Translate this page into:
Papulonecrotic tuberculid with an atypical presentation

*Corresponding author: Rachita S. Dhurat, Prof and Head, Department of Dermatology, Lokmanya Tilak Municipal Medical College and Government Hospital, Mumbai, Maharashtra, India. rachitadhurat@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Kowe P, Surushe SA, Kale GG, Dhurat RS. Papulonecrotic tuberculid with an atypical presentation. CosmoDerma. 2024;4:85. doi: 10.25259/CSDM_83_2024
Abstract
The tuberculids constitute the immune-mediated non-infectious cutaneous hypersensitivity reaction pattern to the underlying focus of Mycobacterium tuberculosis antigen in patients with good cell-mediated immunity. Papulonecrotic tuberculid (PNT) is a true tuberculid that usually occurs secondary to the underlying focus of infection which may be in the lymph nodes, lungs, bone, or rarely in other systems. It manifests as asymptomatic symmetric eruptions of erythematous papules with central areas of ulceration and crusting that heals with varioliform scars. PNT presenting as a generalized folliculitis-like lesion and rosettes has not been described earlier. Furthermore, PNT occurring as a hypersensitivity response due to underlying mediastinal tuberculous lymphadenitis (MTL) is rare. We are highlighting a case of PNT secondary to the MTL in a middle-aged woman.
Keywords
Papulonecrotic tuberculid
Yellow-orange area
Wedge-shaped necrosis
Mediastinal tuberculous lymphadenitis
INTRODUCTION
Tuberculosis (TB) is still considered a serious public health illness as a consequence of drug-resistant Mycobacterium species which requires extended duration of treatment that accounts for high cost and economic burden in a developing country like India. Cutaneous TB generally responds well to the currently available anti-tubercular regimen. At times, the diagnosis of tuberculid may become difficult due to the atypical morphology of skin lesions in an otherwise asymptomatic patient without any proven underlying cause. A thorough investigation for detailed lymph node examination in an asymptomatic individual can pick the diagnosis of lymph node TB which, then, can be promptly treated. A case of papulonecrotic tuberculid (PNT) with an unusual morphology is enlighted here.
CASE REPORT
A 47-year-old woman presented with a complaint of asymptomatic lesions over the face, trunk, and extremities for three months. There was a history of occasional low-grade fever and back pain for the past six months. There was no personal or family history of TB and sexual history was insignificant. Cutaneous examination showed multiple asymptomatic erythematous papules, some were flat-topped tiny papules surrounding the central large papule (rosette-like), and pustules (folliculitis-like), of which some were ulcerated in the center distributed symmetrically over face, chest, abdomen, back, and extremities [Figures 1a-d, 2a and b]. Dermoscopy under polarized mode (Dermlite, DL4, ×10 magnification) showed follicular yellow-white area, perifollicular yellow-orange structureless area, and peripheral white scaling [Figure 3a and b]. We kept the differential diagnosis of secondary syphilis, pityriasis lichenoides et varioliformis acuta (PLEVA), and PNT. General and systemic examination was normal. There was no lymphadenopathy. Erythrocyte sedimentation rate was raised (48 mm in the first hour), serology for human immunodeficiency virus (HIV) infection and venereal disease research laboratory test was non-reactive, and bronchoalveolar lavage for acid-fast bacilli (AFB) was negative. Histopathology from an erythematous papule showed a wedge-shaped area of necrosis extending from the epidermis to the mid dermis with a collection of inflammatory cells mainly neutrophils. Below this necrotic area infiltrate such as neutrophils, lymphocytes, histiocytes, and epithelioid cells were seen forming granulomatous patterns located mainly around the hair follicles, and blood vessels, there was dilatation of blood vessels with perivascular neutrophilic and lymphocytic infiltrate [Figure 4a-c]. The Ziehl-Neelsen stain for AFB and tissue culture for mycobacteria were negative. Her Mantoux test (MT) was strongly positive after 48 h of reading (20 mm × 20 mm) [Figure 5a]. Thus, based on clinical findings, skin biopsy, and positive MT test, a diagnosis of PNT was considered. Chest radiography was normal. High-resolution contrast tomography thorax revealed multiple homogenous enlarged lymph nodes in the pre/paratracheal, prevascular, aortopulmonary, and subcarinal region, multiple fibrocalcific plaques with fibrotic changes in the adjacent lung parenchyma were also noted in the apical segment of both upper lobes suggestive of mediastinal TB [Figure 5b]. Thus, a final diagnosis of PNT secondary to mediastinal tuberculous lymphadenitis (MTL) was made. The patient was started on category I of antitubercular therapy (ATT) as advised by the pulmonary medicine department. There was a visible improvement in skin lesions after 4 weeks of ATT and significant improvement after 4 months of ATT [Figure 6a-e].
