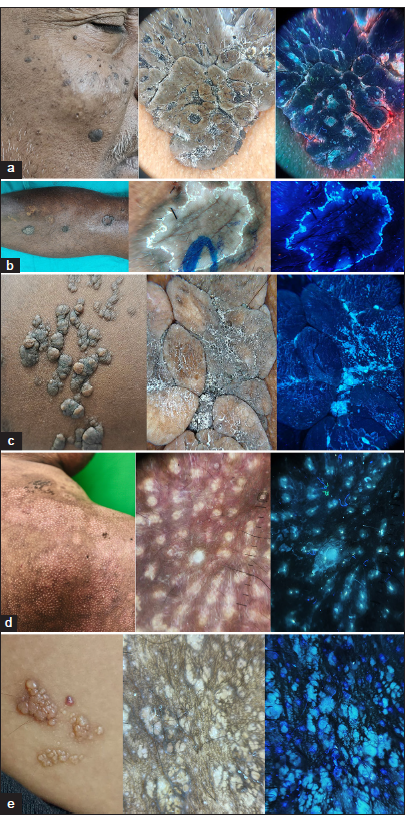 Figure 5:
Figure 5:- (a) Comedonal plugs and milia-like cysts in seborrheic keratosis are enhanced by Ultraviolet fluorescence dermoscopy (UVFD), often referred to as the Ultraviolet (UV) blink sign (Dermlite DL5, ×10 magnification; Polarized and UV mode). (b) The double-edged rim in porokeratosis (coronoid lamella) is visualized as bright bluish fluorescence under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) Keratotic debris and comedonal plugging in nevus lipomatosus are more apparent under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (d) Sebaceous hyperplasia is better visualized with UVFD, where sebum extrusion appears as yellowish or bluish fluorescent material (Dermlite DL5, ×10 magnification; Polarized and UV mode). (e) Bluish fluorescence observed in microcystic lymphatic malformation under UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode).
Porokeratosis: The annular single- or double-edged keratotic rim is highlighted under UVFD with bright bluish fluorescence [Figure 5b].[12]
Nevus lipomatosus: Comedonal plugs and keratotic debris are more clearly visualized as bright bluish fluorescence [Figure 5c].
Sebaceous hyperplasia: This condition appears as a yellowish-green structure under UVFD, aiding in its differentiation from milia or adnexal tumors [Figure 5d].[12]
Neoplastic conditions: Glomus tumors display a “pink glow sign” under UVFD.[17] Basal cell carcinoma may reveal multiple aggregated yellow globules with enhanced fluorescence, which helps distinguish it from apocrine hidrocystomas that exhibit uniform translucent fluorescence.[18]
Lymphatic malformation: Small translucent lacunae are more distinctly observed as bluish-white translucent globules under UVFD [Figure 5e].
Hair disorders
-
Tinea capitis: Bright greenish fluorescence is observed in tinea capitis caused by Microsporum species, attributed to the production of pteridine [Figure 6a].[19]
![(a) Bright green fluorescence of tinea capitis is evident under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Premature canities is better visualized with UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) In lichen planopilaris, the absence of normal follicular fluorescence indicates scarring alopecia (Dermlite DL5, ×10 magnification; Polarized and UV mode).](/content/130/2025/5/1/img/CSDM-5-4-g006.png) Figure 6:
Figure 6:- (a) Bright green fluorescence of tinea capitis is evident under Ultraviolet fluorescence dermoscopy (UVFD) (Dermlite DL5, ×10 magnification; Polarized and Ultraviolet [UV] mode). (b) Premature canities is better visualized with UVFD (Dermlite DL5, ×10 magnification; Polarized and UV mode). (c) In lichen planopilaris, the absence of normal follicular fluorescence indicates scarring alopecia (Dermlite DL5, ×10 magnification; Polarized and UV mode).
