Translate this page into:
Suture materials – Recent advances

*Corresponding author: Ravi Kumar Chittoria, Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. drchittoria@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Chittoria RK, Reddy BP. Suture materials – Recent advances. CosmoDerma. 2023;3:175. doi: 10.25259/CSDM_176_2023
Abstract
A surgical suture, also known as a suture, is a medical device used to hold body tissues together and to hold wound edges together after injury or surgery. Surgical sutures are used to facilitate the closure and healing of surgical or traumatic wounds by holding tissues together to facilitate the healing process. There are many different types of suture materials for medical purposes, and the main types are absorbable and non-absorbable. Recently, there has been an increase in the development of classes of suture materials based on their properties and abilities to improve tissue convergence and wound closure. This review describes and discusses current and emerging trends in suture technology, including knotless needle sutures, antimicrobial sutures, bioactive sutures such as drug-eluting and stem cell sutures, and smart sutures, including elastic and electronic sutures. These newer strategies expand the versatility of sutures from being used only as a physical unit that brings opposing tissues closer to a more biologically active component that allows the delivery of drugs and cells to the desired location, with enormous potential for both therapeutic and diagnostic use.
Keywords
Sutures
Antimicrobial sutures
Drug-eluting sutures
Barbed sutures
Smart sutures
INTRODUCTION
The surgical suture, also known as a suture, was a medical device used to hold body tissues together and to hold wound edges together after injury or surgery. It is well known that sutures were an effective and critical part of surgery and trauma management. The purpose of sutures is to hold the respective tissues together, which facilitates and accelerates the healing process so that there is minimal or no scarring after an injury or surgical procedure.[1] Various materials were used as sewing material, such as gold, silver, iron-steel thread, dried animal intestines, animal hair (e.g., horse hair), silk, tree bark, and plant fibers (e.g., flax, cotton) earlier, although some are still in use.[2] The recent past has witnessed the use of several synthetic biomaterials such as polydioxanone and poly(lactic-co-glycolic acid) as a suture material. However, despite the wide variety of suture materials available, there is no single suture material that is suitable for all types of surgical and medical requirements.
An ideal suture material can be used for any purpose and is characterized by:
Good handling properties
Good node security
Good traction
Must be sterile
Should not be an electrolyte
Should be non-ferromagnetic
Non-capillary
Without allergy
Non-carcinogenic
Does not provide an environment for the growth of bacteria
Resists contraction
Absorbed with minimal tissue reaction
Easy to sterilize without changing its properties
Economical to use.[1]
Despite advances and innovations in material technology and surgical techniques, wound closure after surgical procedures or trauma generally still requires the use of sutures.[3] Some suture materials that have been available for decades are still routinely used. The surgical suture segment of the healthcare industry is growing significantly, with market share even in absorbable and non-absorbable suture products.[4] The demand for suture materials is increasing due to the increasing number of surgical procedures performed worldwide, regardless of the availability of suture substitutes such as surgical staples, adhesives, and tapes in the market. These products sometimes lack the stability and flexibility that sutures provide in wound care.[5,6]
The choice of suture material in wound care depends largely on factors such as the number of tissue layers involved in wound closure, wound tightness, depth of suture placement, swelling, expected suture removal time, adequate strength, and minimal or no inflammatory response.[7] Seams most also have considerable flexibility and flexibility to achieve better handling characteristics when sewing. In addition, ease of knot placement, high knot security, and absence of irritants or adhesives are also highly desired characteristics.[1,8,9] Suture materials available for routine use meet most, but not all, of the primary requirements. Therefore, current efforts are focused on the development of suture materials that have all the desired characteristics and additional properties, for example, any type of suture can be contraindicated in wounds that are contaminated, relatively old, or with a higher risk of infection when closed with stitches, such as small bites on the arms or legs, puncture wounds, or speeding missile wounds.
Newer suture materials and designs have expanded the range of biomedical applications of sutures. Emerging advances and emerging trends in suture technology hold tremendous potential for clinical/surgical applications involving specialty procedures and wound care.
