Translate this page into:
Intradermal radiofrequency treatment for stubborn acne scar

*Corresponding author: Madhuri Agarwal, Department of Dermatology, Yavana Academy of Aesthetic Medicine, Yavana Aesthetics Clinic, Mumbai, Maharashtra, India. drmadhuri@yavana.in
-
Received: ,
Accepted: ,
How to cite this article: Agarwal M, Lodha A. Intradermal radiofrequency treatment for stubborn acne scar. CosmoDerma. 2023;3:176. doi: 10.25259/CSDM_212_2023
Abstract
Atrophic acne scars are common sequelae of acne, which can be disfiguring and cause emotional distress in many people because they mainly affect the face and are constantly present in their everyday lives. There are various procedural and surgical treatments available, each with its own limitations. It can be very difficult to perform subcision or punch excision in cases with multiple deep atrophic scars, and lasers may not be very effective in uplifting the rolling scars. Hence, we performed intradermal radiofrequency (RF) in our patients with stubborn scars. The RF energy was delivered while performing subcision in all the scars, which helped in collagen remodeling and improving the scars.
Keywords
Atrophic acne scars
Subcision
Intradermal radiofrequency
INTRODUCTION
Atrophic acne scars are caused by inadequate collagen formation during the normal wound-healing process after an inflammatory reaction to acne. Atrophic scars are of various subtypes, and procedural treatments such as CROSS trichloroacetic acid (TCA), dermaroller, ablative lasers, non-ablative lasers, microneedling radiofrequency (RF), subcision, and tissue augmentation have been implicated for these scars.[1] Despite these several treatment modalities, there are still some stubborn scars that do not improve. These tenacious scars frequently have fibrous strands tethering to the subcutis that lasers will not target. Hence, for such scars, we performed intradermal RF.
We treated three patients who had resistant acne scars with this modality. Clinical photos were taken using a Canon SLR camera, and standardized settings were used as the assessment tool. We preferred using Goodman and Baron’s scoring systems to assess acne scar severity and to evaluate the efficacy of the treatment. Goodman and Baron’s quantitative score allots points to each category based on the scar type and number of scars. The score would range from a minimum of 0 to a maximum of 84 points [Table 1], whereas the qualitative score is based on scar morphology with grade 1–4 [Table 2].[2,3]
CASE 1
A 24-year-old female, who had previously been treated for acne, had numerous acne scars on her face. We performed three sessions of microneedling RF with good clinical improvement, but some scars lingered. On cutaneous examination, there were different types of atrophic acne scars on the cheeks, including mainly box scars, rolling scars, and a few erythematous macular and ice-pick scars. These scars would not flatten after manual stretching. Goodman and Baron’s qualitative scoring was grade 4 and quantitative was 37 in this case. We performed two sessions of intradermal subcisional RF at monthly intervals. This helped in releasing the fibrous bands pulling on the scars. There were no adverse events.
| Grade | Number of lesions | ||
|---|---|---|---|
| 1–10 | 11–20 | >20 | |
Milder scarring (1 point each)
|
1 | 2 | 3 |
Moderate scarring (2 points each)
|
2 | 4 | 6 |
Severe scarring (3 points each)
|
3 | 6 | 9 |
| Papular scar | 2 | 4 | 6 |
Hyperplastic:
|
Area 5 mm 6 |
Area 5–20 mm 12 |
Area 20 mm 18 |
| Grade | Characteristics |
|---|---|
| Grade 1 | Macular scarring |
| Grade 2 | Mild atrophy/hypertrophic scarring that might not be evident at 50 cm or greater and is masked easily with makeup or hair patterns |
| Grade 3 | Moderate atrophy/hypertrophic scarring, visible at social distances of 50 cm or more and is not covered easily by make-up but gets flattened by manual stretching of the skin |
| Grade 4 | Severe atrophic or hypertrophic scarring, visible at social distances of 50 cm or more and is not covered easily by makeup and does not get flattened by manual stretching of the skin |
CASE 2
A 27-year-old woman with several atrophic acne scars underwent three sessions of microneedling RF and two sessions of fractional carbon dioxide laser therapy with us. Although the scarring was reduced, she was concerned about a few pitted scars and rolling scars that were still evident. We performed two sessions of subcisional intradermal RF in one month’s interval.
CASE 3
A 23-year-old student had grade 3 acne and atrophic acne scars. She was treated with oral isotretinoin for three months following which her acne was resolved, but her underlying scars became more apparent. Since she had many rolling and box scars, we performed an intradermal RF procedure. We observed a substantial reduction in acne scars with one sitting.
