Translate this page into:
Role of Q-switched neodymium-doped yttrium aluminum garnet laser in combination with fractional carbon dioxide laser for the treatment of onychomycosis

*Corresponding author: Komal Sharma, Department of Dermatology, Healing Super Speciality Hospital, Chandigarh, India komal30591ks@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dhawan S, Sharma K. Role of Q-switched neodymium-doped yttrium aluminum garnet laser in combination with fractional carbon dioxide laser for the treatment of onychomycosis. CosmoDerma. 2024;4:85. doi: 10.25259/CSDM_98_2024
Abstract
Objectives:
Our aim was to evaluate the role and efficacy of Q-switched neodymium-doped yttrium aluminum garnet (Nd: YAG) combined with fractional carbon dioxide (CO2) laser for the treatment of onychomycosis without administration of oral antifungals.
Materials and Methods:
Twenty-five patients with onychomycosis and positive fungal cultures, who had not been on any oral antifungal for at least six months, were included in our study. The patients were treated with monthly sessions combining 1,064 nm Q-switched Nd: YAG laser, ms quasi mode, and fractional CO2 laser for six months, along with a topical antifungal. The visual analog score was calculated according to patient observation for cosmetic clearance after three and six sessions, and three and six months after completion of the laser sessions. The onychomycosis severity index (OSI) was used by the clinician at the beginning and the end of the study as a tool to measure the treatment outcome. Fungal cultures were done six months after the completion of sessions to evaluate fungal clearance.
Results:
Twenty of the 25 enrolled patients completed the study. Of these, 5 (25%) patients had complete cosmetic clearance after six sessions, and 15 (75%) patients had complete clearance at three months after completion of the sessions, which was maintained at six months. On comparing the OSI score calculated at the beginning of the laser therapy and six months after completion of laser sessions, a significant response to treatment (P < 0.001) was seen. In total, 17 (85%) patients had negative fungal cultures six months after completion of sessions proving no relapse till six months.
Conclusion:
Our study concludes that Q-switched Nd: YAG in combination with fractional CO2 laser is beneficial in the treatment of onychomycosis by destruction of fungal elements and increasing the topical drug delivery. These lasers are commonly available in dermatology practice and can be combined with oral antifungals to reduce the treatment duration.
Keywords
Onychomycosis
Q-switched neodymium-doped yttrium aluminum garnet laser
Fractional carbon dioxide laser
INTRODUCTION
Onychomycosis, a chronic and recurrent fungal infection of the nail plate, presents challenges in treatment for both patients and clinicians. Onychomycosis comprises about 50% of nail disorders, predominantly affecting older adults with diabetes mellitus, peripheral arterial disease, or immunosuppression.[1,2] Toenails are more susceptible due to limited ventilation and care.[3] Clinically, affected nails exhibit yellowish-white or brown discoloration, detachment (onycholysis), subungual hyperkeratosis, thickening (onychauxis), and increased fragility.[4,5] Occasionally, black pigmentation may occur, attributed to the Melanoides variant of Trichophyton rubrum or other fungi, termed fungal melanonychia [Figure 1].[6] Total dystrophic onychomycosis represents the most severe form, characterized by thickened, friable, and yellowish nails, often accompanied by concurrent tinea pedis [Figure 2].[4,7] Oral antifungals, such as itraconazole and terbinafine, are the gold standard treatments, although with variable degrees of improvement.[8] Effective management requires months of oral antifungal administration. Recurrence rates can be as high as 50%, and exceed 50% in clinical settings.[9] The slow growth rate of the nail plate prolongs treatment duration, decreasing patient adherence due to delayed improvement. Increased awareness prompts many patients to seek alternatives to long-term oral medication, fearing potential liver complications. In addition, the extended treatment regimen poses difficulties for geriatric patients, those on polypharmacy, and individuals with preexisting organ dysfunction. While measures such as footwear disinfection and maintaining foot hygiene and ventilation are feasible, patients with predisposing factors or immunosuppressive conditions necessitate safer and more effective treatment options.

- Fungal melanonychia.

- Total dystrophic onychomycosis accompanied with tinea pedis.
Lasers have enhanced treatment outcomes across diverse medical conditions, necessitating assessment of their efficacy in nail abnormalities. Several studies have explored the ablative potential of high-powered carbon dioxide (CO2) lasers in nail disorders since the 1980s.[10-12] However, concerns persist due to unestablished efficacy, the absence of standardized protocols, and the associated procurement costs leading to elevated treatment expenses. Furthermore, the lack of comparative studies between different laser modalities compounds these apprehensions regarding their utilization in onychomycosis.
A 2022 review by the authors of this study assessed 57 studies on laser therapy for onychomycosis.[13] Perforated CO2 lasers yielded the best outcomes followed by long-pulsed neodymium-doped yttrium aluminium garnet (Nd: YAG) lasers.