The purpose of this article is to provide an overview of currently available sutures, the characteristics, and properties of suture materials, with an emphasis on emerging trends such as sutures containing bioactive molecules (drugs, antimicrobials, and stem cells) and smart sutures. An extensive literature search was conducted using electronic databases such as PubMed, Scopus, and www.clinicaltrials.gov for studies or reports on different types of sutures published up to the end of September 2020. Search terms used in these databases include “sutures,” “suture materials,” “antimicrobial sutures,” “antibacterial sutures,” “surgical site infection,” “drug-eluting sutures,” “stem cell sutures,” “bioactive sutures,” “barbed sutures,” “bioactive barbed wires,” and “elastic sutures.”
These terms were used either independently or in various combinations. Articles searched were limited to articles published in English only. Articles were then collated and examined for relevance and evidence. In addition, articles cited in the reference lists of the searched and selected articles were included in the study. Any studies or reports that lacked evidence to support the conclusions presented in the publications were excluded from the review.
MISCELLANEOUS SUTURES
Liquid stitch
It is also known as “tissue glue” or “liquid sutures” – to close both large and small wounds, such as wounds, incisions made during laparoscopic surgery, and wounds on the face or groin. Cyanoacrylate is the general name for cyanoacrylate-based fast adhesives such as methyl 2-cyanoacrylate, ethyl 2-cyanoacrylate (commonly sold under brand names such as Superglue and Krazy Glue), and n-butyl cyanoacrylate. Skin adhesives such as Indermil and Histoacryl were the first medical tissue adhesives used and are composed of n-butyl cyanoacrylate. They worked well but had the disadvantage of having to be refrigerated because they were extrathermic, so they would sting the patient and the dressing was delicate. Today, a longer chain polymer, 2-octyl cyanoacrylate, is an affordable medical-grade adhesive. It is available under several brand names, including LiquiBand, SurgiSeal, FloraSeal, and Dermabond. Their advantage is that they are more flexible, form a stronger bond, and are easier to use.
Disadvantages of surgical glue
Surgical glue costs more than sutures. Some people are allergic to it. The glue cannot be used if you have an increased risk for slow wound healing (this occurs with diabetes and other health conditions).
Advantages of surgical glue
Minor infections
Less time in the operating room
Less scars
No needles or stitches (kid-friendly)
