Translate this page into:
Nodular basal cell carcinoma in a young female at an unusual site – A rare presentation

*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government T.D. Medical College, Alappuzha, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nair PS, Treasily A. Nodular basal cell carcinoma in a young female at an unusual site – A rare presentation. CosmoDerma. 2024;4:45. doi: 10.25259/CSDM_26_2024
Dear Sir,
A 22-year-old Information Technology employee presented with an asymptomatic hyperpigmented nodule on the anterior abdominal wall of three months’ duration. The lesion first started as an erythematous papule on the abdominal wall, which evolved to attain the present size within a span of three months. The lesion was asymptomatic, and there was no history of bleeding, oozing, crusting or ulceration. The patient denied a history of sun tanning or any previous congenital nevus at the site of the nodule. On examination, there was a well-defined hyperpigmented firm nodule of 2 × 3 cm with the surface showing scaling on the anterior abdominal wall at the midline between the epigastrium and the umbilicus [Figure 1]. There was no regional lymphadenopathy, and the systems were within normal limits. Dermoscopy showed brown-black areas with central scaling and a few dilated blood vessels. We had differentials of dermatofibroma, melanoma, and appendageal skin tumor.

- Well-defined hyperpigmented nodule with scaling on anterior abdominal wall.
The blood hemogram was normal, and viral markers were negative. Ultrasound abdomen and computerized tomography scan of the abdomen were normal and did not show any abdominal lymphadenopathy. An excision biopsy was done by the surgeon. Skin biopsy showed epidermal atrophy and the dermis packed with islands of basaloid tumor cells with melanin deposits in some islands [Figure 2]. High power showed the basaloid tumor cells to have peripheral