Translate this page into:
Terra firma-forme dermatosis

*Corresponding author: Hsuan-Hsiang Chen, Department of Dermatology, National Taiwan University Hospital, Taipei, Taiwan. beauty101@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wang C, Chen H. Terra firma-forme dermatosis. CosmoDerma. 2025;5:3. doi: 10.25259/CSDM_182_2024
Abstract
Terra firma-forme dermatosis (TFFD), also known as Duncan’s dirty dermatosis, may mimic a variety of hyperpigmented dermatoses including dermatosis neglecta, dirty neck syndrome, and acanthosis nigricans. Herein, we report a TFFD case of a 5-year-old girl who had a medical history of atopic dermatitis and presented with a hyperpigmented, dirty-appearing neck rash that was refractory to frequent moisturizer application. We successfully cleared the lesions after rubbing with 70% isopropyl alcohol. We propose a simple diagnostic algorithm to differentiate these three similar hyperpigmented dermatoses.
Keywords
Dermatosis neglecta
Dirty neck syndrome
Duncan’s dirty dermatosis
Terra firma-forme dermatosis
INTRODUCTION
Terra firma-forme dermatosis (TFFD), also known as Duncan’s dirty dermatosis, is a benign skin condition first described in 1987 by Duncan et al.[1] Clinically, TFFD presents as asymptomatic brown-gray-black patches that resemble dirt. The lesions can have a verrucous or papillomatous surface, with some cases displaying a reticulated pattern interspersed with normal skin on the neck, face, trunk, ankles, and navel. The exact cause of TFFD is unclear but is thought to involve abnormal keratinocyte maturation. The differential diagnosis includes dermatosis neglecta (DN), acanthosis nigricans (AN), and dirty neck syndrome. Due to its low prevalence and high similarity with other hyperpigmented dermatoses, TFFD is often misdiagnosed and mistreated. Herein, we report a TFFD case of a 5-year-old girl who had been previously underdiagnosed and managed with frequent moisturizer application without obvious improvement.
CASE REPORT
A 5-year-old girl with atopic dermatitis and frequent moisturizer application presented to the clinic with a neck rash. Examination showed multiple asymptomatic hyperpigmented, dirty-appearing papules, and plaques in a linear arrangement on the neck [Figure 1a]. Dermoscopy revealed dark brown clods and scales resembling cornflakes, arranged in a linear pattern [Figure 1b]. DN and TFFD were suspected. Her mother reported that water, soap, and topical steroids were ineffective. We cleared the lesions by rubbing with 70% isopropyl alcohol, and the diagnosis of TFFD was made.
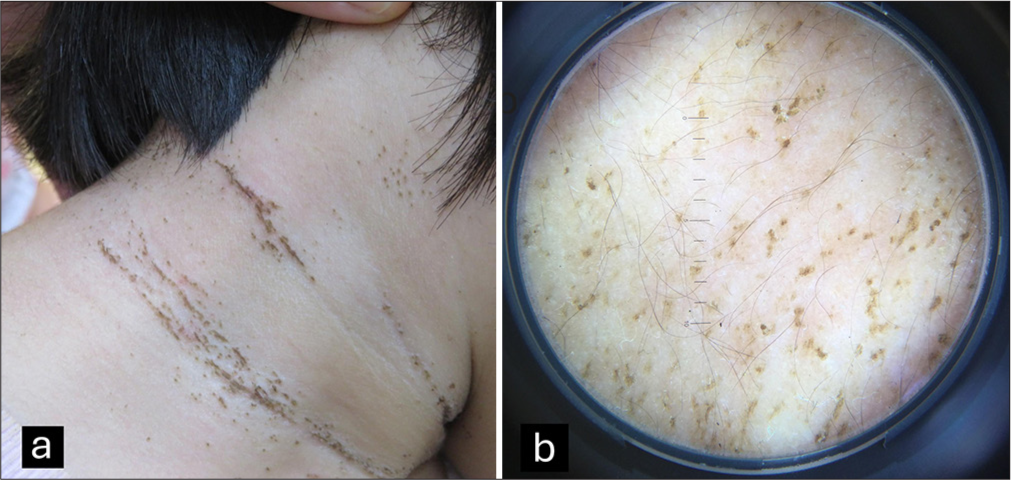
- (a) Multiple asymptomatic hyperpigmented, dirty-appearing papules and plaques in a linear arrangement on the neck. (b) Dermoscopy revealed dark brown clods and scales resembling cornflakes, arranged in a linear pattern.