Fractional CO2 laser combined with topical antifungals and quasi long-pulse (300 ms) Nd: YAG lasers showed promise in shortening treatment duration and enhancing results. Q-switched Nd: YAG and fractional CO2 lasers are commonly available in dermatology clinics.[13-15]
Lasers operate through selective thermolysis, targeting specific tissues without affecting surrounding areas. The parameters must be finely adjusted to achieve optimal fungal destruction while preventing pain and tissue necrosis.[16] To penetrate the nail plate and surrounding skin, wavelengths between 750 nm and 1300 nm are necessary.[17] Pulse duration should be shorter than the thermal relaxation time (TRT) of the target tissue to avoid pain and necrosis. As TRT varies with the structure, thermal diffusivity, and cell wall composition, it is variable for fungal conidia, hyphae, and mycelia (3/4th and 2/3rd of the conidia, respectively). TRT is 0.7 ms; therefore, spacing between two pulses should be long enough to allow heat to dissipate to prevent pain and necrolysis of the tissue but short enough to provide enough heat accumulation for fungal tissue destruction.[8] Microsecond pulses use differences in TRTs between fungi and dermal tissue, elevating fungal temperature while maintaining dermal temperature.[16] Spot size determines tissue penetration depth, with larger spots delivering optimal energy fluence while minimizing side effects.
MATERIALS AND METHODS
Study design
A prospective observational study to evaluate the role and efficacy of 1,064 nm Nd: YAG laser combined with fractional CO2 laser in onychomycosis was conducted over a period of one year, from January 1, 2022, to December 31, 2022, in our outpatient department.
Both men and women 18 years or above of age, who gave consent for the treatment, and had positive fungal cultures and nil-to-negligible response after six or more months of oral itraconazole were included in the study. Patients with negative fungal cultures were excluded from the study. Patients with active paronychia were advised against laser treatment until resolution.
To avoid bias in clinical improvement due to the reservoir effect of oral antifungals, patients who had taken any oral antifungals in the preceding six months were not initiated with laser sessions till the lapse of six months without oral antifungals.
In total, 25 patients fulfilled the study parameters. Five of these patients were either irregular with the monthly sessions or were lost to follow-up and hence were not included in the final evaluation even if they showed any improvement during the sessions. Hence, 20 patients were included in the final analysis.
Treatment protocol
A total of six monthly sessions, combining 1,064 nm nanosecond Q-switched Nd: YAG laser, microsecond quasi mode, and fractional CO2 laser, were done.
Topical lignocaine was applied on the proximal nail fold for 45 min before each session.
The first round of laser was done with quasi (300 ms) mode of 1064 Nd: YAG laser at the highest fluences produced by this laser. The patients were informed before the session that the nails were being heated, and he/she should inform the clinician in case of discomfort. Patients with moderate-to-severe hyperkeratosis could not feel the heat; hence, the number of shots was limited to 80–100 for great toes and 50 for small toes.
The second round of laser was done with 1,064 nm Q-switched mode. Energies were adjusted according to the comfort of the patient, and patients were pre- informed about mild pricking sensation at the time of the laser.
The third round of laser was done with a 10,600 nm fractional CO2 laser to form a net of fenestrations [Figure 3 and Table 1].

- Net of fenestrations formed by carbon dioxide laser.
| S. No. | Laser/mode used | No. of passes | Laser Parameters |
|---|---|---|---|
| 1. | 1,064 nm Nd: YAG quasi mode laser | Multiple passes till heating | 6 mm spot size, 5 J/cm2 energy, frequency 5 Hz 8 mm spot size, 2.8 J/cm2 energy, frequency 5 Hz |
| 2. | Long-pulse 1,064 nm Nd: YAG laser |
a. 2–3 passes b. 5–6 passes |
6 mm spot size at 3–4 J/cm2 energy, frequency 5 Hz 8 mm spot size at 1.8–2.2 J/cm2 energy, frequency 5 Hz |
| 3. | Fractional CO2 laser | 4 passes | 30 mJ energy at 5% density |
CO2: Carbon dioxide, Nd: YAG: Neodymium-doped yttrium aluminum garnet
Photographs were taken before each session and at follow-ups after the completion of laser sessions.
The patients were advised to take the tablet paracetamol in case of pain or discomfort and were prescribed a combination of steroid and antibiotic cream twice daily for three days on the proximal nail fold to prevent post-treatment inflammation. Daily topical 2% sertaconazole nitrate lotion was continued along with laser sessions.
Measurement of response
The cosmetic response was assessed as per patient observation by the visual analog score (VAS) system after three and six sessions and three and six months after the sixth session. Results of the treatment were measured on the basis of improvement in color, decrease in the area of involvement, and decrease in the thickness of the nail plate. The VAS grading and outcomes measured are shown in Table 2.
Treatment outcome and clinical response were measured by the clinician by comparing the pre-treatment onychomycosis severity index (OSI) score with the score obtained 6 months after the completion of the laser sessions on the basis of area of involvement, proximity to the matrix, and presence of a dermatophytoma and/or >2 mm subungual hyperkeratosis [Table 3]. The OSI scores were compared using student’s t-test, and P < 0.05 was considered to be statistically significant.
