Translate this page into:
Pustular exacerbation of psoriasis precipitated by erythema multiforme like pityriasis rosea

*Corresponding author: Akash Agarwal, Assistant Professor, Department of Dermatology, IMS and SUM Hospital, Bhubaneswar, Odisha, India. akash.22.1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Madhual S, Sahoo S, Panda M, Agarwal A. Pustular exacerbation of psoriasis precipitated by erythema multiforme like pityriasis rosea. CosmoDerma. 2024;4:131. doi: 10.25259/CSDM_107_2024
Dear Sir,
A 47-year male, with a known case of chronic plaque psoriasis, presented to the dermatology outpatient department with reddish skin lesions over the trunk and lower limbs since a week. Initially, the patient developed multiple asymptomatic red elevated skin lesions over the trunk, upper limbs and back for 10 days followed by multiple painful pus-filled lesions adjacent to pre-existing psoriatic plaques for 2–3 days. Cutaneous examination revealed multiple annular erythematous to dusky papules and plaques over the trunk with the center showing necrosis and peripheral rim of edema (targetoid morphology) suggestive of erythema multiforme-like pityriasis rosea (EM-like-PR). There were multiple well-defined erythematous indurated plaques with central loosely adherent silvery white scales over the elbow, lower abdomen, and bilateral lower limbs clinically suggestive of plaque psoriasis. Grattage test was done at the bedside which showed accentuation of exfoliation of loosely adherent scales over the lower abdomen. Auspitz sign was also found to be positive over plaques over the lower abdomen. After a meticulous/thorough clinical examination, it was found that most of the PR lesions appeared over an apparently normal-looking skin over the trunk, which was distant to the previously present psoriatic plaque in the lower abdomen, elbow, and bilateral lower limb. Over the bilateral lower limbs, the psoriatic plaques were tender with surrounding erythema extending beyond the plaques. Over the erythematous base, multiple pus-filled lesions were observed with a few of them merging to give a “lake of pus appearance” [Figure 1a-d].
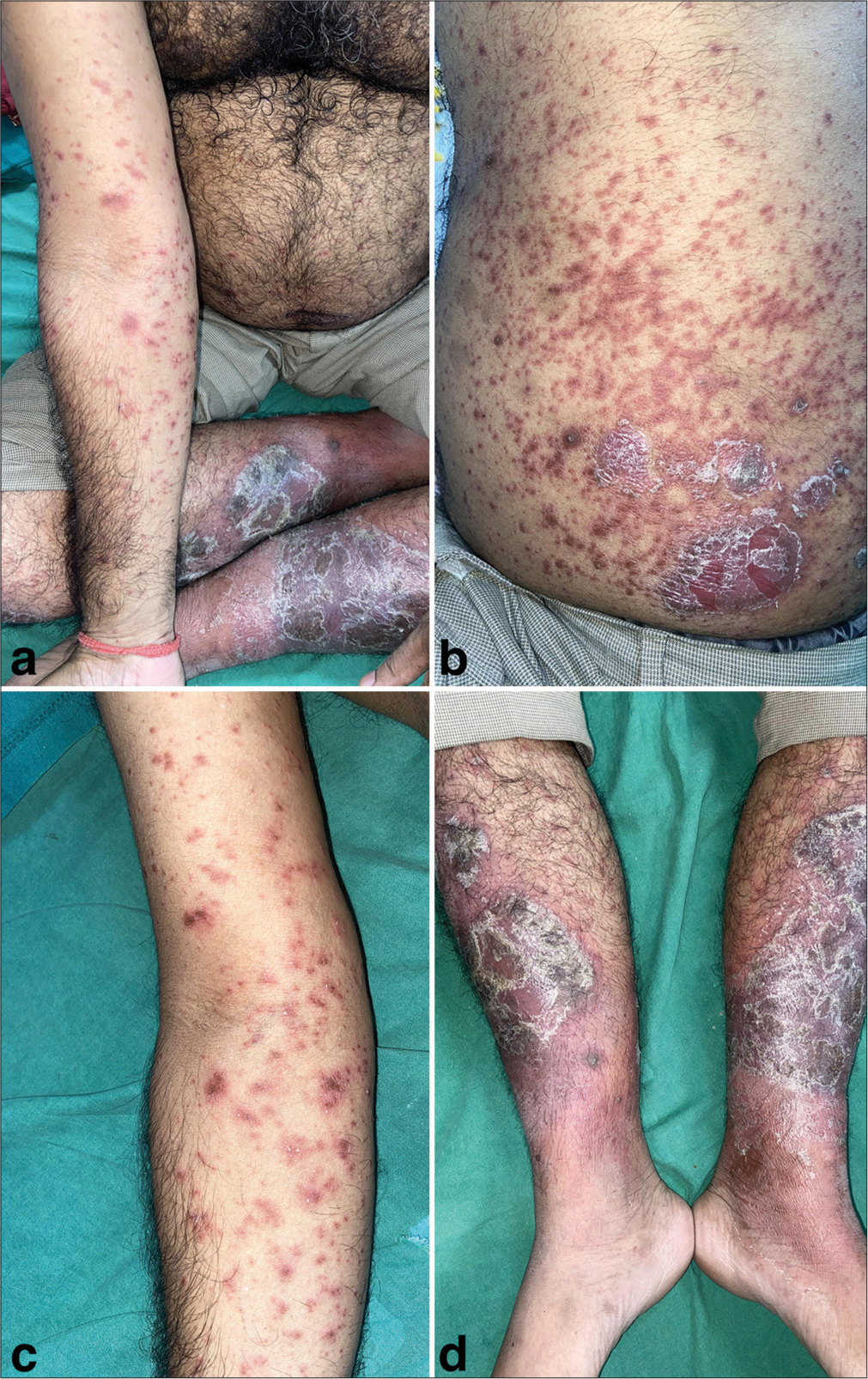