Premature canities: UVFD effectively assesses premature canities, leukotrichia, and poliosis, as these conditions appear brighter under UV light [Figure 6b].[20]
Scarring alopecia: Folliculocentric reddish fluorescence in a normal scalp resembles a “starry night sky pattern,” indicating viable hair. The absence of this pattern signifies the destruction of follicular units, suggesting a poorer prognosis [Figure 6c].[21,22]
Use in dermatosurgery
Biopsy site identification: UVFD is a simple method for biopsy site identification as it appears darker compared to normal skin due to the presence of inflammation, neo-angiogenesis, and scarring.[23]
The comparison of polarized and UVFD findings has been summarized in Tables 1-5.
| S. No | Condition | Polarized dermoscopy | UVFD | Comments |
|---|---|---|---|---|
| 1. | Scabies | White tunnel with dark brown triangular structure at the end (“triangle sign”/”delta wing jet with contrail sign”)[24] | Bluish-green fluorescence highlighting the tunnels (scabies sign) along with fluorescence mite (ball sign) and fecal pellets (Glittering tail sing) | Exudation due to the inflammation along with scaling leads to the fluorescence highlighting theburrows |
| 2. | Cutaneous Larva migrans | Red to pink to purple structureless area in a linear serpiginous and winding pattern, corresponding to the track created by the migration of the larva.[25] | Bluish fluorescence of the larval tracks seen better under UVFD | Superficial scaling along the serpiginous tunnels |
| 3. | Pitted keratolysis | Heterogeneous pitting with interruption of dermatoglyphics[26] | Presence of coral red clods along the eccrine and perieccrine regions | Production of corynebacterial coproporphyrins |
| 4. | Pseudomonal infections | Presence of greenish pigment in the nail plate (Green aurora sign)[27] | Greenish fluorescence of the nail plate | Production of pseudomonal pigment mainly pyoverdine and pyocyanin |
| 5. | Pityrosporum folliculitis | Follicular-based papules and pustules with perifollicular erythema and scaling with coiled, looped, and hypopigmented hairs[28] | Follicular-based bluish fluorescence | Follicular-based inflammation, hyperkeratosis, and fungal enzymes |
| 6. | Molluscum contagiosum | Polylobular, white-yellow, amorphous structure in the center with a surrounding crown of vessels[29] | More prominent umbilicated papules appearing as bluish fluorescence | Due to the presence of molluscum bodies in the central umbilication |
| 7. | Demodicosis | Follicular gelatinous threads or filaments (Demodex tails) along with dilated follicular openings with grayish-brown plugging and erythema (Demodex follicular openings)[30] | Demodex mites are seen as bright blue, fluorescent objects | Due to ingested sebum visualized through the translucent mite body |
UVFD: Ultraviolet fluorescence dermoscopy
| S. No | Condition | Polarized dermoscopy | UVFD | Comments |
|---|---|---|---|---|
| 1. | Psoriasis | Regularly arranged dotted vessels along with whitish scales over a light red background[31] | Pinkish-red uniform fluorescence | Presence of entrapped protoporphyrin on the scales |
| 2. | Lichen planus | Presence of Wickham striae over a violaceous background with red dots and capillaries[32] | Poorly demarcated white lines | Correspond to Wickams striae |
| 3. | Acne vulgaris | Dilated central pore with brownish yellow plugging (comedones) along with erythematous round area (papules) and whitish yellowish structures (pustules)[33] | Orange-red fluorescence of the comedonal plug, follicular blackouts in papulopustular inflammatory lesions | Production of coproporphyrin II by Cutibacterium acnes |
| 4. | Pityriasis Rosea | Peripheral collarette scaling, central scale with peripheral dotted vessels in a patchy distribution. There is the presence of brown globules and central yellow with a peripheral red background[34] | Bright bluish collarette of scaling noted | Collarette of Scales that reflect visible light |
| 5. | Eczema | Dotted vessels arranged in random or clusters along with yellowish scales and serocrusts, hemorrhages[35] | Bluish/yellow-green fluorescence | Due to exuded bilirubin along with serocrusts |
| 6. | Cutaneous collagenous vasculopathy | ick linear serpentine vessels with alternate constrictions and dilatations of reticular/polygonal arrangement[13] | ick serpentine vessels with sausage string appearance along with darker perivascular structureless area | Higher absorption of UV spectrum by the hemoglobin |
UV: Ultraviolet, UVFD: Ultraviolet fluorescence dermoscopy
| S. No | Condition | Polarized dermoscopy | Ultraviolet fluorescent dermoscopy | Comments |
|---|---|---|---|---|