Faster return to work and other activities such as sports
Non-removable stitches
Steri-Strips
Wound closure strips are porous strips of surgical tape that can be used to close small wounds. They are placed over the wound so that it pulls the skin on both sides of the wound together. Wound closure strips can be used instead of sutures (stitches) for some wounds because they reduce scarring and are easier to treat. The porous fabric of Steri-Strips allows more fresh air into the wound and prevents skin from soaking. Plastic or other non-porous dressings often prevent sweat and other body fluids from drying and are more likely to cause the wound to soak, thus increasing the risk of bacterial or fungal infection. Sterile strips cause less scarring compared to staples or stitches. They offer less chance of infection than sutures or staples.
PHYSICAL AND STRUCTURAL CHARACTERISTICS OF SUTURE MATERIALS
The main characteristics and properties that affect the performance of different sutures are filament structure, size, degradation properties, tensile strength, surface texture, stiffness, and material flexibility. The resistance of sutures to tissue-induced tension and repair capacity is directly related to the size and tensile properties of the suture material[1] [Figure 1]. The tensile strength of the suture material should balance the tensile strength of the tissue to improve healing. The tensile strength of suture materials can vary according to their size and is measured by the mass required to break the suture (kg). The tensile strength of the suture material also depends on the number of filaments (monofilament or multifilament).[7] Multifilament sutures offer high mechanical properties and considerable flexibility and elasticity than monofilament sutures.[1]
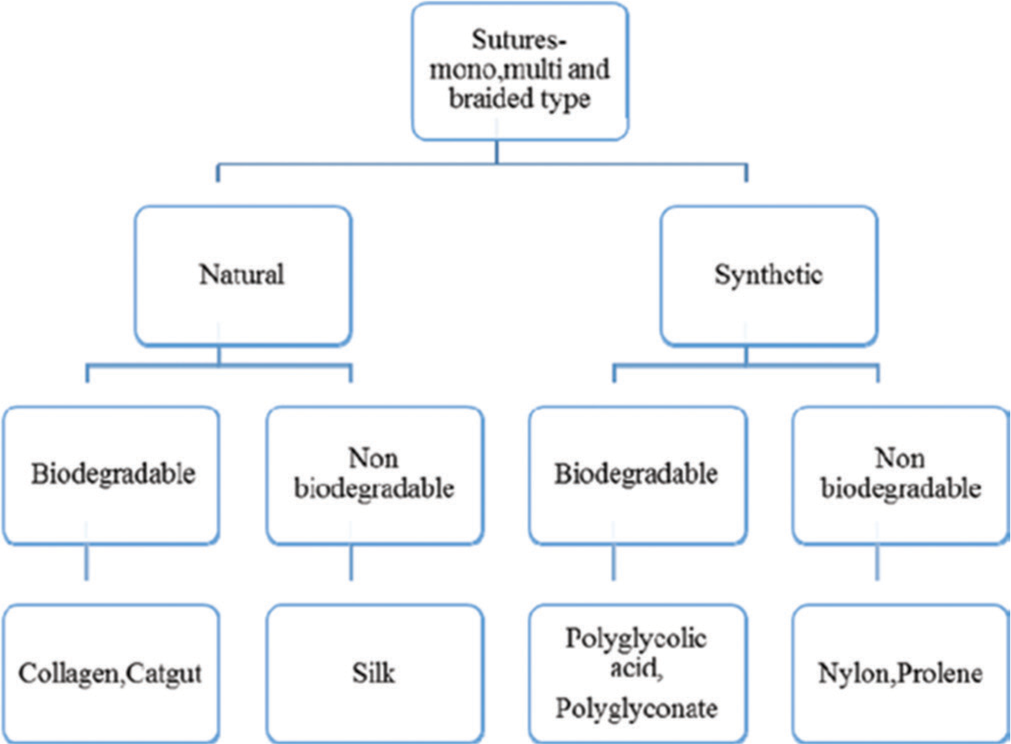
- Classification of suture materials.
RECENT AND EMERGING TRENDS
Recently, there has been an explosion in the development of sutures with additional properties, such as those modified with antimicrobial agents, bioactive molecules such as deoxyribonucleic acid (DNA), drugs, antibodies, proteins, growth factors, and silver to adapt and improve functional properties. After several years of research and development, the first antibacterial suture Vicryl Plus (triclosan-coated polyglactin 910 suture) was approved by the US Food and Drug Administration in 2002 to reduce the risk of surgical site infections (SSI). In addition, the use of triclosan coating has been extended to other suture materials to overcome bacterial adhesion and prevent or reduce SSI. Bioactive sutures can be