DISCUSSION
TFFD is often confused with other acquired disorders that present with hyperpigmented, dirt-like lesions. Its typical distribution occurs in flexural areas, though it can affect any body site, appearing as patches, plaques, or hyperkeratotic nodules.
Dermoscopic examination reveals characteristic brown polygonal plate-like scales arranged in a cobblestone pattern,[2] though these features may not always be present. However, TFFD, DN, AN, and other hyperpigmented conditions may be clinically and dermoscopically similar [Table 1]. Palaniappan et al. presented the largest case series on DN, highlighting that the most frequently affected site was a recent surgical site, in contrast to the typical locations observed in TFFD, which commonly involves the face, neck, umbilicus, and ankle.[3] A hallmark of TFFD is its response to the alcohol swab test, also known as the Skin Modified by Alcohol Rubbing Test, where lesions are removed with 70% isopropyl alcohol.[4] In contrast, DN resolves with soap and water.
| Dermatosis neglecta | Terra firma-forme dermatosis | Acanthosis nigricans | Dirty neck syndrome | |
|---|---|---|---|---|
| Soap-water test | + | – | – | – |
| 70% isopropyl alcohol test | + | + | – | – |
| Wood’s light | - | Chalk-white fluorescence[6] | – | – |
| Dermoscopy | Cornflake-like waxy scales | Plate-like scales in a mosaic pattern; “stone pavement” pattern | Clods with crista cutis | Not reported |
The pathogenesis of TFFD remains unclear, though it is considered a keratin-retention disorder. Contributing factors include occlusive topicals, poor hygiene, sun exposure, and Malassezia spp. colonization.[1] There is also evidence suggesting a link between TFFD and atopy, as a defective epidermal barrier may possibly delay keratinocyte maturation, and excessive moisturization may further impair keratinocyte detachment.[5] In contrast, DN results from inadequate skin cleansing, leading to the accumulation of sebum, sweat, keratin, and debris. Palaniappan et al. proposed a comprehensive diagnostic algorithm that could be used as a diagnostic tool when encountering dirt-like lesions.[7]
CONCLUSION
Therefore, it is not always a result of the worsening of their condition when patients with atopic dermatitis develop skin issues. If moisturizing creams and steroids show no effect, the differential diagnoses mentioned above should be considered. Herein, we recommend using the soap-water test as an initial step to rule out DN for hyperpigmented, dirt-like lesions on the neck. If the lesion remains, a 70% isopropyl alcohol test serves as a straightforward clinical tool to confirm a diagnosis of TFFD. Should both tests yield negative results, other hyperpigmented conditions should be considered.
Acknowledgments
We would like to thank Andre Yanchen Yeh for editing and reviewing this manuscript for English language.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopy in terra firma-forme dermatosis and dermatosis neglecta. Int J Dermatol. 2017;56:1481-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatosis neglecta: A retrospective study at a tertiary care center in southern India. Indian J Dermatol. 2023;68:62833.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive methods to establish the diagnosis of terra firma-forme dermatosis: The SMART (skin modified by alcohol rubbing test) evaluation and dermoscopy. Dermatol Online J. 2016;22 doi: 10.5070/D3226031331
- [CrossRef] [Google Scholar]
- Terra firma-forme dermatosis-more than just dirty. Indian Dermatol Online J. 2023;15:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Chalk-white fluorescence under Wood light in a case of terra firma-forme dermatosis. Clin Exp Dermatol. 2021;46:165-6.
- [CrossRef] [PubMed] [Google Scholar]