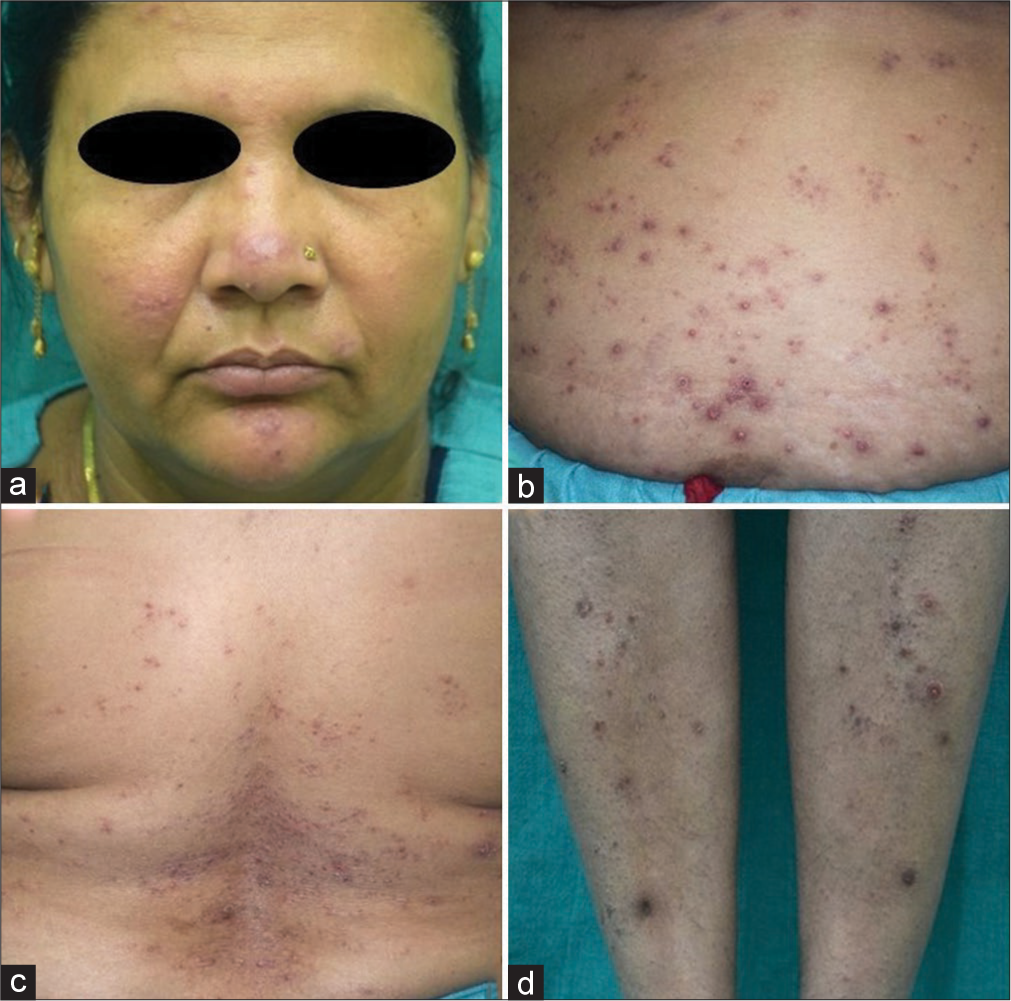
- (a-d) Erythematous crusted and ulcerated papules over face, abdomen, back, and legs.