Mycological cure was measured by fungal cultures performed at the six-month follow-up.
| S. No. | Improvement (%) | Grade | Improvement |
|---|---|---|---|
| 1. | 0 | 0 | No improvement |
| 2. | 0–25 | 1 | Poor improvement |
| 3. | 26–75 | 2 | Moderate improvement |
| 4. | >76 | 3 | Good improvement |
| 5. | 100 | 4 | Complete clinical clearance |
VAS: Visual analog score
| Area of involvement of nail plate (%) |
Points | Proximity to matrix | Points | Patch/streak/SH* | Points |
|---|---|---|---|---|---|
| 1–10 | 1 | Distal groove | 1 | Yes | 10 |
| 11–25 | 2 |  |
2 | No | 0 |
| 26–50 | 3 | 3 | 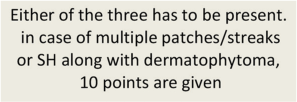 |
||
| 51–75 | 4 | 4 | |||
| >76 | 5 | Matrix involvement | 5 |
OSI: (Points for area of involvement×Points for proximity to matrix)+dermatophytoma or SH. *Dermatophytoma can be present as a patch or streak. SH: Subungual Hyperkeratosis
RESULTS
Patient characteristics
Twelve men and eight women were included in the study and had an average disease duration of 21.8 months [Table 4].
| S. No. | Age (years) |
Sex | Duration of disease (Months) | Type | Left foot nails involved | Right foot nails involved | Left hand nails involved | Right hand nails involved |
|---|---|---|---|---|---|---|---|---|
| 1. | 28 | M | 12 | WSO | 1 | 2 | 0 | 0 |
| 2. | 56 | M | 30 | DSO | 1 | 2 | 0 | 0 |
| 3. | 31 | F | 8 | DLSO | 0 | 0 | 2 | 1 |
| 4. | 83 | M | 60 | WSO | 5 | 5 | 0 | 0 |
| 5. | 48 | F | 30 | DLSO | 3 | 2 | 0 | 0 |
| 6. | 21 | M | 15 | DSO | 1 | 0 | 0 | 0 |
| 7. | 39 | F | 12 | WSO | 0 | 0 | 1 | 3 |
| 8. | 37 | M | 12 | DSO | 0 | 3 | 0 | 0 |
| 9. | 49 | M | 24 | DLSO | 1 | 0 | 3 | 2 |
| 10. | 48 | M | 48 | TDO | 5 | 5 | 0 | 0 |
| 11. | 57 | F | 12 | DSO | 1 | 1 | 0 | 0 |
| 12. | 36 | F | 20 | DSO | 0 | 0 | 2 | 1 |
| 13. | 18 | M | 15 | DLSO | 0 | 1 | 0 | 0 |
| 14. | 59 | F | 12 | DLSO | 1 | 0 | 0 | 0 |
| 15. | 81 | M | 36 | DLSO | 1 | 2 | 2 | 0 |
| 16. | 33 | F | 12 | Endonyx | 0 | 1 | 0 | 0 |
| 17. | 36 | M | 12 | DLSO | 0 | 1 | 0 | 0 |
| 18. | 64 | M | 24 | WSO | 3 | 2 | 0 | 0 |
| 19. | 52 | M | 30 | DLSO | 2 | 3 | 1 | 2 |
| 20. | 22 | F | 12 | DLSO | 1 | 1 | 0 | 0 |
DSO/DLSO: Distal subungual onychomycosis/distal lateral subungual onychomycosis. WSO: White superficial onychomycosis. TDO: Total dystrophic onychomycosis
The patients’ ages ranged from 18 years to 83 years, with an average age of 44.9 years. Twenty patients with 77 nails (n = 57 for feet and n = 20 for hands) were treated.
On examination, 14 (70%) patients had distal lateral subungual onychomycosis, 4 (20%) had white superficial onychomycosis, and 1 (5%) patient each had endonyx and total dystrophic onychomycosis [Table 4]. Of the 20 patients, 8 (40%) suffered from chronic illnesses, such as diabetes mellitus (3), hypertension (3), and rheumatoid arthritis (RA) (2). One of the patients with RA was on methotrexate for more than five years and presented with severe subungual hyperkeratosis. On fungal culture, the most commonly found organisms were T. rubrum in 13 (65%) patients and Trichophyton interdigitale in 6 (30%) patients. The patient presenting with severe subungual hyperkeratosis showed mixed infection with T. rubrum and Candida albicans.
