Translate this page into:
Pityriasis rosea gigantea

*Corresponding author: Biswanath Behera, Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta P, Shetty M, Behera B. Pityriasis rosea gigantea. CosmoDerma 2023;3:160.
A middle-aged female presented to us with 2-month duration of asymptomatic reddish raised scaly lesions over the trunk and proximal extremities. On examination, multiple, well-defined erythematous annular to polycyclic plaques of size varying from 1 × 1 cm to up to 10 × 8 cm were present over the above-mentioned sites with minimum fine scales and central hypopigmentation [Figures 1 and 2]. Biopsy from the lesions was done with clinical possibility of pityriasis rosea gigantea and was confirmed on histopathology which revealed acanthotic epidermis with lymphocytic exocytosis, spongiosis, hypogranulosis, and focal intraepidermal erythrocytes. In dermis, mild perivascular lymphocytic infiltrate and extravasated erythrocytes were seen [Figure 3]. A diagnosis of pityriasis rosea gigantea (atypical) was made and lesions resolved at 3-month follow-up. Other differentials which can be considered include pityriasis alba and small plaque/large plaque parapsoriasis. Pityriasis alba is characterized by ill-defined hypopigmented patches with minimal erythema and scaling. On the contrary, lesions in our patient were having eruptive scaly erythematous margins and hypopigmented hue in the center. Similarly, small plaque parapsoriasis has dermatomal pattern of digitate lesions with size <5 cm not seen in our case. Large plaque parapsoriasis will have gradual onset, larger, asymmetric, non-scaly plaques. In addition, the absence of poikiloderma and more than 50% improvement within 1 month of topical steroid application were points favoring the diagnosis of pityriasis rosea over parapsoriasis. On histopathology, in addition to lymphocytic infiltrate, parapsoriasis will show interface dermatitis and often atrophied epidermis which were absent in our case. However, histopathology is non-specific and diagnosis is clinical. The absence of follicular plugs and atrophied sebaceous glands on histopathology ruled out pityriasis alba. Differential diagnosis of leprosy can be considered as the differential; however, it was ruled out clinically by the absence of history of erythematous skin lesions, no sensory or autonomic loss on the lesions, and no thickened nerve on palpation. Histopathologically, no granulomatous reaction and no bacilli seen on wade-fite staining ruled out leprosy.

- Clinical image shows annular plaques with erythematous scaly margin and central hypopigmentation. Note the gigantic plaque measuring 10 × 8 cm.

- Multiple large annular erythematous plaques with central hypopigmentation and scaling at the periphery.
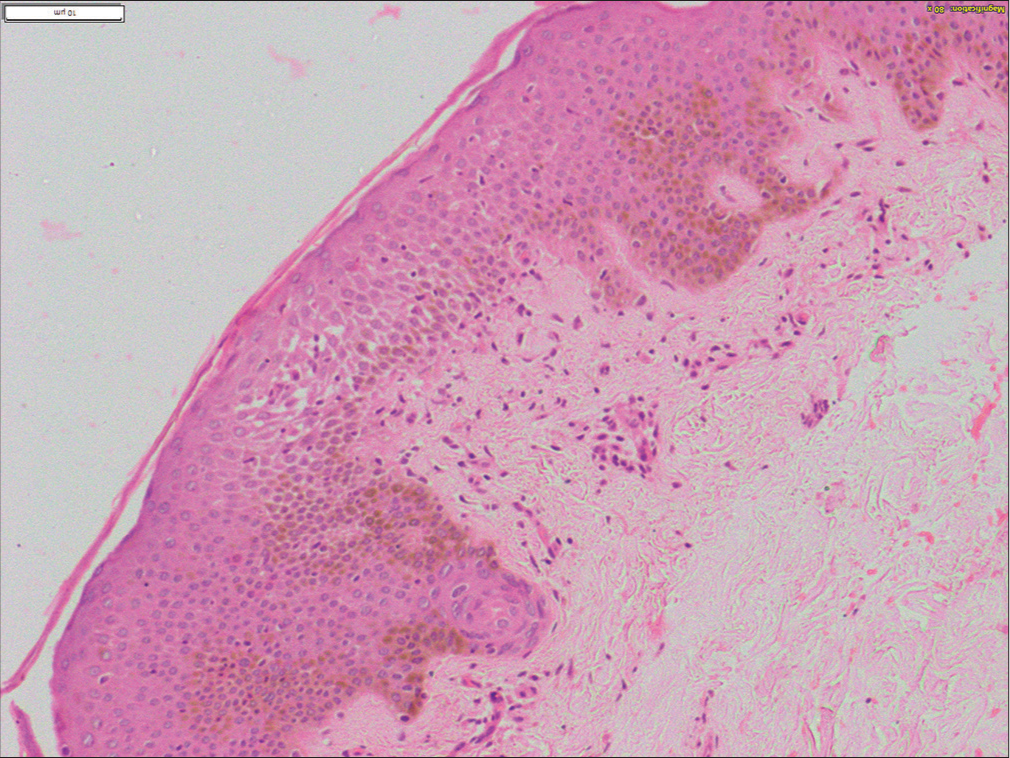
- Histopathological image shows acanthotic epidermis with lymphocytic exocytosis, spongiosis, hypogranulosis, and focal intraepidermal erythrocytes. Dermis shows mild perivascular lymphocytic infiltrate and extravasated erythrocytes (H and E, ×400).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.