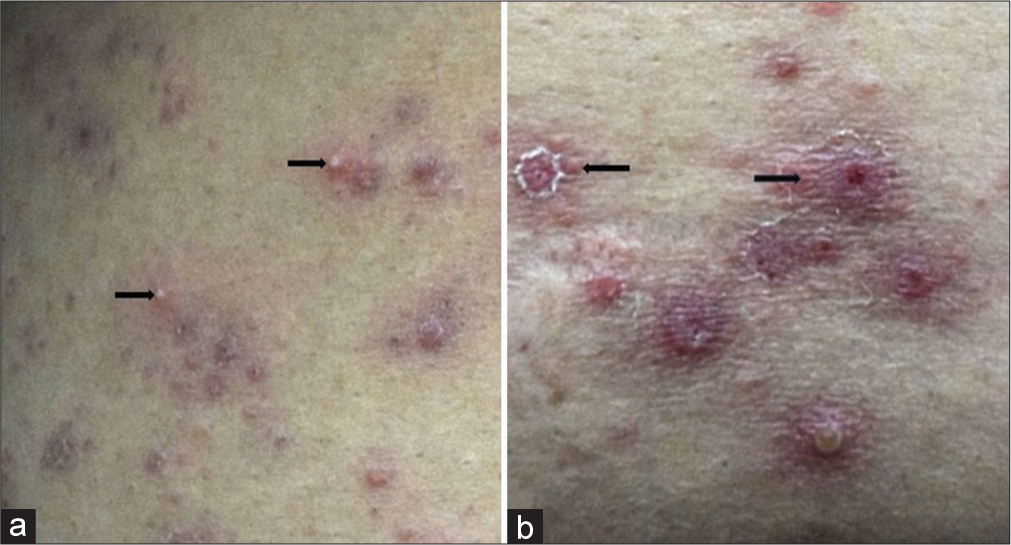
- (a) Follicular pustule, and (b) erythematous crusted papule with rosette formation.
![(a) Dermoscopy showing follicular yellow-white area (black circle), perifollicular yellow-orange structureless area (black star) and peripheral white scaling (black arrow) and (b) crust with peripheral pigmentation (black arrow) [DermLite DL4, polarized, ×10 magnification].](/content/130/2024/4/1/img/CSDM-4-85-g003.png)
- (a) Dermoscopy showing follicular yellow-white area (black circle), perifollicular yellow-orange structureless area (black star) and peripheral white scaling (black arrow) and (b) crust with peripheral pigmentation (black arrow) [DermLite DL4, polarized, ×10 magnification].
![(a) Scanner view showing wedge-shaped necrosis of epidermis extending till mid dermis with periappendageal granulomatous collection (blue arrow) [H and E, ×40], (b) dilatation of blood vessels with perivascular neutrophilic and lymphocytic infiltrate (black arrow) [H and E, ×100], and (c) collection of inflammatory cells such as lymphocytes, histiocyte, and epithelioid cells forming granulomas in the deep dermis (blue arrow) [H and E ×400].](/content/130/2024/4/1/img/CSDM-4-85-g004.png)
- (a) Scanner view showing wedge-shaped necrosis of epidermis extending till mid dermis with periappendageal granulomatous collection (blue arrow) [H and E, ×40], (b) dilatation of blood vessels with perivascular neutrophilic and lymphocytic infiltrate (black arrow) [H and E, ×100], and (c) collection of inflammatory cells such as lymphocytes, histiocyte, and epithelioid cells forming granulomas in the deep dermis (blue arrow) [H and E ×400].