Patient satisfaction and cosmetic response
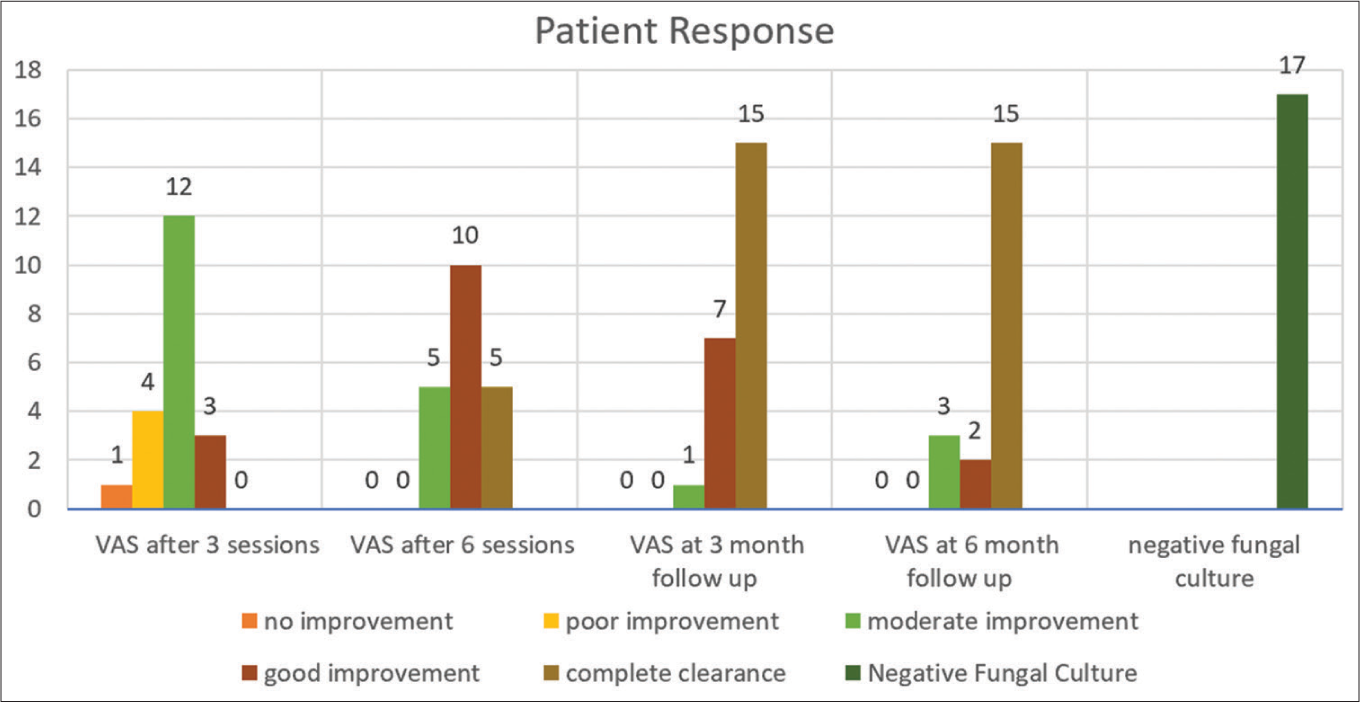
The VAS was recorded after the third and sixth sessions and three and six months after the sixth session [Table 5]. The initial improvement was first noticed near the proximal nail fold. Of the 20 patients treated, 5 (25%) showed complete cosmetic clearance after six sessions. After three months of completion of sessions, 15 (75%) patients had complete clearance with no relapses, which was maintained at six months [Table 6 and Figure 4]. Two patients had onycholytic pockets, which gradually resolved ([Figure 5], patient 1).
| S. No. | Average OSI pre treatment | OSI grading pre treatment |
VAS after 3 sessions |
VAS after 6th session |
VAS at 3 months follow-up | VAS at 6 months follow-up | Average OSI at 6 months follow-up | OSI grading at 6 months follow-up | Fungal culture at 6 months follow-up | Response |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 6.3 | Moderate | 1 | 3 | 4 | 4 | 0 | clearance | Negative | cured |
| 2. | 4 | Mild | 2 | 3 | 4 | 4 | 0 | clearance | Negative | cured |
| 3. | 5 | Mild | 2 | 2 | 4 | 4 | 0 | clearance | Negative | cured |
| 4. | 8 | Moderate | 0 | 2 | 3 | 3 | 1.67 | mild | Negative | cured |
| 5. | 6.2 | Moderate | 2 | 4 | 4 | 4 | 1 | mild | Negative | cured |
| 6. | 2 | Mild | 2 | 3 | 4 | 4 | 0 | clearance | Negative | cured |
| 7. | 4.75 | Mild | 3 | 4 | 4 | 4 | 0 | clearance | Negative | cured |
| 8. | 12 | Moderate | 2 | 3 | 4 | 4 | 0 | clearance | Negative | cured |
| 9. | 6.3 | Moderate | 2 | 3 | 4 | 4 | 2 | mild | Negative | cured |
| 10. | 28.2 | Severe | 1 | 2 | 2 | 2 | 22.4 | severe | Positive | negligible |
| 11. | 4 | Mild | 2 | 3 | 3 | 2 | 3 | mild | Positive | mild |
| 12. | 13.3 | Moderate | 2 | 3 | 4 | 4 | 0.67 | clearance | Negative | cured |
| 13. | 6 | Moderate | 3 | 4 | 4 | 4 | 0 | clearance | Negative | cured |
| 14. | 12 | Moderate | 1 | 3 | 4 | 4 | 1 | mild | Negative | cured |
| 15. | 10.75 | Moderate | 2 | 2 | 3 | 2 | 9.25 | moderate | Positive | mild |
| 16. | 6 | Moderate | 2 | 3 | 4 | 4 | 0 | clearance | Negative | cured |
| 17. | 2 | Mild | 3 | 4 | 4 | 4 | 0 | clearance | Negative | cured |
| 18. | 7.6 | Moderate | 1 | 2 | 3 | 3 | 2 | mild | Negative | cured |