| 1. | Vitiligo | In stable vitiligo, there can be perifollicular depigmentation, perilesional/marginal repigmentation, and perilesional erythema, whereas in unstable vitiligo, there is perifollicular pigmentation, reduced pigment network, trichrome pattern, starburst pattern, comet tail sign, micro Koebnerization, micro satellites, leukotrichia[36] | e bluish-white fluorescence makes the borders more apparent | Due to autofluorescence from the underlying dermalcollagen due to the absence of melanocytes |
| 2. | Pityriasis versicolor | Shows non-uniform pigmentation with perilesional hyperpigmentation. Scaling can be patchy, diffuse, peripheral, perifollicular, and along the furrows[37] | Greenish fluorescence of the scales seen, follicular blackouts in achromic pityriasis versicolor | Fungal production of pityralactone Interrupted cutibacterial reddish fluorescence due to the antibacterial activity of azelaic acid |
| 3. | Erythrasma | Hyperpigmentation along the skin folds[5] | Coral red fluorescence along the scaling | Production of coproporphyrin III by corynebacteria |
| 4. | Terra firma-forme dermatosis | Polygonal brown scales and clods arranged in a mosaic pattern[38] | Bluish plaques in a mosaic distribution | Reflection of visible light from the mosaic scales |
| 5. | Progressive macular hypomelanosis | Diffuse/focal whitish areas with subtle broken reticular network With fine whitish scales[39] | Reddish folliculocentric fluorescence | Follicular presence of coproporphyrin III |
| S.No | Condition | Polarized dermoscopy | UVFD | Comments |
|---|---|---|---|---|
| 1. | Seborrheic keratoses | Comedo-like openings, Cerebriform appearance, Milia-like cysts, Fingerprint-like structures, hairpin blood vessels, moth-eaten borders[40] | Enhanced bluish fluorescence of the comedo-like openings and milia-like cysts | Referred to as the “UV blink sign” |
| 2. | Porokeratosis | Central pale homogenous structureless area with a peripheral double marginated/tram track border[41] | Bright bluish keratotic rim highlighted in UVFD | Double-edged scale reflecting visible light |
| 3. | Nevus lipomatosus | Cerebriform pattern, with a honeycomb pigment network, and yellowish structureless areas[42] | Bright bluish fluorescence from keratotic debris and comedonal plugs | Bluish fluorescence fromkeratin |
| 4. | Basal cell carcinoma | Maple leaf-like areas, blue-white veils, telangiectasia, arborizing vessels, spoke wheel areas, areas of ulceration, and, MAY globules[43,44] | Multiple aggregated globules in BCC reveal bright white fluorescence in UVFD | Microcalcification showing enhanced fluorescence |
| 5. | Sebaceous hyperplasia | Multiple yellow/white nodules with branching linear vessels (crown vessels)[45] | Yellowish-green fluorescence of the sebaceous glands | Exuded sebum appears as yellow fluorescent structures |
| 6. | Lymphatic malformation | Multiple white or yellowish lacunae with surrounding pale septa and a few with hypopyon[46] | Bright bluish fluorescence of lacunae | e translucent lymph spaces reflect blue visiblelight |
MAY: Multiple aggregated yellow, UV: Ultraviolet, UVFD: Ultraviolet fluorescence dermoscopy, BCC: Basal cell carcinoma
| S. No | Condition | Polarized dermoscopy | UVFD | Comments |
|---|---|---|---|---|
| 1. | Premature canities | No specific dermoscopic features | Better seen as whitish fluorescence in UVFD | Absence of melanin in the hairshafts |
| 2. | Tinea capitis | Broken hairs, zig-zag hairs, comma hairs, corkscrew hairs, and more code hairs[47] | Bright green fluorescence of the hair shafts especially vellus hair involvement | Production of pteridine by Microsporum species |
| 3. | Scarring alopecia (lichen plano pilaris) | Presence of structureless areas (absent follicular openings), perifollicular erythema and scaling, and perifollicular whitish-grey scaling[48] | Absent follicular reddish fluorescence (follicular blackouts) | Destruction of viable hair follicles thereby colonizing cutibacteria producing the reddish fluorescence is lost |
UVFD: Ultraviolet fluorescent dermoscopy
Advantages and disadvantages of UV dermoscopy
Advantages - portability, ease of use, a combination of magnification with UV imaging which can be stored as electronic data in devices, no requirement of a dark room.[12]
Disadvantages - Disparity in quality and characteristics of images due to the variability of UVFD devices, skin pigmentation, sun damage, exogenous applications, uneven surfaces, applied pressure while using UVFD, and improper patient preparation.[12]
CONCLUSION
UVFD is an invaluable tool for dermatologists, especially in diagnosing dermatoses in patients with skin of color. A thorough understanding of its methods and principles is essential for accurate diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ultraviolet imaging in dermatology. Photodiagnosis Photodyn Ther. 2020;30:101743.