therapeutically useful in many site-specific procedures and accelerate the healing process. The following chapters describe various emerging suture technology concepts, such as drug-eluting sutures, cell-seeded sutures, and smart sutures, to overcome post-operative wound complications, including SSI, biofilms, scarring, inflammation, and pain. These advances promise enormous potential in tissue engineering, regenerative medicine, and minimally invasive surgery [Figure 2].
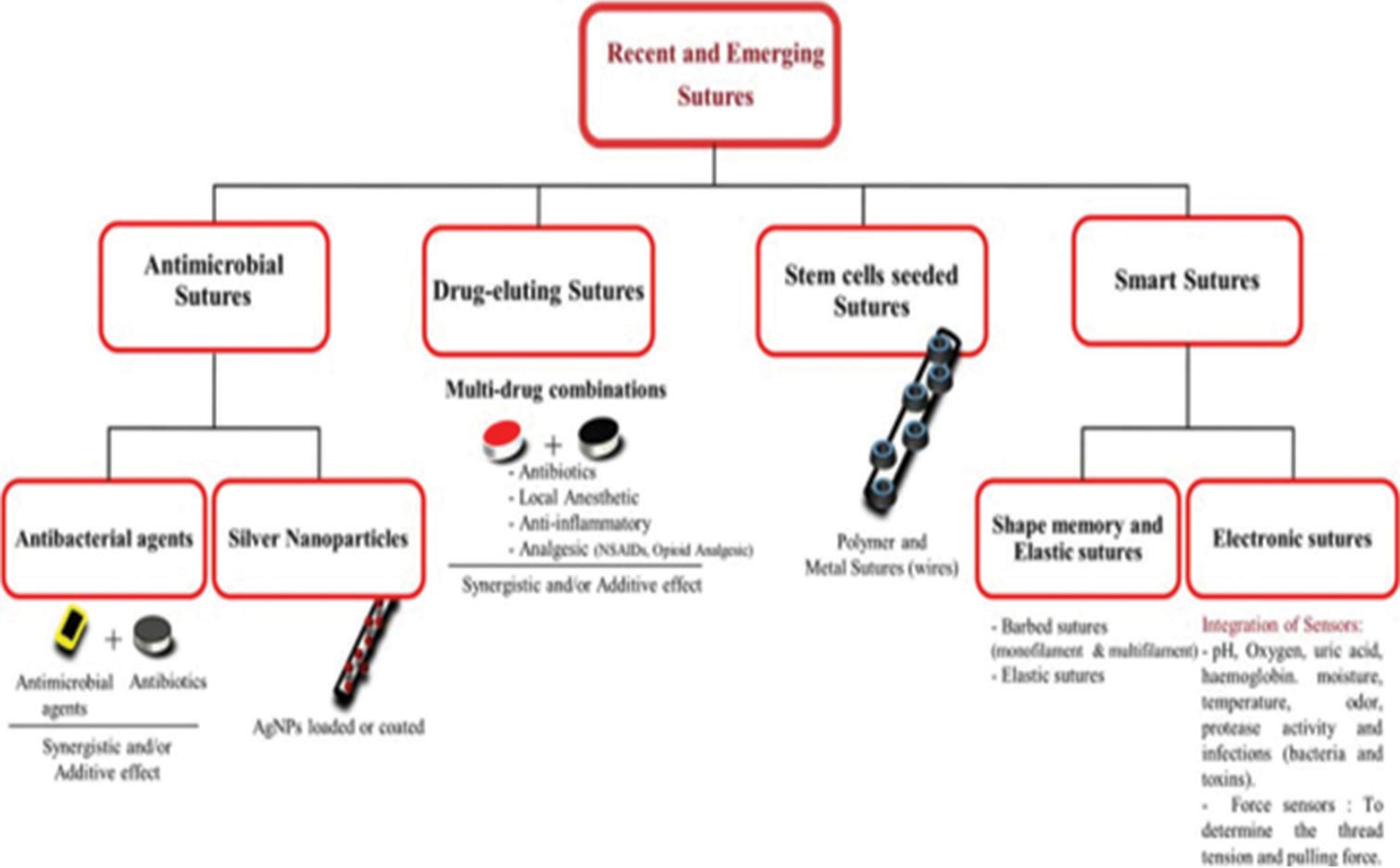
- Recent trends in sutures.
Antimicrobial sutures
Infections resulting from the attachment and proliferation of bacteria on the surfaces of devices or implants are a major problem during reconstructive procedures and the use of implantable biomedical devices. Local SSIs are the most common post-operative complications, occurring in an estimated 5% of all procedures. SSIs are generally classified into three categories: Superficial incisional, deep, and organ/ space or intracavitary infections. Staphylococcus aureus, a class of Gram-positive bacteria capable of colonizing the surface of medical implants, caused mainly 23% of SSI. Bacterial growth at the incision site is also similar to biofilm formation over sutures. Chitin (a natural polysaccharide) with antimicrobial properties can effectively accelerate wound healing and provide protection against wound infections. A recently developed diacetyl chitin-based absorbable suture formula retained 63% of its initial strength within 14 days, and complete absorption of the material was observed after 42 days with higher wound break strength and rapid tissue regeneration at the incision site in rats similar to Vicryl Plus VR. This new multifibrous suture material may support its potential use in short-and medium-length epithelial and connective tissue wound healing. Another recent study reported that oxidation plasma treatment with different suture materials by controlled etching resulted in different nanotopographies that prevented bacterial attachment to the suture surface.[8] This strategy can be used to develop cost-effective sutures with uncompromising antibacterial potential. Although a long course of antibiotics can treat bacterial infections, it is often ineffective and leads to systemic complications, including bacterial resistance to antibiotic therapy.[9] To overcome the complications associated with broad-spectrum microbial antibiotic resistance and post-operative infections at the surgical site, research has focused on identifying and modifying the organic and inorganic composition of sutures to combat or prevent infections.