The RF energy is a non-ionizing electromagnetic radiation that diminishes elastotic materials and promotes neocollagenesis.[4] This RF energy is generated in the non-insulated tip (1 mm) of the intradermal cannula, which helps in precisely delivering energy to the desired target [Figure 1]. The intradermal cannula electrodes are of sizes 21 and 27 gauge. The complete intradermal cannula is insulated with a biocompatible parylene layer with only the distal 1 mm left exposed to function as the electrode in the tissue. A monopolar RF device was used for the procedure, which had a grounding pad attached to the patient to complete the circuit. We created a small tunnel adjacent to the scar with an 18-gauze needle after infiltration of local anesthesia. We opted for intradermal RF treatments at 18 W (level 5 at 1 MHz), employing a 21-gauge cannula electrode coated with insulation. The 21G intradermal cannula is inserted through this tunnel in both superficial and deep planes and was moved back and forth and in a fanning fashion under the scars to release fibrous bands. Multiple passes of irradiation were performed on each side of the scars using a fanning technique. We performed intradermal RF at two levels: Superficial (below the individual scar) and deep (upper subcuticular) to cause disruption of fibrotic bands in the superficial plane and generate new collagen in the deep plane. Intradermal RF emits uniform heat waves to the dermis, causing immediate collagen denaturation and elastic material depletion with subsequent neocollagenesis. On the other hand, there is no new collagen formation in conventional subcision.[5] Simultaneously, these waves cause coagulation; therefore, there is no to minimal chance of hematoma as compared to conventional subcision with improvement in skin contour.[2] Post-procedure, there may be redness and swelling, which goes down in 24 h. The procedure was conducted over a span of three months with a four-week interval between sessions. All the cases were evaluated with Goodman and Baron’s qualitative and quantitative scoring before and after the treatment and clinical photographs. In case one, Goodman and Baron’s quantitative score was 37 and their qualitative score was 4, which was reduced to 14 points on the quantitative scale and to grade 2 on the qualitative scale after intervention [Figure 2 a and b]. In case two, a qualitative score of 3 and a quantitative score of 19 were reduced to scores of 2 and 8, respectively, after two sessions [Figure 3a and b]. Similarly, the qualitative score was 4, and the quantitative score was 22 in case three. It was reduced to scores of 3 and 6, respectively, after a single treatment. None of the patients experienced unfavorable ramifications.
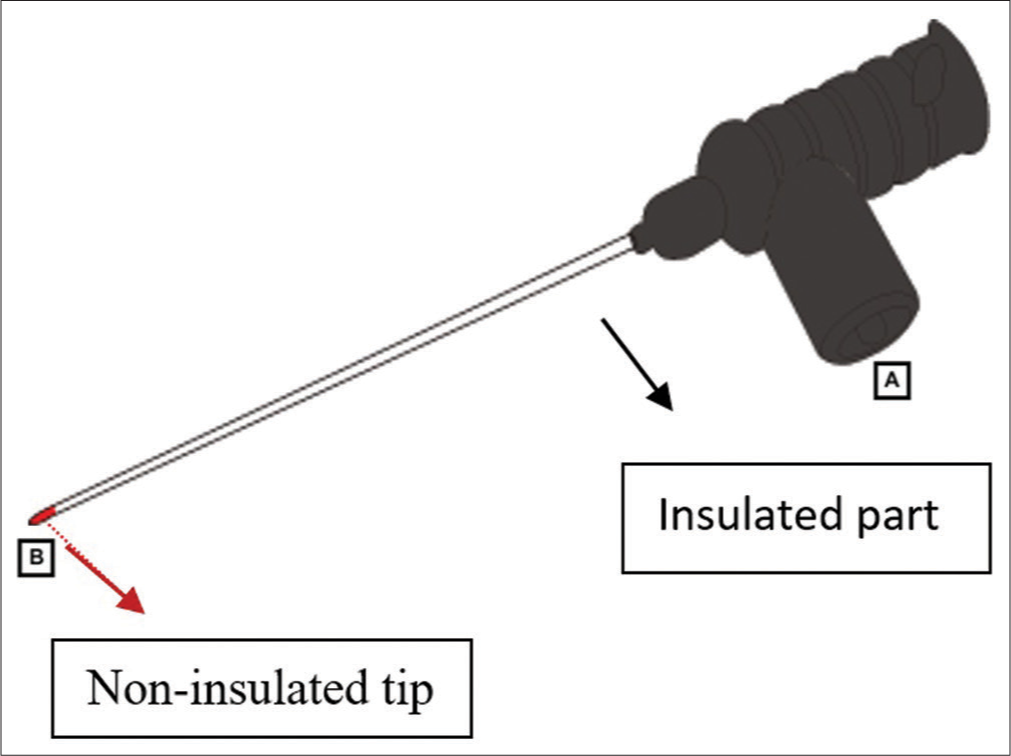
- 21G cannula used in procedure. Point A: The part for input energy from mainboard. Point B: The part for output energy. Inside black plastic, there is a connection port to point A and cannula. The energy coming from point A is delivered to cannula. The cannula is coated (semi-insulated), so radiofrequency energy is emitted only at the end of the cannula, i.e., Point B.