- (a) Multiple well-defined erythematous indurated plaques approximately of size ranging from 4 × 5 cm to 6 × 7 cm with central loosely adherent silvery white scale over the elbow, lower abdomen, and bilateral lower limbs clinically diagnostic of plaque psoriasis. (b and c) Multiple annular erythematous to dusky papules and plaques of varying sizes with the center showing necrosis and peripheral rim of edema (targetoid morphology) suggestive of erythema multiforme such as pityriasis rosea over trunk, forearm, and back. (d) Over the bilateral lower limbs, the psoriatic plaques with surrounding erythema extending beyond the plaques. Over the erythematous base, multiple pus-filled lesions were observed with few of them merging to form a “lake of pus appearance.”
Biopsy taken from the psoriatic lesion showed histological features consistent with psoriasis [Figure 2a], while a sample from the annular papule over the trunk showed spongiosis, lymphocytic infiltration around dilated blood vessels in the upper dermis, and extravasated red blood cells (RBCs) suggestive of PR [Figure 2b and c]. No drug association was present and all routine investigations were within normal limits. Venereal disease research laboratory test was negative. Based on history, clinic-histopathological correlation, and ruling out other precipitating factors, a final diagnosis of EM-like-PR causing pustular exacerbation of psoriasis was made. The patient was admitted and managed conservatively with oral acitretin and topical emollients. The patient’s condition improved in the next seven days and is currently on regular follow-up.
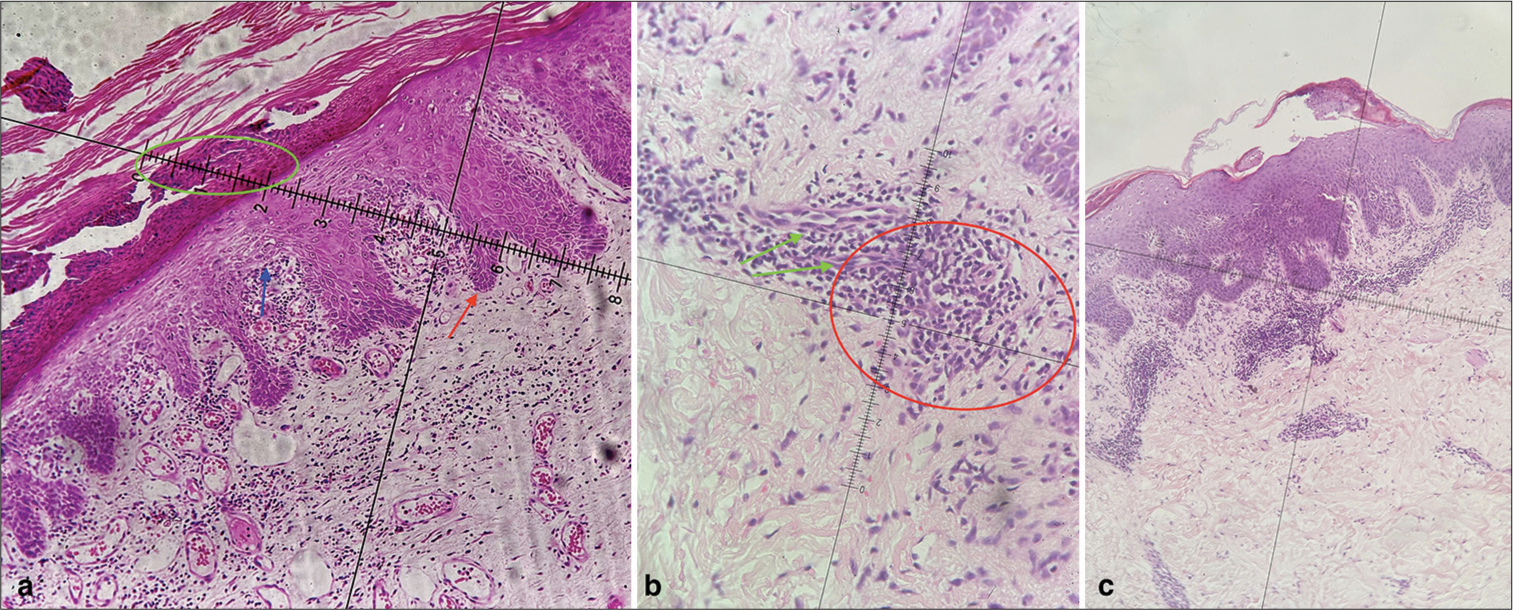
- (a) Photomicrograph shows features of hyperkeratosis, acanthosis, parakeratosis, Munro’s microabscess (green circle), and suprapapillary thinning (blue arrow) and regular elongation of rete ridges (red arrow) suggestive of psoriasis (×40, H&E stain), (b) photomicrograph lymphocytic infiltration in the upper the dermis around dilated blood vessels (green arrow), and extravasated red blood cells (red circle) suggestive of pityriasis rosea (×40, H&E stain), and (c) Photomicrograph shows hyperkeratosis, irregular acanthosis, spongiosis, and parakeratoses with inflammatory infiltrate in dermis (×10, H&E stain). H&E: Hematoxylin and eosin.