| 19. | 5.9 | Moderate | 2 | 4 | 4 | 4 | 1 | mild | Negative | cured |
| 20. | 12 | moderate | 2 | 3 | 4 | 4 | 2 | mild | Negative | cured |
VAS: Visual analog score, OSI: Onychomycosis severity index
| Number of patients (percentage) n=(%) | |||||
|---|---|---|---|---|---|
| No improvement | Poor improvement | Moderate improvement | Good improvement | Complete clearance | |
| VAS after 3 sessions | 1 (5) | 4 (20) | 12 (60) | 3 (15) | 0 |
| VAS after 6 sessions | 0 | 0 | 5 (25) | 10 (50) | 5 (25) |
| Follow-up at 3 months | 0 | 0 | 1 (5) | 7 (35) | 15 (75) |
| Follow-up at 6 months | 0 | 0 | 3 (15) | 2 (10) | 15 (75) |
VAS: Visual analog score
- Bar chart showing response to laser treatment in the form of clinical clearance as improvement in visual analog score at 3 sessions, 6 sessions, 3 months follow-up and 6 months follow-up, and negative fungal cultures at 6 months follow-up. VAS: Visual analog score.
- Clinical appearance of nails with onychomycosis before the laser sessions (images a), at the end of 6 sessions (images b) and at 6 months follow-up (images c).
Two patients had shown a decrease in VAS during the sessions, but indicated a relapse after stopping the laser sessions. The patient on methotrexate had presented with highly hyperkeratotic nails. At the end of six sessions, he showed mild improvement in the form, a decrease in hyperkeratosis, and a decrease in the area of involvement in a few nails [Figure 6].

- A patient on methotrexate with highly hyperkeratotic nails in right foot (a) and left foot (c). At the end of six sessions, he showed mild improvement in right foot (b) and left foot (d) in the form of decrease in hyperkeratosis and decrease in the area of involvement in few nails.
Clinical efficacy
The OSI evaluated before the start of the laser sessions was compared with OSI measured six months after completion of the laser sessions [Figure 7]. A highly significant response (P < 0.001) to this treatment protocol was observed.
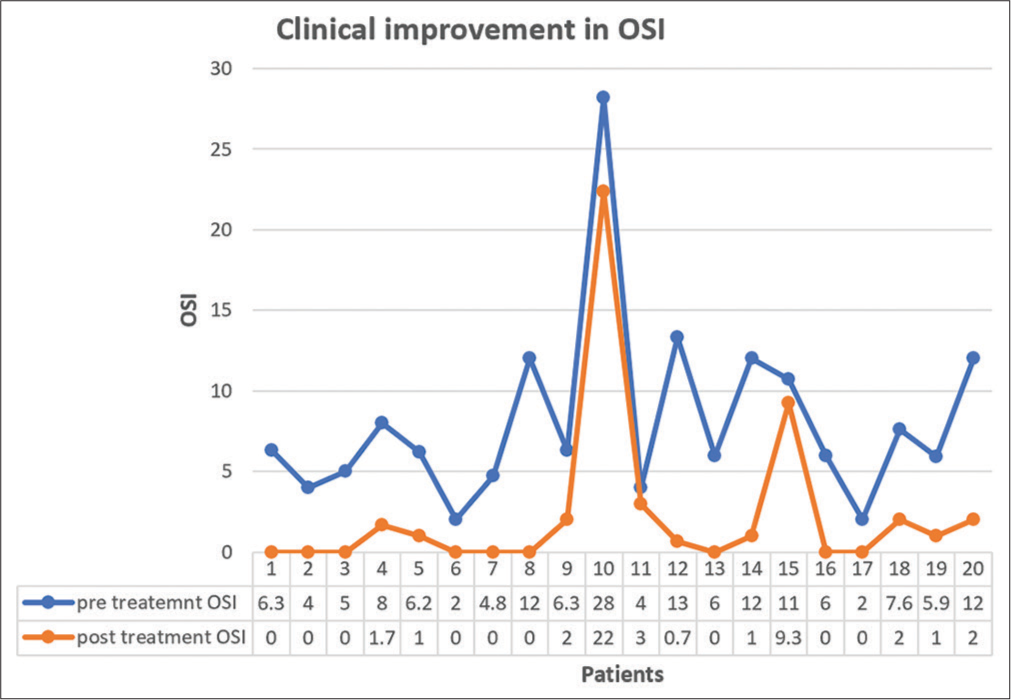
- Comparison of pre-treatment and post laser treatment (at 6 months follow-up) onychomycosis severity index score, depicting combined clinical efficacy of both the laser modalities.
