Translate this page into:
Photoprotection in children - Is it really required?

*Corresponding author: Uwe Wollina, Department of Dermatology and Allergology, Städtisches Klinikum Dresden, Dresden, Germany. uwollina@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wollina U. Photoprotection in children - Is it really required? CosmoDerma. 2025;5:57. doi: 10.25259/CSDM_71_2025
Human skin is exposed to sunlight, which consists of ultraviolet (UV) and near-infrared irradiation. UVB and UVC are absorbed directly by deoxyribonucleic acid (DNA), causing the formation of thymine dimers, mainly cyclobutane pyrimidine dimers and pyrimidine (6–4) pyrimidone photoproducts.
UVA exposure also causes thymine dimers. In addition, it leads to the generation of reactive oxygen species (ROS) through photosensitizing reactions, and thus, indirectly causes oxidative DNA damage. There is an absolute safe range of UV exposure. Darker skin has a higher eumelanin content and therefore absorbs more UV light than light skin.
While UV irradiation has positive effects on general health, well-being, and Vitamin D metabolism, excessive exposure can cause harm. Sunburn, preliminary skin aging, and possible induction of skin cancers are well-known risks.
About 80% of lifetime exposure to UV irradiation occurs before puberty. This should be a strong argument for an early start of photoprotection in childhood.
While the interest in tanning is high in Western countries, the interest in photoprotection in infants and children seems to be remarkably low worldwide [Figures 1 and 2].
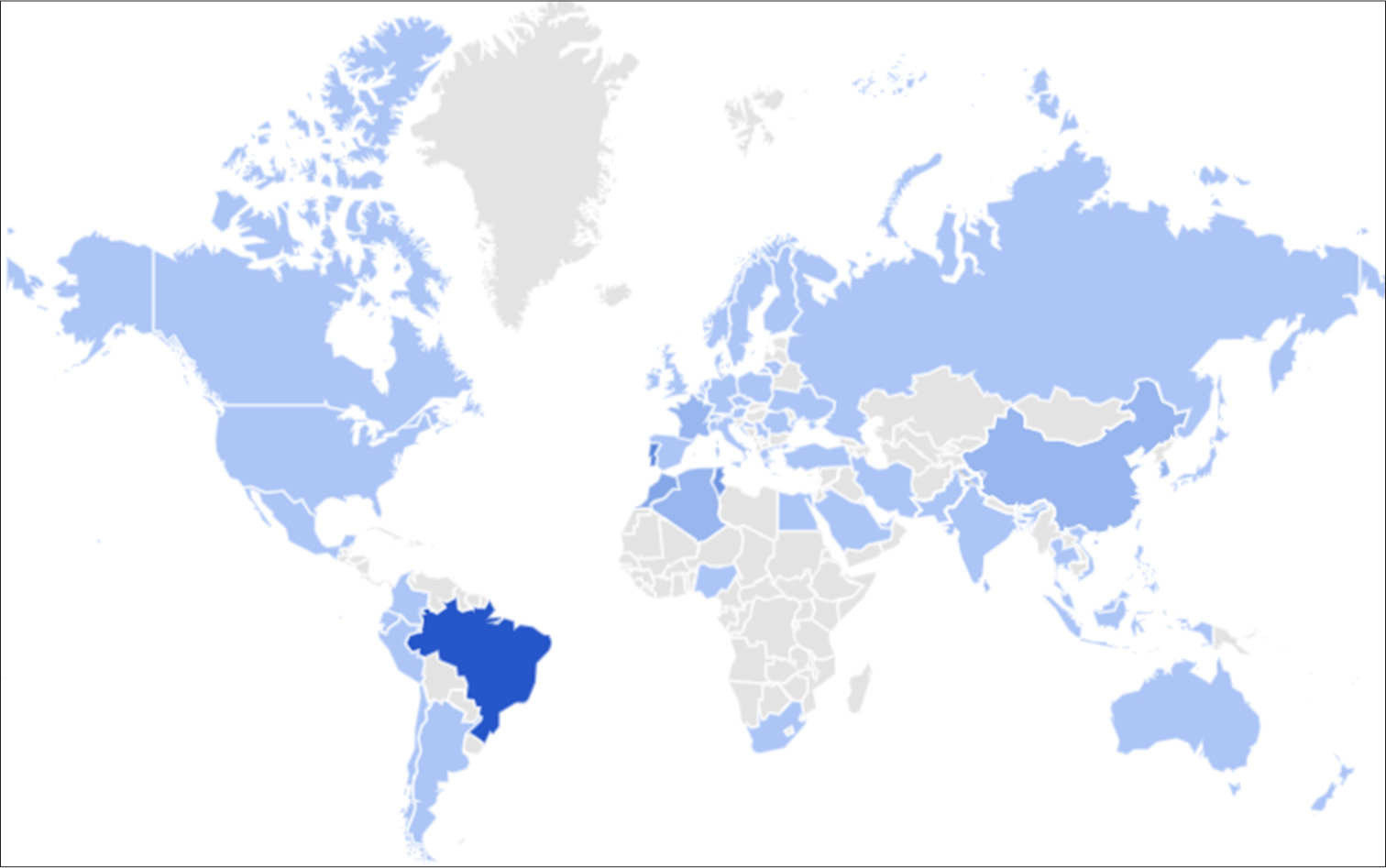
- Interest in tanning marked as light blue and dark blue areas (Google Trends 2004–2025).

- Interest in photoprotection during childhood marked as light and dark brick red areas (Google Trends 2004–2025).
This situation is incomprehensible since the protection of children is a great asset. Primary prevention of long-term risks of UV exposure should be started as early as possible. In infants, avoidance of direct sun exposure and the use of protective clothes are essential. In infants younger than 6 months, sunscreens are not recommended due to possible systemic absorption of ingredients.
In infants and children of older age, sunscreens with physical filters can be recommended. Iron oxides and pigmentary-grade titanium dioxide are the only filters for visible light. In melanated patients, white sunscreen is less convenient to use but tinted sunscreen is less available and often more expensive. As experience shows, concentrating solely on sunscreens is insufficient and conveys a false sense of security. Appropriate sun behavior and protective clothing are crucial. Parents and other caregivers take on a model role in dealing with the sun. Preschool can also help with this. Children’s playgrounds should offer shaded areas.
Nutritional factors should not be ignored. There is no sunscreen available that protects sufficiently against ROS, but natural products in our nutrition plan can help. Efficient ROS scavengers including vitamins C and E, lycopene, carotenoids, and flavonoids contained in vegetables and fruits are examples of a holistic approach to sun protection. On the other hand, fast food that supports glycation depletes endogenous antioxidant systems. Last but not least, the potential harmful effects of excessive sunscreen use on vulnerable ecosystems cannot be ignored.
International scientific activities such as the SunSmart policy in Australia of C.O.C.C.O. guidelines of the Photoprotection Group of the Italian Federation of Pediatricians focus on the special needs of infants and children.
Health and intellect are the two goods of life – as Meandros (342–291 B.C.) the Greek poet – mentioned. Promoting them should begin at an early age.