The PR, a benign self-limiting papulosquamous disorder, may present with atypical morphologies such as vesicular, purpuric, inverse, lichenoid, EM like lesions, in up to 20% of cases that might pose a diagnostic challenge.[1-3] Various hypotheses incriminate infection (mostly viruses such as human herpesvirus-6 and human herpesvirus-7 infection), drugs, or vaccines as a cause. Although most cases are idiopathic, features such as presence of prodrome, seasonal exacerbation, and clustering in communities indicate infective etiology.[2]
Psoriasis is a chronic immune-mediated inflammatory disease with multiple phenotypes such as plaque, flexural, guttate, pustular, or erythrodermic. Although the correlation between guttate psoriasis and streptococcal pharyngitis is well established, viral and fungal infections have also been implicated to induce psoriasis.[3] Pustular psoriasis is an unstable form of psoriasis that may occur de novo or in patients of chronic plaque psoriasis due to triggers such as withdrawal of steroids, infections, stress, electrolyte imbalance, few drugs, or vaccines.[3,4] In this report, we present a case of a pustular flare of psoriasis probably precipitated due to EM-like-PR. The patient was in remission for the past six months after receiving secukinumab, and the patient was not also on any intermittent medications such as systemic steroids, methotrexate, or cyclosporine. History of any recent stress, vaccination, surgery, or other infections was also excluded from the study.
Reports of temporal association of PR leading to pustular aggravation of psoriasis are lacking. Sacchidanand et al. reported a single case of PR precipitating psoriasis wherein coexisting features of both PR and psoriasis had been found on histopathological analysis.[5] To the best of our knowledge, this case may represent the first case of EM-like PR precipitating pustular psoriasis.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pityriasis rosea: An update on etiopathogenesis and management of difficult aspects. Indian J Dermatol. 2016;61:375-84.
- [CrossRef] [Google Scholar]
- A case series of erythema multiforme-like pityriasis rosea. Indian Dermatol Online J. 2016;7:212-5.
- [CrossRef] [Google Scholar]
- Clinical course and characteristics of generalized pustular psoriasis. Am J Clin Dermatol. 2022;23(Suppl 1):21-9.
- [CrossRef] [Google Scholar]
- Polymorphic pityriasis rosea precipitating psoriasis. Indian Dermatol Online J. 2013;4:63-4.
- [CrossRef] [Google Scholar]