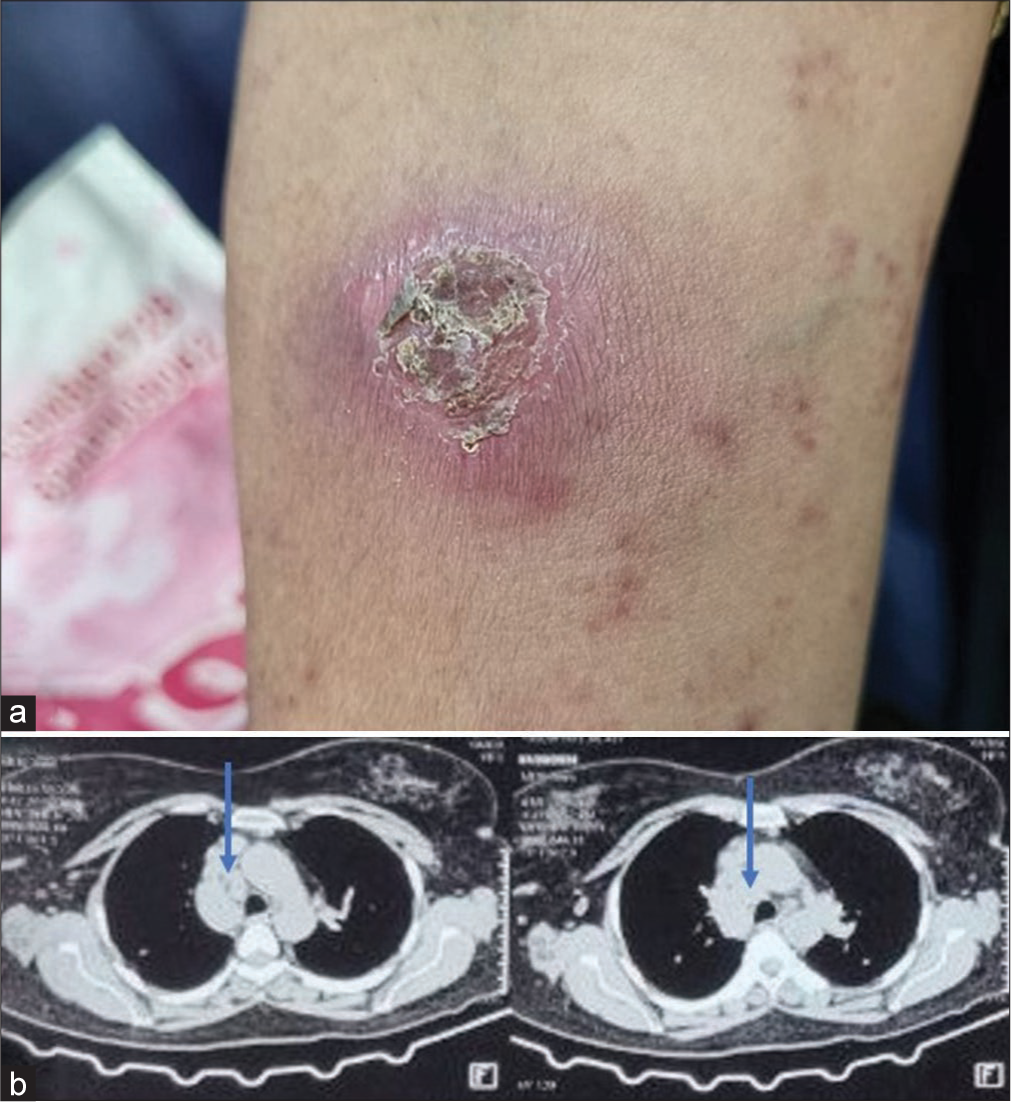
- (a) Strongly positive Mountox test and (b) high-resolution computed tomography thorax showing enlarged mediastinal lymph nodes (blue arrow).