palisading of the nuclei along with melanin deposits and intervening stromal reaction pattern [Figure 3]. Immunohistochemistry demonstrated the tumor cells to be positive for Bcl-2 [Figure 4]. All these were diagnostic of basal cell carcinoma (BCC). We made a final diagnosis of nodular BCC – pigmented type. The biopsy specimen showed complete tumor excision with normal tumor-free margins. There was no recurrence even after one-year follow-up.
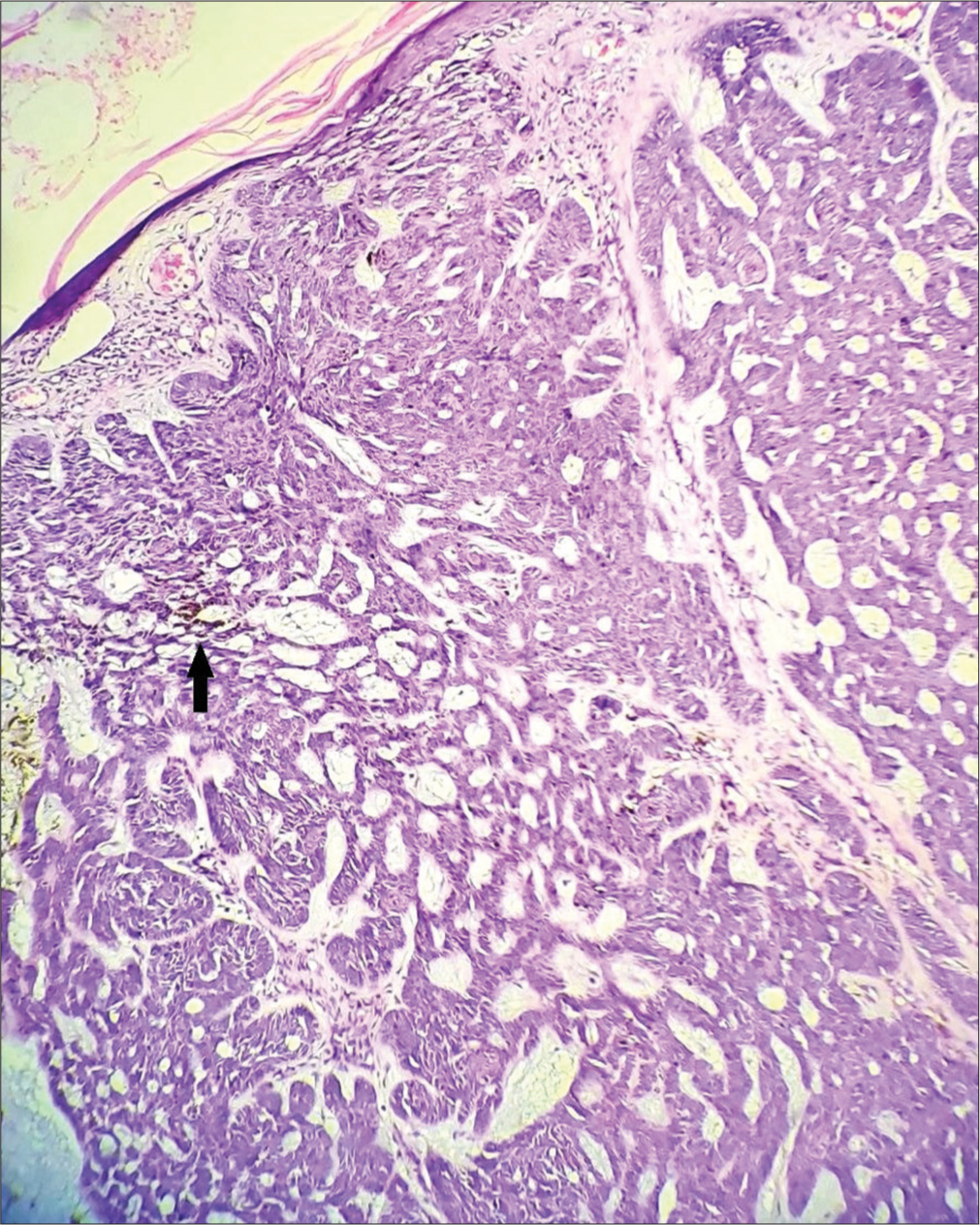
- Islands of basaloid tumor cells in the dermis with melanin deposits (arrow), H & E × 100.
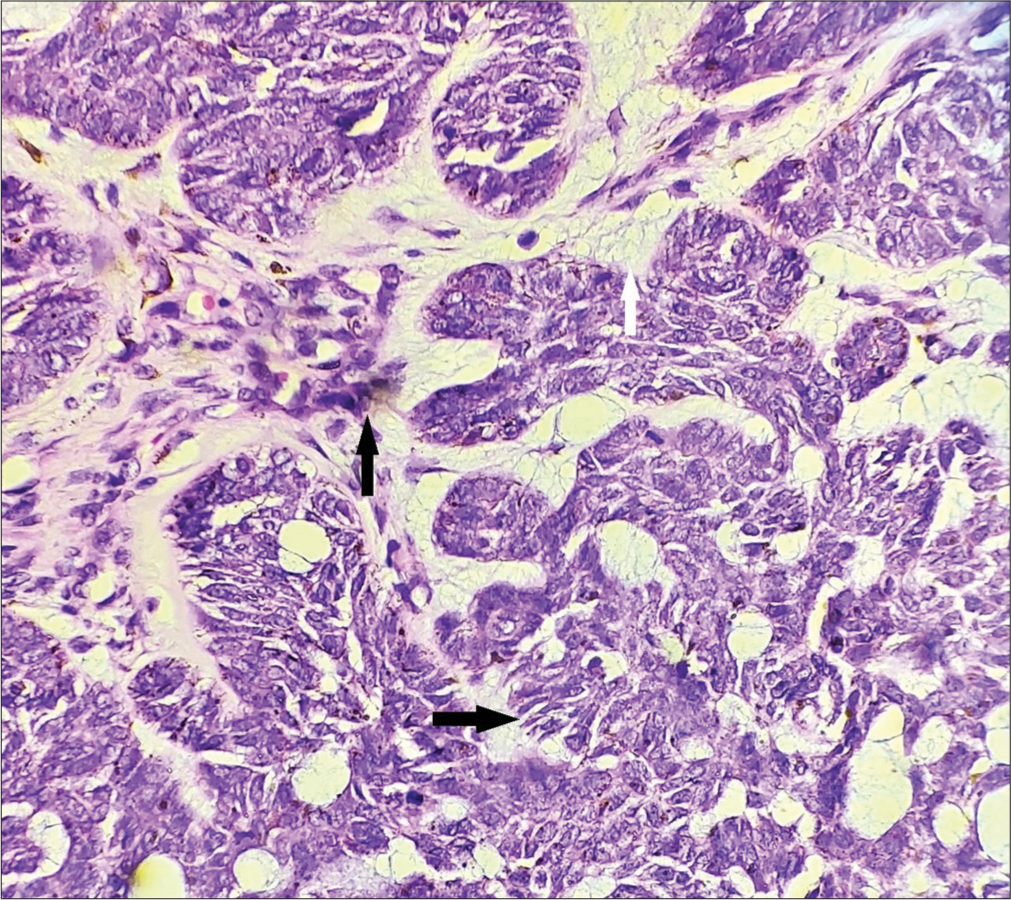
- Basaloid tumor islands showing peripheral palisading of nuclei (horizontal black arrow), melanin deposits (vertical black arrow), and intervening stroma (vertical white arrow), H&E × 400.
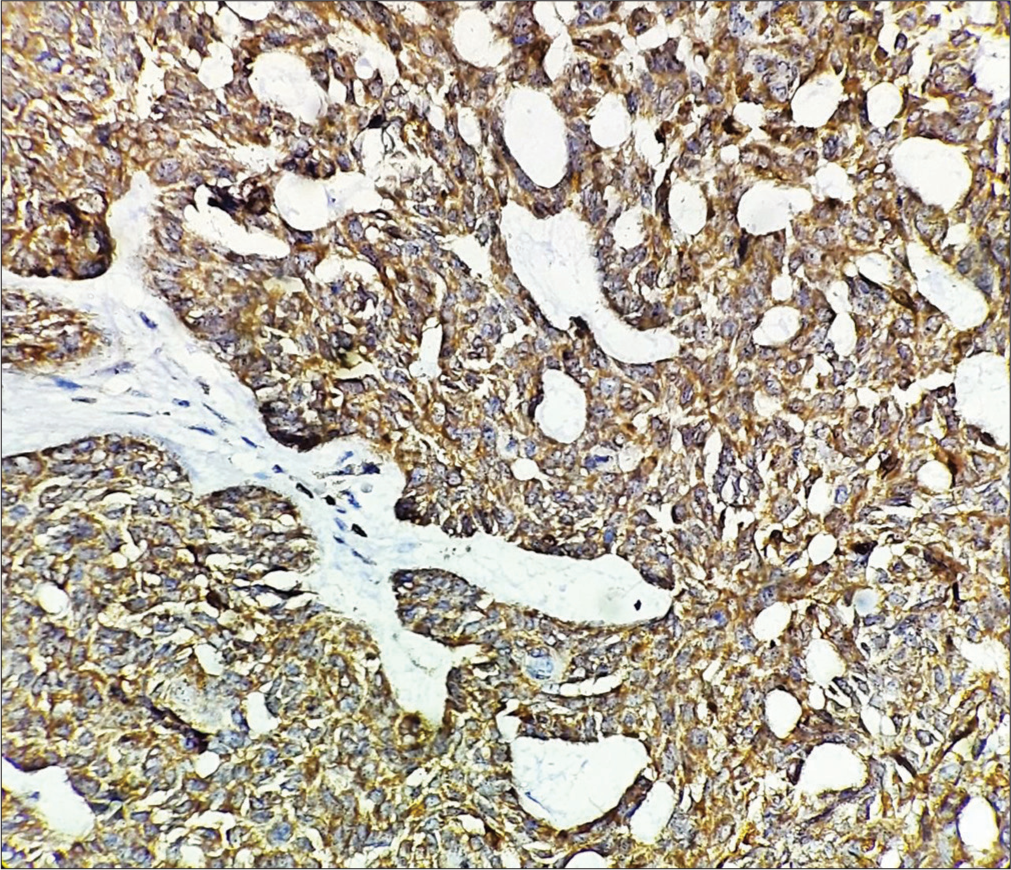
- Immunohistochemistry showing tumor cells to be positive for Bcl-2, Immunohistochemistry stain × 400.