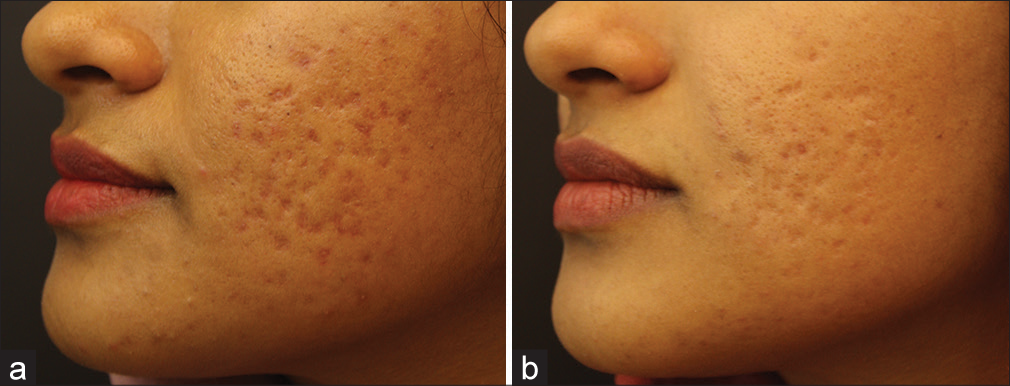
- (a) Before the first session of intradermal radiofrequency. (b) After the two intradermal radiofrequency session result seen in scar reduction.

- (a) Acne scars seen before the start of intradermal radiofrequency (b) There is significant reduction in acne scars and improvement in skin texture after two sessions of intradermal radiofrequency.
DISCUSSION
Acne scars are a complex and ubiquitous condition, and they have a psychosocial and emotional impact on many individuals. About 90% of acne sufferers have some acne scarring when examined under a bright light.[6] The treatment of atrophic acne scars varies depending on the types of scars. Dermatologists may face a therapeutic challenge due to the limitations of treatment modalities in their ability to improve scars.[7] Rolling scars are attached to subcutis with fibrous bands may show substantial improvement with ablative lasers. Conventional subcision only treats one scar at a time, does not result in collagen remodeling, and may also cause mechanical trauma and hematoma. Intradermal RF is one such minimally invasive treatment where subcision is conducted, and RF is simultaneously delivered through the scars with minimal adverse events. The RF energy reduces the elastic material, reorients the existing elastic material, and induces collagen production. Histopathological findings from animal studies also show an increase in the number of collagen bundles and elastic fibers.[5]
Kaur et al. performed RF-assisted subcision in 21 patients where five patients had 0–25% improvement, nine had 25– 50% improvement, five had 50–75% improvement, and two had 75–90% improvement.[8] The RF-assisted subcision is a novel modality, so there are no previous studies regarding its efficacy.
Two of our patients had previously been treated with different modalities and had some lingering scars, which will not improve with conventional procedures. Hence, we performed intradermal RF, which lifted the depressed scars and gave optimum results. We believe that this procedure is ideal for stubborn, adherent fibrotic scars not responsive to conventional subcision and laser. Patients may require two to three sessions depending on the severity of the acne scar, which can be repeated in four weeks.
CONCLUSION
It is a safe and effective treatment for acne scars. This treatment may be particularly helpful for patients who have not responded well to previous therapeutic options or have not achieved optimum results. A large-scale clinical study is required for a better understanding of the effectiveness of this procedure in treating acne scars.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Evaluation of microneedling fractional radiofrequency device for treatment of acne scars. J Cutan Aesthet Surg. 2014;7:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring--a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48-52.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [CrossRef] [PubMed] [Google Scholar]
- A combination trial of intradermal radiofrequency and hyaluronic acid filler for the treatment of nasolabial fold wrinkles: A pilot study. J Cosmet Laser Ther. 2014;16:37-42.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy, longevity, and safety of combined radiofrequency treatment and hyaluronic acid filler for skin rejuvenation. Ann Dermatol. 2014;26:447-56.
- [CrossRef] [PubMed] [Google Scholar]
- Disorders of sebaceous glands Rook's Textbook of Dermatology. Vol 3. (8th ed). Oxford, UK: Blackwell Scientific Publications; 2010. p. :42.1-86.
- [CrossRef] [Google Scholar]
- Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8:33-40.
- [Google Scholar]
- A split-face randomized controlled study comparing the efficacy and safety of intralesional radiofrequency-assisted subcision vs conventional subcision in postacne scars. J Cosmet Dermatol. 2020;19:1086-92.
- [CrossRef] [PubMed] [Google Scholar]