Antimicrobial agent-coated sutures
Absorbable suture materials coated with antimicrobial triclosan have been introduced commercially to overcome or prevent post-operative infections.[10] Triclosan is an antimicrobial agent used commercially in many products such as soaps, deodorants, shower gels, and toothpastes due to its low antimicrobial activity and toxicity to humans. The antimicrobial activity of triclosan-coated polyglactin 910 suture (Vicryl Plus, Ethicon) was consistent across a range of suture diameters and treatment conditions, even after multiple passes through the fascia and subcutaneous tissue in a porcine model. The bacterial barrier zone surrounding ligated sutures using triclosan-coated suture material showed antimicrobial activity against Staphylococcus aureus and Staphylococcus epidermidis. In vivo studies with triclosan-coated sutures showed a significant inhibition of bacterial colonization on its surface near the infected site without compromising the mechanical properties of the suture. Polyglecapron suture containing triclosan (Monocryl Plus, Ethicon) has shown good antibacterial efficacy after implantation in animal models.
Silver nanoparticles (AgNPs) treated sutures
AgNPs are considered the best candidates for coating polymeric medical devices to improve their antimicrobial profile. The mechanism of action of the antibacterial effect of silver involves the formation of reactive oxygen species, which directly affect the DNA and cell membrane of microorganisms. In addition, bacterial resistance to AgNPs is very rare, and silver ion nanoclusters with a diameter of 1–100 nm have a high surface-to-volume ratio, which allows the use of a smaller amount with less risk of toxicity.[11] At present, AgNPs are used in medical devices such as urinary catheters and wound dressings for burns. Recently, surgical sutures treated with AgNPs to prevent bacterial adhesion to their surface have attracted interest to improve aseptic wound closure at the incision site. Recently, a long-term active antimicrobial coating for surgical sutures was developed with AgNPs and hyperbranched polylysine. The poly(glycolic acid)-based suture was coated by the immersion method, and the coated surface was highly effective against S. aureus, reducing bacterial adhesion by more than 99.5% without cytotoxicity to fibroblast cells than the uncoated suture. In another study, coating AgNPs (0.5%) on sutures showed effective antimicrobial activity and reduced bacterial adhesion of Staphylococcus aureus and Escherichia coli. In another study, AgNP-coated suture had both antibacterial and anti-inflammatory effects. In addition, an in vivo study in mice investigated intestinal anastomotic healing by significantly increasing collagen accumulation and significant mechanical properties of the anastomotic tissue.
Drug-eluting sutures
Depending on the type of therapeutic agent used, drug-eluting sutures can reduce post-operative complications such as SSIs and speed wound healing. It may also reduce the need for additional medications that may be less effective or less available at the site of the procedure after systemic administration. Sustained release of drugs at a specific site can allow therapeutically significant concentrations locally for extended periods of time without exceeding the toxicity threshold in the systemic circulation. Drug-eluting sutures are developed using a variety of methods, including coating the suture surface using a dipping method, grafting, or electrospinning. The challenge of fabricating a drug-eluting suture is to achieve the required drug concentration and efficacy without compromising the important mechanical properties of the suture, and this can be achieved through strategies to enhance polymer degradation and controlled drug release. Braided sutures are prone to bacterial adhesion and the tendency for bacteria to become trapped in the braided filament is quite high. Braided silk sutures have a higher risk of SSIs because they are more susceptible to bacterial attachment. Tetracycline-coated silk suture showed greater antimicrobial activity against E. coli than S. aureus, and the antimicrobial efficacy improved with drug concentration. In addition, braided silk sutures coated with a mixture of levofloxacin chloride and poly (ε-caprolactone) showed similar results to tetracycline, which was more sensitive to E. coli than S. aureus, acceptable in vitro cytotoxicity to porcine endothelial cells, and higher average node voltage. Static and dynamic suture friction and flexural stiffness changed during antibacterial treatment. Drug-eluting sutures containing levofloxacin-loaded poly(L-lactic acid) and polyethylene glycol prepared from biocompatible polymers with a hydrophilic polymer (microfiber) for the use in ophthalmic surgery inhibited bacterial growth S. epidermidis and infection rate in rats. Vancomycin grafted onto polypropylene suture with acrylic polymer by ionic interaction with acrylic acid moieties but not by covalent immobilization through glycidyl groups of glycidyl methacrylate reported sustained release of the drug. The potential of drug-eluting sutures can be broadened by fabricating sutures with multiple drugs, in combination that can exhibit synergistic and/or additive effects on the desired site with limited payload.[12] The fabrications can be extended to produce drug-eluting braided suture with high tensile strength, flexibility, and better handling characteristics along with sustained release of drugs. Conversely, complications such as delayed wound healing, severe scar formation, and skin irritations in barbed sutures warrant more clinical studies, and the need for modifications with bioactives can widen its functionality and reduce the adverse effects.[13] Bioactive sutures with a wide range of bioactive molecules and their possible combinations can be placed in the needle corners or elongated body of monofilament and multifilament sutures to extend its function and therapeutic effect.