The BCC is the most common malignant skin tumor worldwide. The presentation is usually in middle to old age, and the majority give a history of frequent sunlight exposure indicating ultraviolet radiation as an important risk factor.[1] The most common presentation is the “Rodent ulcer,” of which the nodular BCC is one variant. The ulcerated type has a characteristic raised rolled edge. Our patient was very young (22 years), did not give a history of frequent sun exposure, and the tumor was in a sun-protected area, the anterior abdominal wall. This is the highlight of this case report. The most common site of BCC is the face, and presentation in sun-protected areas is very rare. However, multiple BCCs in photo and photo-protected areas are seen in the context of nevoid BCC syndrome (Gorlin’s syndrome), chronic arsenic poisoning, and xeroderma pigmentosum. It is not very clear of the factors responsible for the presentation of BCC in sun-protected area in our case. The other rare presentations are the morpheaform BCC, fibroepithelioma of pinkus, micronodular BCC, and basosquamous carcinoma, in which both basaloid and squamous tumor cells are seen.[2] The BCC is a localized malignant skin tumor, but very rarely metastasis can occur to the lymph nodes, lungs, and bones. The other rare presentation is local destruction of underlying tissue including bones, denoted as “ulcus terebrans.” The classical dermoscopic findings are gray-brown structureless areas, blue-gray ovoid nests, maple leaf-like areas, spoke wheel-like patterns, concentric structures, and arborizing vessels.[2] However, these features may not be seen in all the cases, as in our case. The histopathology is classic with basaloid islands of tumor cells with peripheral palisading of nuclei, stromal reaction pattern, and peritumor lacunae.
When melanin deposits are seen in the tumor islands, as in our case, the term pigmented BCC is used. The cytomarkers used for diagnosis of BCC are Ber EP4, Bcl-2 (positive in our case), and CD10. The most important histological differential diagnosis is trichoepithelioma. However, in trichoepithelioma in addition to basaloid tumor cells, papillary mesenchymal bodies are seen, and the peritumor lacunae seen in BCC are absent, and the tumor is CD10 negative. Surgical excision is the treatment of choice for nodular BCC. If the excised skin biopsy specimen shows tumor cells in the free margins, external radiation may be given.[3] Small BCCs can be treated medically with 5% imiquimod, 5-fluorouracil, and photodynamic therapy.[4] Moh’s micrographic surgery, cryotherapy, and carbon dioxide ablative lasers are the other destructive modalities.[3,4] Recent reports indicate that advanced BCC, destructive BCC, and metastatic BCC can be treated with Hedgehog inhibitors such as vismodegib and sonidegib.[5] These drugs are also useful in preventing BCC occurring in nevoid BCC syndrome. Rare presentations of BCC may be misdiagnosed.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Trends in basal cell carcinoma incidence and identification of high-risk subgroups, 1998-2012. JAMA Dermatol. 2015;151:976-81.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-17.
- [CrossRef] [PubMed] [Google Scholar]
- Treatments of primary basal cell carcinoma of the skin: A systematic review and network meta-analysis. Ann Intern Med. 2018;169:456-66.
- [CrossRef] [PubMed] [Google Scholar]
- Photodynamic therapy versus topical imiquimod versus topical fluorouracil for treatment of superficial basal-cell carcinoma: A single blind, non-inferiority, randomised controlled trial. Lancet Oncol. 2013;14:647-54.
- [CrossRef] [PubMed] [Google Scholar]
- Inhibiting the hedgehog pathway in patients with basal-cell nevus syndrome: Final results from the 36-month trial. Lancet Oncol. 2016;17:1720-31.
- [CrossRef] [PubMed] [Google Scholar]