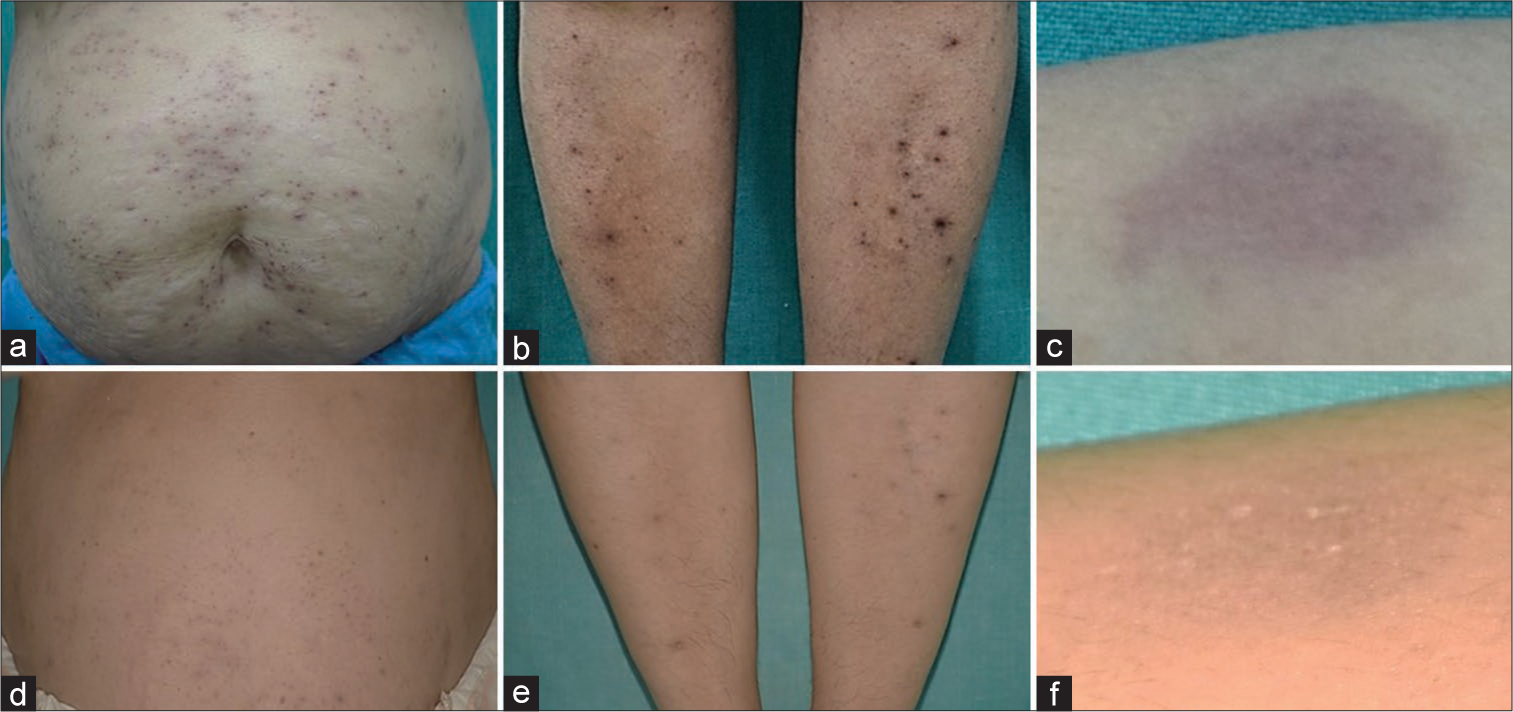
- (a-c) Post-treatment after 4 weeks and (d-f) post-treatment after 4 months.
DISCUSSION
Among cutaneous TB, the prevalence rate of tuberculid ranges from 4 to 44.2% in different studies worldwide and the incidence of PNT is approximately 4%.[1,2] It primarily impacts children and adolescents with a slightly higher incidence in females.[2] The PNT along with lichen scrofulosorum represents true tuberculid as Mycobacterium tuberculosis is the major etiological agent reported. Other rare causes of PNT include Mycobacterium kansasii, Mycobacterium avium-intracellulare complex, bacillus Calmette-Guerin vaccination, MT, and HIV infection.[2] The typical morphology of PNT includes crops of dusky-red papules with central ulceration healing with atrophic depressed scar involving extensors of extremities, ears, acral region, genitalia, perineum, etc. There are reports of atypical presentation of PNT, including molluscum-like, perforating granuloma annulare-like, pityriasis lichenoides chronica-like, and PNT with systemic features [Table 1].[1,3,4] Our patient presented with papulopustular morphology mimicking folliculitis and some of the lesions over the abdomen resembled rosettes (central erythematous crusted papules encircled by tiny erythematous papules). Thus, we observed two different morphologies (rosettes-like and folliculitis-like) that were not reported earlier. Dermoscopy of PNT includes yellow-orange structureless areas.[2,5] In addition to this, radiating white streaks were also reported.[6] Our patient showed a follicular yellow-white area in the center that corresponded to neutrophilic collection on histopathology, surrounded by a yellow-orange perifollicular structureless area correlated with the granulomatous collection on histopathology, which was surrounded by peripheral white collaret of scale. Among extrapulmonary TB cases, lymph node TB is the most prevalent form with the cervical lymph nodes being the most commonly affected group.[7] The PNT is most commonly associated with tuberculous lymphadenitis followed by pulmonary, bone, genitourinary nasopharyngeal, and renal TB.[1] Involvement of mediastinal lymph nodes by mycobacteria is rare and MTL as a cause of PNT is even more rare.[8] The MTL commonly presents in children and adolescents; however, the index case presented in her fifth decade was an uncommon finding. The closest clinical differential diagnosis of PNT is PLEVA from which it is differentiated based on the symmetrical crops of papulo-ulcerated lesions with central crusting healing with varioliform scars, highly positive MT, evidence of underlying TB, and prompt response to ATT. The PLEVA presents as red-brown papulovesicular lesions with a mica-like scale which are adherent in the center and lifted peripherally over the trunk and proximal extremities that heal with hypo or hyperpigmentation.[9] The PNT is known to respond well to a standard four-drug ATT regimen for six months with the response being noted as early as four to six weeks. Our patient responded to ATT in a month with near-complete resolution in four months.