- [CrossRef] [PubMed] [Google Scholar]
- Using ultraviolet light in diagnosing scabies: Scabies' Sign via Wood's Lamp. J Am Acad Dermatol. 2023;89:e195-6.
- [CrossRef] [PubMed] [Google Scholar]
- A new sign with UV dermoscope in the diagnosis of scabies: Ball sign. Skin Res Technol. 2023;29:e13336.
- [CrossRef] [PubMed] [Google Scholar]
- Glittering trail: Feces of scabies indicated by high-power-field dermatoscopy using UV-A light. J Am Acad Dermatol. 2024;90:e17-8.
- [CrossRef] [PubMed] [Google Scholar]
- Role of dermatoscopy and the use of ultraviolet-induced fluorescence dermatoscopy in the diagnosis of erythrasma and other skin infections. BMJ Case Rep. 2024;17:e258821.
- [CrossRef] [PubMed] [Google Scholar]
- Ultraviolet-induced fluorescence dermatoscopy reveals fluorescent clues in pitted keratolysis. Dermatol Pract Concept. 2023;13:e2023242.
- [CrossRef] [PubMed] [Google Scholar]
- UV dermoscopy for the diagnosis of pityrosporum folliculitis. Dermatol Pract Concept. 2024;14:e2024092.
- [CrossRef] [PubMed] [Google Scholar]
- Ultraviolet reflectance dermoscopy. Indian J Dermatol Venereol Leprol. 2024;90:838-41.
- [CrossRef] [PubMed] [Google Scholar]
- Image gallery: Wandering demodex mite in vivo under ultraviolet dermoscopy of rosacea. Br J Dermatol. 2020;182:e2.
- [Google Scholar]
- Specific features of psoriasis vulgaris under the ultraviolet dermoscopy. Photodiagnosis Photodyn Ther. 2022;40:103100.
- [CrossRef] [PubMed] [Google Scholar]
- Pink-red fluorescence observed in ultraviolet-induced fluorescence dermoscopy of psoriatic plaques. Dermatol Pract Concept. 2023;13:e2023243.
- [CrossRef] [PubMed] [Google Scholar]
- Applications of ultraviolet and sub-ultraviolet dermatoscopy in neoplastic and nonneoplastic dermatoses: A systematic review. Dermatol Ther (Heidelb). 2024;14:361-90.
- [CrossRef] [PubMed] [Google Scholar]
- Could conventional, ultraviolet-induced fluorescence and sub-ultraviolet reflectance dermatoscopy assist the diagnosis of cutaneous collagenous vasculopathy? A case report. Dermatol Pract Concept. 2024;14:e2024077.
- [CrossRef] [PubMed] [Google Scholar]
- Novel ultraviolet-dermoscopy: Early diagnosis and activity evaluation of vitiligo. Skin Res Technol. 2023;29:e13249.
- [CrossRef] [PubMed] [Google Scholar]
- Pityriasis versicolor-a narrative review on the diagnosis and management. Life (Basel). 2023;13:2097.
- [CrossRef] [PubMed] [Google Scholar]
- Terra firma-forme dermatosis displays bright blue plaques in ultraviolet-induced fluorescence dermatoscopy. Australas J Dermatol. 2024;65:393-5.
- [CrossRef] [PubMed] [Google Scholar]
- "Pink glow": A new sign for the diagnosis of glomus tumor on ultraviolet light dermoscopy. Indian Dermatol Online J. 2015;6:S21-3.
- [CrossRef] [PubMed] [Google Scholar]
- The role of ultraviolet-induced fluorescence dermatoscopy for the detection of multiple aggregated yellow-white globules in basal cell carcinoma. J Am Acad Dermatol. 2024;91:1250-2.