Mycological clearance
At the six-month follow-up, fungal cultures were performed to measure mycological clearance [Table 5]. Seventeen (85%) patients, including two patients with resolving onycholytic pockets, showed negative cultures six months after completion of the sessions, proving there was no relapse till six months ([Figure 5], patient 2).
In addition, three patients (15%) showed positive cultures at the six-month follow-up. Two out of these three patients had a decrease in VAS during the sessions, indicating relapse after stopping the laser sessions. Both these patients were above the age of 50 years (51 and 81 years, respectively), with the former having uncontrolled diabetes at the time of treatment.
Adverse effects
Some patients experienced mild pain and discomfort during the laser sessions; however, these symptoms subsided soon after the laser. There was no bleeding or inflammation during or after the treatment, and none of the patients felt the need for an oral anti-inflammatory medication post the laser session.
DISCUSSION
Onychomycosis is the most common infective nail disorder, constituting 50% of all nail disorders.[2] T. rubrum and T. interdigitale are the most common causative dermatophytes, followed by molds, such as Fusarium, Aspergillus, and Acremonium. Yeasts, like Candida, are commonly found in individuals with predisposing factors, such as diabetes and immunosuppression.[4]
Onychomycosis is a difficult condition to treat due to the slow growth rate of the nail plate. The treatment is prolonged and can exceed more than a year. Oral antifungals are contraindicated in patients with active or chronic liver and kidney diseases. Some patients may refuse oral medications due to the prolonged duration and the possible side effects of such extended regimens. Relapses are also fairly common due to residual spores.[18] In addition, the fungal elements are believed to form a biofilm, making them refractory to therapy.[19] All these factors have made the formulation of alternative treatment methods essential.
Early reviews on the use of lasers in onychomycosis have given no consensus on the effectiveness of lasers.[16,20-22] Although the results have been mixed, these studies have definitely proven that lasers hold a future in the treatment of onychomycosis. A review article written by the authors of this study concluded that perforated CO2 laser had the best results followed by long-pulsed Nd: YAG laser.[13] We inferred that fractional CO2 laser in conjunction with a topical antifungal and with the use of quasi long-pulse (300 ms) mode of 1,064 nm Nd: YAG laser, shortened the treatment length and improved outcomes.[13] These are more readily available technologies in dermatology clinics, which prompted the authors to evaluate the efficacy of these lasers in their own practice.
It has been proven that complete fungal growth impairment can be achieved at temperatures above 50°C.[23] Nd: YAG lasers emit near-infrared light at a wavelength of 1,064 nm, which raises the tissue temperature to 60°C.[24] This temperature can cause fungal protein denaturation and collagen coagulation.
Long-pulsed Nd: YAG lasers have pulse duration in milliseconds. Due to the longer wavelength, the depth of penetration is deeper, but the degree of non-specific heating is high. Hence, a cooling system is required.[22] Moreover, the 1,064 nm lasers have melanin as their target chromophore. Melanoides variant of T. rubrum or other fungi (Neoscytalidium dimidiatum or Aspergillus niger) have melanin as an essential element of the fungal cell wall.[6]
Studies have shown successful treatment of onychomycosis with fractional CO2 lasers combined with topical antifungals.[25,26] Fractional CO2 laser works by vaporization of the target tissue. This has a photothermal effect on the fungi, causes exfoliation of the nail plate, forms fenestrations, and enhances the absorption and effect of topical antifungals.[27]
In this study, we evaluated the role of 1,064 nm Q-switched Nd: YAG laser and fractional CO2 laser in onychomycosis non-responsive to oral antifungals. The resistance to treatment can be attributed to the formation of a biofilm by the arthrospores, making the fungus refractive to the therapy. Laser therapy is not affected by biofilm formation.[19] Of the 20 patients included in the study, 60% were men. In addition, the number of involved nails of the feet was more (n = 57) than that of the hands (n = 20). This can be attributed to lesser hygiene of feet, which increases with age due to physical disability. Patients also tend to be less concerned with the cosmetic appearance of nails of feet unless multiple nails or massive hyperkeratosis is involved.
In this study, we combined two spot sizes (6 mm and 8 mm) at different energy levels of 1,064 Q-switched Nd: YAG laser using both nanosecond 1,064 nm and long-pulse quasi mode. This was done to give a combination of energies focused at different depths and destroy the fungal hyphae using thermal (photo-thermolytic) and mechanical (photo-chemical) action of the laser causing denaturation of the fungal cells.[19] A fractional CO2 laser was used to enhance the absorption of topical antifungal medication by the formation of a grid of fenestrations on the nail plate.[27]
In our study, 17 (85%) patients had negative fungal cultures at the last follow-up (six months after the laser sessions), indicating no relapse at six months. The clinical response was measured by comparing the OSI score before starting the laser treatment and the score at the last follow-up (six months after the sixth session). A significant difference in the two sets of values (P < 0.001) showed a good response to treatment. This clinical clearance was also maintained at six months.