| Uncommon morphology | Description |
|---|---|
| Molluscum-like lesions.[1] | Pink-umbilicated molluscum-like papules |
| Perforating granuloma-annulare-like lesions.[1] | Erythematous umbilicated papules with central crusting with discrete perilesional desquamation |
| Pityriasis lichenoides chronica-like lesions.[1] | Erythematous papules with peripheral scaling seen in association with cervical tuberculous lymphadenitis |
| PNT associated with ophthalmological complications.[1] | Uveitis, optic neuritis as a part of immune-mediated reaction |
| PNT associated with Poncet disease.[1] | Poncet disease is an immune-mediated, inflammatory oligoarthritis which represents a rare paucibacillary manifestation of TB |
| Localized form of PNT manifesting as penile TB.[1] | Papulonodular lesions with ulceration presenting over glans penis |
| PNT with other cutaneous TB.[1] | There are reports of co-occurrence of PNT with other forms of cutaneous TB such as lupus vulgaris, scrofuloderma, tubercular gumma, erythema induratum, and other tuberculids |
| It has also been reported at the site of tuberculin skin test | |
| Hodgkin’s lymphoma presenting with PNT.[3] | Papulonodular skin lesions on an erythematous base as a paraneoplastic manifestation of Hodgkin’s lymphoma |
| PNT of the vulva.[4] | Multiple crops of erythematous papules with crusting involving vulva in a patient of lymphatic and pulmonary TB |
| Present case. | Folliculitis-like and Rosette-like morphology |
TB: Tuberculosis, PNT: Papulonecrotic tuberculid
CONCLUSION
The PNT is an uncommon manifestation of tuberculid, and when it occurs, a thorough evaluation for the involvement of internal organs is necessary. Our case is unique in terms of age, atypical morphology of skin lesions, and prompt response to ATT.
Ethical Approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tuberculids: A narrative review. Indian Dermatol Online J. 2023;14:320-9.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of Hodgkin's lymphoma presenting with papulonecrotic tuberculid. BMJ Case Rep. 2017;2017:bcr2017220484.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual case of vulval papulonecrotic tuberculid. Clin Exp Dermatol. 2011;36:277-80.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of the diverse spectrum of cutaneous tuberculosis in the skin of color. Dermatol Pract Concept. 2022;12:e2022203.
- [CrossRef] [PubMed] [Google Scholar]
- A cross sectional descriptive study of dermoscopic features of clinical variants of cutaneous tuberculosis. Indian J Tuberc. 2023;70:501-7.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculous lymphadenopathy: Experience from the referral center of Northern India. Niger Med J. 2016;57:134-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mediastinal tuberculous lymphadenitis presenting with insidious back pain in a male adult: A case report and review of the literature. J Int Med Res. 2021;49
- [CrossRef] [PubMed] [Google Scholar]
- Pityriasis lichenoides et varioliformis acuta (PLEVA) In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
- [Google Scholar]






