Translate this page into:
Sorafenib-induced hand-foot skin reaction

*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government T D Medical College, Alappuzha, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nair PS, Xson C. Sorafenib-induced hand-foot skin reaction. CosmoDerma. 2025;5:30. doi: 10.25259/CSDM_11_2025
Sorafenib (SF) is an orally active multikinase inhibitor with anti-angiogenic ability and is used widely for advanced renal cellular carcinoma (RCC) and hepatocellular carcinoma. A 46-year-old man with advanced RCC was started on SF 400 mg 3 months ago and is now on the maintenance dose of 200 mg. One month ago, he noticed pain on both soles while walking. Later, he noticed a thickening of the plantar skin in pressure-bearing areas. There was no prior blistering of the plantar region. He denied any past history of callosities, corn feet or diabetes. There were no lesions on the palms. On examination, the patient had multiple well-defined yellowish hyperkeratotic plaques distributed on the heels, forefeet, and toes which were tender on palpation [Figure 1]. Some of the plaques showed erosions and deep pits. Dermoscopy was non-contributory but showed multiple longitudinal furrows and white scales [Figure 2]. The patient was not willing for a skin biopsy. We made a diagnosis of SF-induced hand-foot skin reaction (HFSR) – Grade 1. The patient was given antibiotics and 12% salicylic acid ointment. The patient showed moderate improvement after 4 weeks, with a reduction in erythema, pain, and scaling of lesions. After eight weeks, there was a 50% reduction in the lesions.

- Hyperkeratotic yellowish plaques with erosions (arrow) and deep pits (arrow).
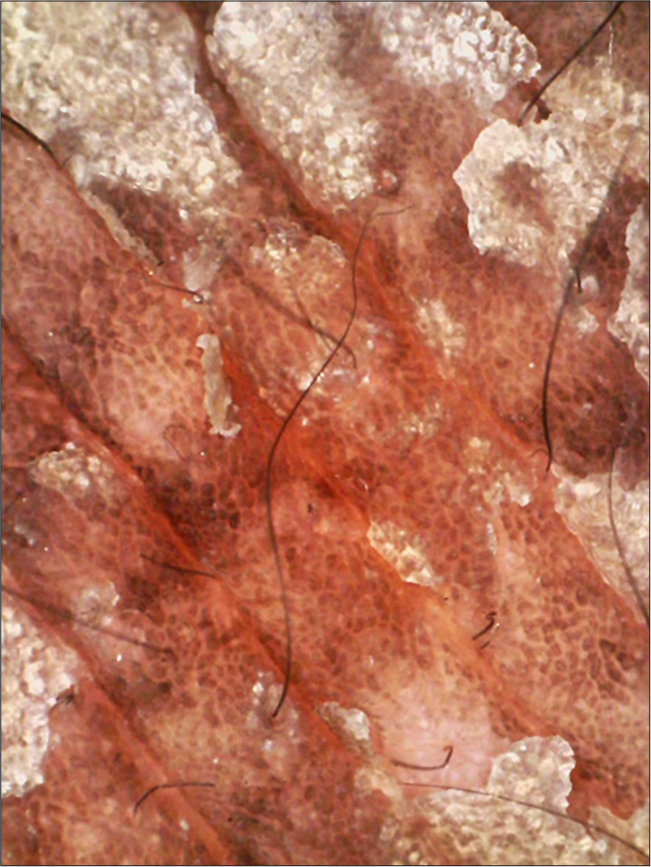
- Dermoscopy showing longitudinal furrows and white scales, non-polarizing light ×80 magnification.
HFSR, also known as palmoplantar erythrodysesthesia or Burgdorf reaction, is commonly observed with multikinase and tyrosine kinase inhibitors used for treating organ-specific advanced tumors.[1] The other drugs known to cause it are capecitabine, 5-fluorouracil, docetaxel, bleomycin, and cyclophosphamide. Previously, the term hand-foot syndrome (HFS) was denoted for this condition, but the current term is HFSR, as the presentation can be varied, such as erythema, scaling, edema, erosions, and ulcers. Even though the term used is HFSR, in some cases, only the palms or soles (as in our case) may be affected. There are three grades of HFSR: Grade 1 – erythema, pain, hyperkeratosis of palms and soles, Grade 2 – bleeding, edema, and fissures, and Grade 3 – severe pain, blisters.[2] The exact mechanism of SF-induced HFSR is not known, but it is postulated that the metabolites of SF are excreted through the sweat glands which are abundant in the palms and soles and may contribute to the hyperkeratosis.[1,2] Fortunately, HFSR is self-limited and there is no indication for stopping therapy. There are many conditions in dermatology presenting with palmoplantar keratodermas, such as psoriasis, ichthyosis, and chronic eczemas. However, these disorders present with diffuse palmoplantar keratoderma rather than localized as in HFSR, and there will be a previous history of these dermatoses. Moreover, the keratoderma in HFSR is painful. Histopathological findings are usually non-specific. Massive hyperkeratosis, irregular acanthosis, and lymphocytic infiltrate in the dermis are reported findings.[3] There are no dermoscopic features of HFSR reported in the literature, and hence, our findings of longitudinal furrows and scales cannot be further elaborated. However, these findings are common in any case of keratodermas. Emollients, keratolytics, and topical steroids are the therapeutic options. Reports say that they have only symptomatic relief, and no duration of therapy is mentioned anywhere.[1-3]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Hand-foot skin reaction induced by sorafenib in a hepatocellular carcinoma patient. Postgrad Med J. 2020;96:495.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous adverse reactions of chemotherapy in cancer patients: A clinicoepidemiological study. Indian J Dermatol. 2018;63:41-6.
- [CrossRef] [PubMed] [Google Scholar]
- Chemotherapy-induced hand-foot syndrome and nail changes: A review of clinical presentation, etiology, pathogenesis, and management. J Am Acad Dermatol. 2014;71:787-94.
- [CrossRef] [PubMed] [Google Scholar]





