Translate this page into:
Primary cutaneous actinomycosis manifesting as pyomyositis: A diagnostic challenge

*Corresponding author: Anil Kumar Panda, Department of Dermatology, Venereology, Leprosy, Institute of Medical Sciences and SUM Hospital, Bhubaneswar, Odisha, India. dranil18@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pramanik A, Mishra S, Panda AK, Panda M. Primary cutaneous actinomycosis manifesting as pyomyositis: A diagnostic challenge. CosmoDerma. 2024;4:72. doi: 10.25259/CSDM_49_2024
Dear Sir,
Actinomycosis is an infectious disease caused by Gram-positive, non-acid fast, filamentous group of bacteria Actinomyces. It progresses slowly and usually involves cervicofacial, abdominopelvic, and pulmothoracic regions of the body. Involvement of the leg as a primary site of infection is uncommon. Moreover, the development of an intramuscular abscess secondary to cutaneous actinomycosis is a rare finding and poses both a diagnostic and therapeutic challenge. We are presenting a case letter of primary cutaneous actinomycosis with pyomyositis which required surgical intervention along with conventional medical treatment.
A 57-year-old female patient presented with skin-colored fluctuant swelling over the posterolateral aspect of the right leg having occasional seropurulent discharge with pain and difficulty in walking for the past three months. On examination, there was a solitary nodule having a sinus with seropurulent, odorless discharge. Adjacent to it, an atrophic scar was present that represented the previously healed lesion [Figure 1]. On palpation, there was minimal tenderness over the swelling and also over the right calf muscle. She was complaining of mild intermittent fever, not associated with an evening rise in temperature, cough, or weight loss. There was no prior history of trauma, animal bite, barefoot walking, or any surgical intervention. On general examination, the patient had stable vitals, mild pallor, and no lymphadenopathy.

- Solitary erythematous nodule having discharging sinus with adjacent scar present over posterolateral aspect of right leg.
Routine baseline blood investigations were normal. Chest x-ray was unremarkable. Cartridge-based nucleic acid amplification test was negative. There were no granules in the pus. On Gram stain examination, the pus showed Gram-positive bacilli but no organism was found on culture. No acid–fast bacilli were found. A potassium hydroxide mount was prepared but nothing significant was detected. On histopathology, basophilic bacterial colonies were seen in the upper dermis surrounded by inflammatory cell infiltrates containing predominantly neutrophils and macrophages [Figure 2]. No epithelioid cell granuloma was noticed. X-ray of the leg showed no bone involvement. Ultrasonography showed ill-defined heteroechoic collection in the intramuscular plane in the posteromedial aspect of the right leg, which is focally communicating with the skin surface through a sinus tract. The patient was sent to the surgery department for incision and drainage. The collected pus revealed Gram-positive and culture-negative bacilli on microbiological examination similar to the previous report, which was done from cutaneous discharging sinus. So finally, a diagnosis of primary cutaneous actinomycosis with pyomyositis was made and the patient was started with an antibiotic coverage of cotrimoxazole (double-strength tablet) and amoxicillin 2 g daily. After 6 weeks, the lesion improved significantly both morphologically and symptomatically. The sinuses healed with fibrosis and there was no induration, discharge, or appearance of any new lesions [Figure 3]. The patient is still continuing the above antibiotics, which are planned for further two months.
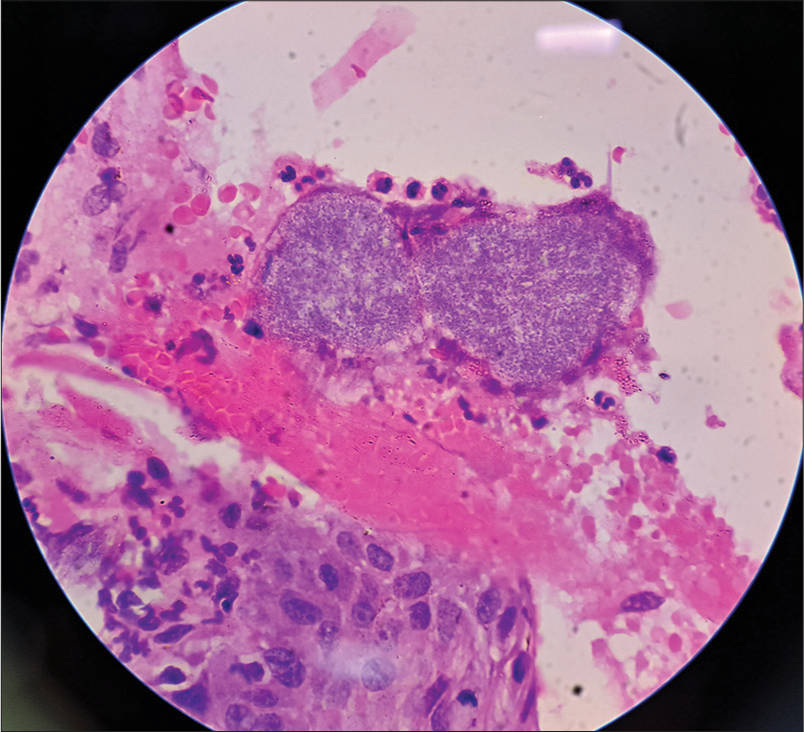
- Histopathology showing basophilic actinomycotic colonies surrounded by inflammatory cell infiltrates present in upper dermis (Hematoxylin and eosin, ×40).