Stem cells seeded sutures
Biodegradable scaffolds are widely used in tissue engineering and regenerative medicine as a carrier to transplant and differentiate stem cells into various tissues. Recent studies revealed that sutures coated with growth factors or stem cells could be used as a mode of delivery for these biological components to the desired site. Sutures with bioactive surface provide desirable tensile property and degradation rate for rapid tissue regeneration after implantation.[14] The primary objective of stem cell seeded suture is to increase the number of these cells at the injured site to accelerate tissue regeneration and repair. Although, suture-based cell delivery appears to be a feasible approach to transplant stem cells into the soft tissues of the body, retaining the desired mechanical and physical properties of such sutures would be a major challenge.
Recently, a novel stem cells seeded biological suture material for use in cardiac surgery/tissue was developed. The human mesenchymal stem cell seeded suture material was developed by loading with quantum dot nanoparticles to track the seeded cells within the myocardium. It was found that the cell-seeded biological suture was able to deliver the stem cells to the heart more efficiently than the conventional manner (injection), illustrating a greater efficiency in the transplantation of stem cells in soft tissues in rats, and reduction in fibrosis with the increased mechanical function of the heart was reported. In another study, biosuture developed from adipose-derived stem cells (ASCs) suppressed local acute inflammation in the tracheal anastomosis.[15] The previous reports on the use of stem cells coated biosutures in colonic anastomosis showed no effect in anastomotic healing, whereas, in colonic anastomosis with peritoneal installation of icodextrin 4% (adhesion-free environment), biosutures displayed more resistance than conventional sutures.[16] More recently, Juan Wang et al. reported that biodegradable suture filled with ASCs showed equal distribution of cells across the filament with improved viability and increased metabolic activity of cells with release of cytokines from in vitro wound healing assay.[17] Furthermore, sutures modified with mesenchymal stem cells showed abundant deposition of collagen alpha-1(I) chain with rapid recovery on wound healing.
Smart sutures
Shape-memory and elastic sutures
Newly developed thermoplastic polyurethane elastic sutures are feasible and safe for midline laparotomy wound closure with promising tensile characteristics to prevent post-operative complications like burst abdomen after abdominal surgery. Elastic sutures showed significant material strength with a mean elastic elongation of 56% after 10 cycles. The development of smart sutures from shape-memory polymers (SMP) can replace conventional sutures using self-tightening wound closures, reducing complexity for surgeons, especially during keyhole surgery. SMPs are able to return from a deformed state (temporary shape) to the original state (permanent) on stimulation of external energy such as heat, light, solution, and magnetic or electric field.[18] Smart sutures are pre-stretched smart material filament (temporary shape) above a critical temperature and placed into a temporary shape by cooling below the critical temperature. The suture attaches loosely to wounds under controlled tension. Stimulation above a critical temperature point restores the suture to its original state and shape, with some tension in the surrounding tissues.[19] In this way, it is easier for the spikes to change their shape when the temperature rises, either in body conditions or using an external source. Smart sutures provide high flexibility and elasticity and important mechanical properties to form a self-tightening knot for effective wound closure. Recently developed flexible thermoplastic polyurethane sutures are feasible and safe for midline laparotomy wound closure with promising properties to prevent postoperative complications such as abdominal dissection after abdominal surgery. The elastic joints showed significant material strength and the average elastic elongation was 56 × 10 cycles.
Electronic sutures
Electronic sutures that can monitor, recognize, and activate typical biological responses in the body would be very useful to improve local tissue health monitoring.[20] The suture material was designed in the shape of a snake, and the model has two silicon and platinum nanofilm temperature sensors and a gold microheater. Electronic suturing can accurately measure the high temperature, which can be used to detect the infection situation and also help maintain the ideal temperature and support the healing process with the help of micro-heaters at the wound. The fabricated electronic suture was highly flexible, facilitating effortless threading of surgical needles with significant traction and knots without degrading the device in the mouse.