VAS was used as a tool to measure the cosmetic response as observed by the patients. Progressive improvement of the VAS is an indicator of a positive response to the treatment. Fifteen (75%) out of the 20 patients showed complete clinical clearance at three months after completion of the six monthly sessions.
The results of our study show that the dose of energies administered by our treatment protocol produced temperatures high enough to serve as a deactivating dose for the fungus. It was observed that the study showed promising results with mild-to-moderate disease. The three patients, who did not respond to the treatment, had significant subungual hyperkeratosis, which takes more time to respond to any form of treatment. Lack of optimal response to treatment can also be attributed to old age and the presence of a concurrent underlying disease.
In contrast to the results of our study, in a study by Carney et al., no inhibition of the fungal colonies and no clinical improvement were observed after treatment with Nd: YAG laser.[28] Similarly, Hees et al. were unable to show satisfactory results both in a pilot study in 2012 and a study in 2014.[29] The results of our study are in compliance with the satisfactory results of other studies evaluating the effects of Q-switched Nd: YAG laser in onychomycosis.[30-33] Similar to this study, studies by Lim et al., Zhou et al., Arora et al., and Bhatta et al. evaluating the role of fractional CO2 laser also show positive results.[25-27,34] Our study is compared with other similar studies in Table 7.
| Authors | Laser used | Sessions | Follow-up periods | Study end point |
|---|---|---|---|---|
| Our study | Quasi microsecond and nanosecond Q switched 1064 nm Nd: YAG laser with fractional CO2 laser | 6 sessions, 1 month apart | At 3 months and at 6 months after completion of sessions | Clinical clearance in 15 (75%) patients at both follow-ups with mychological cure in 17 (85%) patients at 6 months |
| Carney et al.[28] | 1064 nm quasi long-pulse Nd: YAG laser | 4 sessions (at 1, 2, 3 and 7 weeks) |
At 6 months after last session | No significant decrease in area of nail involvement with OSI and negative cultures |
| Hees et al.[29] | 1064 nm Nd: YAG. Long-pulse (left toe nail) versus Short pulse (right toe nails) |
2 sessions, 4 weeks apart | 9 months | Decrease in area of nail involvement with OSI and negative histology and cultures in first 6 months and slight reversal at the end of 9 months. |
| Hochman[30] | 1064 nm short pulse Nd: YAG laser with topical anti-fungal | 2 or 3 sessions, 3 weeks apart | 6 months after final treatment | Significant visual improvement (not quantified) and negative fungal cultures. |
| Kimura et al.[31] | 1064 nm quasi long-pulse Nd: YAG laser | 2–3 sessions, 1–2 months apart | 6 months | Decrease in affected nail surface area (92%) and negative microscopy (50%) |
| Hollmig et al.[32] | 1064 nm quasi long-pulse Nd: YAG laser | 2 sessions, 2 weeks apart | 12 months | Negative cultures and clearance at 3 months (33% patients). No difference at 12 months in treated and control group. |
| Moon et al.[33] | 1064 nm quasi long-pulse Nd: YAG laser | 5 sessions, 1 month apart | 6 months | Decrease in affected nail surface area (15.38% complete clearance and 23% excellent>80% clearance) and negative microscopy (76.9%) |
| Lim et al.[25] | Fractional CO2 laser | 3 sessions, 1 month apart (with topical anti-fungal) |
6 months | Decrease in affected nail surface area (92%) and negative microscopy (50%) |
| Zhou et al.[27] | Fractional CO2 laser with 1% luliconazole AND Fractional CO2 laser alone | 1 session every 2 weeks for 6 months with or without daily topical application | 6 months | Mycological and clinical cure respectively; Laser: 39% and 53% Laser plus topical: 57% and 73% |
| Arora et al.[34] | Fractional CO2 laser | 4 sessions 1 month apart | 6 months after last session | 90% KOH and 88% culture negativity after 4 sessions, 86% KOH and 88% culture negativity after 6 months |
| Bhatta et al.[26] | Fractional CO2 laser with terbinafine cream | 3 sessions 4 weeks apart | 3 months and 6 months after the 3rd session | 94.66% and 92% KOH and culture negative at 3 months. 84% and 80% KOH and culture negative at 6 months. 98.18% and 78.18% clinical response in OSI at 3 and 6 months respectively. |
CO2: Carbon dioxide, Nd: YAG: Neodymium-doped yttrium aluminum garnet, OSI: Onychomycosis severity index, KOH: Potassium hydroxide
Limitations of the study
This study has a six months follow-up-up period after completion of the laser sessions. Due to the slow rate of growth of the toenails, we would further like to evaluate the results at the end of 12 months after the sixth session. As the effectiveness of lasers in onychomycosis is established without the use of oral antifungals, the authors would further like to compare the effectiveness of both the lasers with each other, as well as look into the response of these lasers to specific fungal species.
CONCLUSION
We can infer from our study that at the six months follow-up after the laser sessions, 75% of our patients had complete cosmetic clearance, with 85% of patients having negative fungal cultures indicating no relapse at 6 months, and a highly significant clinical response in OSI (P < 0.001) to this treatment protocol combining Q-switched Nd: YAG laser and fractional CO2 laser. Thus, we can definitely conclude that our study shows a promising use of lasers in the treatment of onychomycosis without the administration of oral anti-fungal drugs.