- Healed nodule and sinus after 6 weeks of therapy.
Actinomycosis is usually underdiagnosed in the field of dermatology and is considered as a diagnostic challenge. It is most commonly caused by the Gram-positive bacterium Actinomyces israelii.[1] It is characterized by a contiguous spread with multiple abscesses and discharging sinuses having sulfur granules. It affects mostly males in the middle decade of life.[2] Predominantly, it is endogenous in origin with involvement of cervicofacial, thoracic, abdominal, and pelvic regions. Being a non-virulent organism, it requires a breakage in the integrity of the mucous membranes to cause disease. Recognition of definitive history and factors that enable bacterial entry into deep tissues is likely to be difficult. However, it should not rule out the disease when the clinical scenario is appropriate. Primary cutaneous actinomycosis is a rare condition and the soft tissue involvement due to the chronic disease is also an underreported subject. Primary disease of the extremities is uncommon.[3] Most of the cases reported give a clear history of trauma, either a human bite or a perforating injury with contamination from the outside. Occasionally, the hematogenous spread can occur.[4] The infection may begin either as an abscess-like swelling that can penetrate to overlying skin mimicking malignancy or as nodules that later develop into fistulae, clinically simulating cutaneous tuberculosis, sporotrichosis, and nocardiosis.[5] In our patient, there was no history of trauma and so the exact pathogenesis remains unclear. A similar case reported from Delhi had no history of trauma.[6] In addition, there were no granules in our case which is typically seen in actinomycosis. The diagnosis was finally confirmed by histopathological examination of the lesions and corroboratory radiological and microbiological findings.
The treatment of primary cutaneous actinomycosis can involve a combination of surgery and antibiotics which is poorly standardized. Surgery should be indicated in conditions where there is involvement of deeper structures like muscle or lack of response to usual conventional antibiotics.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Agents of actinomycosis In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice in infectious diseases. Vol 2. Philadelphia, PA: Elsevier; 2009. p. :2864-73.
- [CrossRef] [Google Scholar]
- Actinomycosis In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. Harrison's principles of internal medicine (20th ed). United States: McGraw Hill; 2018.
- [Google Scholar]
- A suspected case of primary cutaneous actinomycosis on the buttock. J Dermatol. 2001;28:276-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary actinomycosis of an extremity: A case report and review. Rev Infect Dis. 1987;9:581-9.
- [CrossRef] [PubMed] [Google Scholar]
- Primary actinomycosis of the thigh-a rare soft tissue infection with review of literature. JRSM Short Rep. 2012;3:24.
- [CrossRef] [PubMed] [Google Scholar]