- [CrossRef] [PubMed] [Google Scholar]
- Polarized and ultraviolet dermoscopy for the diagnosis of dermatophytosis of vellus hair. Indian J Dermatol Venereol Leprol. 2020;86:607.
- [CrossRef] [PubMed] [Google Scholar]
- Looking for a grey needle in a 'hair' stack! Using a Wood's lamp for evaluating canities. Indian J Dermatol Venereol Leprol. 2023;89:636-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ultraviolet-induced fluorescence dermoscopy aids in distinguishing scarring and nonscarring alopecia: Enhancing identification of hair follicle openings: The potential of ultraviolet-induced fluorescence dermoscopy in hair loss diagnosis. J Am Acad Dermatol. 2024;91:e1-2.
- [CrossRef] [PubMed] [Google Scholar]
- The “Starry Night Sky Sign” using ultraviolet-light-enhanced trichoscopy: A new sign that may predict efficacy of treatment in frontal fibrosing alopecia. Int J Trichology. 2018;10:241-3.
- [CrossRef] [PubMed] [Google Scholar]
- Ultraviolet-induced fluorescent dermoscopy for biopsy site identification prior to dermatologic surgery: A retrospective study. J Am Acad Dermatol. 2023;89:841-3.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of scabies by dermoscopy. Case Rep. 2009;2009:bcr0620080279.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy before and after treatment of cutaneous larva migrans: Through the dermoscope. Indian Dermatol Online J. 2022;13:690-4.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of pitted keratolysis. Case Rep Dermatol. 2010;2:146-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of green nail syndrome: The “green aurora sign”. Dermatol Pract Concept. 2021;11:e2021093.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of pityrosporum folliculitis. J Am Acad Dermatol. 2019;80:e43-4.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of molluscum contagiosum. Arch Dermatol. 2005;141:1644.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of dermoscopy in the diagnosis and monitoring treatment of demodicidosis. Dermatol Pract Concept. 2017;7:35-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical value of dermoscopy in psoriasis. J Cosmet Dermatol. 2024;23:370-81.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic signs of lichen planus. BMJ Case Rep. 2016;2016:bcr2015213923.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy and reflectance confocal microscopy correlations in nonmelanocytic disorders. Dermatol Clin. 2018;36:487-501.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of pityriasis rosea. BMJ Case Rep. 2023;16:e256304.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of inflammatory dermatoses (inflammoscopy): An up-to-date overview. Dermatol Pract Concept. 2019;9:169-80.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopic patterns in vitiligo. Dermatol Pract Concept. 2023;13:e2023197.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic pattern of pityriasis versicolor. Clin Cosmet Investig Dermatol. 2019;12:303-9.
- [CrossRef] [PubMed] [Google Scholar]
- Terra firme-forme dermatosis diagnostic sign and treatment: A case report. Case Rep Dermatol. 2019;11:108-12.
- [CrossRef] [PubMed] [Google Scholar]
- Spectrum of seborrheic keratoses in South Indians: A clinical and dermoscopic study. Indian J Dermatol Venereol Leprol. 2011;77:483-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of porokeratosis of mibelli. Indian Dermatol Online J. 2017;8:304-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopic evaluation of three cases of nevus lipomatosus cutaneous superficialis. Indian J Dermatol Venereol Leprol. 2017;83:383-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of basal cell carcinoma in skin of color: A retrospective cross-sectional study from Puducherry, South India. Indian J Dermatol Venereol Leprol. 2023;89:254-60.
- [CrossRef] [PubMed] [Google Scholar]
- White globules in basal cell carcinoma: A dermoscopic sign with preoperative implications. Dermatol Pract Concept. 2021;11:e2021103.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of sebaceous hyperplasia. Arch Dermatol. 2005;141:808.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of cutaneous lymphangioma circumscriptum. Dermatol Pract Concept. 2017;7:37-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tinea capitis in children and trichoscopic Criteria. Int J Trichology. 2017;9:47-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic findings in different clinical variants of lichen planus. Is dermoscopy useful? Dermatol Pract Concept 2015. ;. ;5:51-5.
- [CrossRef] [PubMed] [Google Scholar]