This study includes non-responder patients who opted out of further oral antifungal medication; hence, it was pertinent to formulate an effective alternate treatment option. These modalities are easily available in a dermatological setup; thus, they can either be combined with oral and topical antifungal treatments or used as stand-alone options.
Ethical approval
The study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that all subjects have given their informed consent for inclusion before they participated in the study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Antifungal drug use for onychomycosis. Am J Ther. 2019;26:e388-96.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013;32:S2-4.
- [CrossRef] [PubMed] [Google Scholar]
- Comorbidity of tinea pedis and onychomycosis and evaluation of risk factors in Latino immigrant poultry processing and other manual laborers. South Med J. 2014;107:374-49.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis: An updated review. Recent Pat Inflamm Allergy Drug Discov. 2020;14:32-45.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis: Clinical overview and diagnosis. J Am Acad Dermatol. 2019;80:835-51.
- [CrossRef] [PubMed] [Google Scholar]
- Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol. 2004;150:537-44.
- [CrossRef] [PubMed] [Google Scholar]
- The future of onychomycosis therapy may involve a combination of approaches. Br J Dermatol. 2001;145(Suppl 60):3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Preliminary report on use of carbon dioxide laser in podiatry. J Am Podiatry Assoc. 1984;74:509-13.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide laser use for certain diseases of the toenails. Clin Podiatr Med Surg. 1987;4:809-21.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive CO2 laser fenestration improves treatment of onychomycosis. Clin Laser Mon. 1992;10:123-4.
- [Google Scholar]
- The use of lasers in the treatment of onychomycosis (letter) Podiatry Now. 2009;12:57.
- [Google Scholar]
- Laser treatment for onychomycosis: A systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e17948.
- [CrossRef] [PubMed] [Google Scholar]
- The future of lasers in onychomycosis. J Dermatolog Treat. 2016;27:167-72.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of argon, dye, and Nd: YAG lasers on epidermis, dermis, and venous vessels. Lasers Surg Med. 1986;6:87-93.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis in clinical practice: Factors contributing to recurrence. Br J Dermatol. 2003;149(Suppl 65):5-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of Q-switched Nd: YAG 1064 nm/532 nm laser in the treatment of onychomycosis in vivo. Dermatol Res Pract. 2013;2013:379725.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of lasers in the treatment of onychomycosis: A systematic review. J Foot Ankle Res. 2014;7:34.
- [CrossRef] [PubMed] [Google Scholar]
- Laser and light therapy for onychomycosis: A systematic review. Lasers Med Sci. 2014;29:823-9.
- [CrossRef] [PubMed] [Google Scholar]
- Laser treatment for onychomycosis: A review. Mycoses. 2014;57:734-40.
- [CrossRef] [PubMed] [Google Scholar]
- Antifungal efficacy of lasers against dermatophytes and yeasts in vitro. Int J Hyperthermia. 2013;29:544-50.
- [CrossRef] [PubMed] [Google Scholar]
- Temperature rise in biological tissue during Nd: YAG laser irradiation. Lasers Surg Med. 1985;5:75-82.
- [CrossRef] [PubMed] [Google Scholar]
- Toenail onychomycosis treated with a fractional carbon-dioxide laser and topical antifungal cream. J Am Acad Dermatol. 2014;70:918-23.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon-dioxide (CO2) laser-assisted topical therapy for the treatment of onychomycosis. J Am Acad Dermatol. 2016;74:916-23.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of fractional carbon dioxide (CO2) laser combined with luliconazole 1% cream for the treatment of onychomycosis: A randomized, controlled trial. Medicine (Baltimore). 2016;95:e5141.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of onychomycosis using a submillisecond 1064-nm neodymium: yttrium-aluminum-garnet laser. J Am Acad Dermatol. 2013;69:578-82.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of onychomycosis using the 1064 nm Nd: YAG laser: A clinical pilot study. J Dtsch Dermatol Ges. 2014;12:322-9.
- [CrossRef] [PubMed] [Google Scholar]
- Laser treatment of onychomycosis using a novel 0.65-millisecond pulsed Nd: YAG 1064-nm laser. J Cosmet Laser Ther. 2011;13:2-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treating onychomycoses of the toenail: Clinical efficacy of the sub-millisecond 1,064 nm Nd: YAG laser using a 5 mm spot diameter. J Drugs Dermatol. 2012;11:496-504.
- [Google Scholar]
- Lack of efficacy with 1064-nm neodymium: yttrium-aluminum-garnet laser for the treatment of onychomycosis: A randomized, controlled trial. J Am Acad Dermatol. 2014;70:911-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of onychomycosis with a 1,064-nm long-pulsed Nd: YAG laser. J Cosmet Laser Ther. 2014;16:165-70.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional CO2 laser in the management of onychomycosis. J Mar Med Soc. 2020;22:50-3.
- [CrossRef] [Google Scholar]