CONCLUSION
Surgical sutures play an essential role as a medical device in wound care, and recent advances have expanded its applicability and effectiveness. Important advances in this field can be attributed to the technological development of material science. Polymers have significant potential due to their high flexibility, resulting in various suture materials with excellent physical and mechanical properties. In addition, biodegradable polymers that cannot be easily degraded and excreted or reabsorbed without removal or surgical revision have proven useful. These materials are also known for their ability to carry drugs, stem cells, proteins, peptides, antibodies, DNA, nanoparticles, and so on to the desired location, increasing the therapeutic potential of the threads. The main function and efficiency of sutures depend on the physical-mechanical properties, and the preservation of these properties is crucial when they are modified or covered with bioactive substances and sensors. In addition, it should also be non-carcinogenic, non-toxic, allergen-free, and most importantly, should not cause adverse reactions in host tissues to achieve better processing properties and desired modifications. To meet these requirements, detailed preclinical studies and evaluation of the safety and efficacy of these new sutures in human trials are needed. Next generation suture materials, the result of multidisciplinary efforts, have enormous potential to influence surgical outcomes and wound care.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ethicon Inc. 2005. Available from: https://www.uphs.upenn.edu/surgery/Education/facilities/measey/wound_sclosure_manual.pdf [Last accessed on 2014 Dec 12]
- [Google Scholar]
- Advances in suture material for obstetric and gynecologic surgery. Rev Obstet Gynecol. 2009;2:146-58.
- [Google Scholar]
- The use of barbed sutures in obstetrics and gynecology. Rev Obstet Gynecol. 2010;3:82-91.
- [Google Scholar]
- Surgical sutures, market size, share, analysis and forecast 2022-2028 Intelligence market report. 2022. Available from: https://www.mordorintelligence.com/industry-reports/surgical-sutures-market [Last accessed on 2015 Aug 19]
- [Google Scholar]
- Demand for surgical sutures high: Rise in surgical procedures performed globally. 2013. Available from: https://com/en/pharmaceuticals-news/item/540-demand-for-surgical-sutureshigh.html [Last accessed on 2015 May 19]
- [Google Scholar]
- Surgical knot tying manual. 2008. (3rd ed). Ireland: Covidien; Available from: https://com/imageserver.aspx?contentid=11850&contenttype=application/pdf [Last accessed on 2014 Feb 13]
- [Google Scholar]
- Suture choice and other methods of skin closure. Surg Clin North Am. 2009;89:627-41.
- [CrossRef] [PubMed] [Google Scholar]
- Biomaterials science: An introduction to materials in medicine In: Applications of materials in medicine and dentistry. United States: Academic Press; 1996. p. :356-9.
- [CrossRef] [Google Scholar]
- Evaluation of suture abrasion against rotator cuff tendon and proximal humerus bone. Arthroscopy. 2008;24:329-34.
- [CrossRef] [PubMed] [Google Scholar]
- Factors relating to the volume of surgical knots. Int J Gynaecol Obstet. 1989;30:355-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tissue reactions to modern suturing material in colorectal surgery. Bull Exp Biol Med. 2007;143:767-70.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing wound complications: A clinical and experimental study. Ann R Coll Surg Engl. 1983;65:71-7.
- [Google Scholar]
- Capillary activity of surgical sutures and suture-dependent bacterial transport: A qualitative study. Surg Infect (Larchmt). 2005;6:377-83.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial adherence around sutures of different material at grafted site: A microbiological analysis. Materials (Basel). 2019;12:2848.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of adipose-derived stem cells on full-thickness skin grafts. . 2016;2016:1464725.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of hyaluronic acid added to suture material and its relationship with bacterial colonization: An in vitro study. J Int Soc Prev Community Dent. 2018;8:391-5.
- [CrossRef] [PubMed] [Google Scholar]
- Physical and mechanical evaluation of five suture materials on three knot configurations: An in vitro study. Polymers (Basel). 2016;8:147.
- [CrossRef] [PubMed] [Google Scholar]
- Smart surgical sutures using soft artificial muscles. Sci Rep. 2021;11:22420.
- [CrossRef] [PubMed] [Google Scholar]






