Translate this page into:
Maturational hyperpigmentation: An update

*Corresponding author: Payal Chauhan, Department of Dermatology, All India Institute of Medical Sciences, Jammu, Jammu and Kashmir, India. chauhanpayal89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Goyal P, Chauhan P. Maturational hyperpigmentation: An update. CosmoDerma. 2024;4:23. doi: 10.25259/CSDM_269_2023
Abstract
Maturational hyperpigmentation is a form of acquired idiopathic facial melanosis, which is a relatively recently described entity, mainly seen in middle-aged individuals. Apart from its disturbing nature due to significant psychosocial impact and cosmetic concern, it is also believed to be associated with a metabolic syndrome similar to facial acanthosis nigricans. While both these disorders are close differentials of each other and could represent the same spectrum, there are significant differences between both. It is therefore important to raise awareness among dermatologists so as not to miss this relatively new, under-recognized, and frequently misdiagnosed entity.
Keywords
Clinical dermatology
Facial melanoses
Maturational hyperpigmentation
Metabolic syndrome
Facial melanoses include a spectrum of hyperpigmentary disorders with overlapping features, predominantly melasma, exogenous ochronosis, lichen planus pigmentosus, Riehl’s melanosis, facial acanthosis nigricans, pigmentary demarcation lines, frictional melanosis, and post-inflammatory hyperpigmentation. These facial dermatoses have a substantial psychosocial impact and are linked to cosmetic deformity.
Maturational hyperpigmentation is a form of acquired idiopathic facial melanosis, which is a relatively recently described entity seen in middle-aged patients with darker Fitzpatrick skin phototypes V and VI. Clinically, it presents as asymptomatic granular hyperpigmentation with indistinct margins blending into the surrounding normal skin. It tends to predominantly involve the sun-exposed areas of the lateral face. The temples and hollows of the cheeks are mainly affected with occasional extension onto the melolabial folds [Figure 1a].[1] Various characteristics noted in maturational hyperpigmentation include the adult onset of the disease, obesity, ambiguous relationship to sun exposure, and pigmentation preferentially involving the usual sleeping side of the face.[2] Maturational hyperpigmentation is believed to be associated with metabolic syndrome, similar to facial acanthosis nigricans.[2] Therefore, the possibility of both these disorders representing the same spectrum cannot be completely ruled out. By the extension of the same theory of association with metabolic syndrome presenting predominantly in middle-aged adults, which is further compounded by cumulative sun exposure, the occurrence of maturational hyperpigmentation in middle age can be effectively explained.
Facial acanthosis nigricans is the closest differential of maturational hyperpigmentation.[2] Both entities are believed to signify cutaneous manifestations of metabolic syndrome during the disease.[3] However, there are significant clinico-dermoscopic and histopathological differences between the two entities. Maturational hyperpigmentation has a distinct fine granular surface as compared to the velvety rough surface of facial acanthosis nigricans. The former shows the presence of accentuated pseudoreticular pigment network, brown globules, and brown rings concentrated around the follicular openings without any sulci or cristae on dermoscopic examination [Figure 1b]. Histopathology of maturational hyperpigmentation is characterized by minimal hyperkeratosis and mild-to-moderate basal layer melanocytic proliferation with slight papillomatosis sans dermal inflammation.[2,3] However, acanthosis nigricans on dermoscopy shows characteristic linear crista cutis and sulcus cutis with dark brown or black dots with perifollicular hyperpigmentation whereas the histopathological examination reveals the presence of basketweave hyperkeratosis, acanthosis, dermal papillomatosis with elongated and pigmented rete ridges.[4]
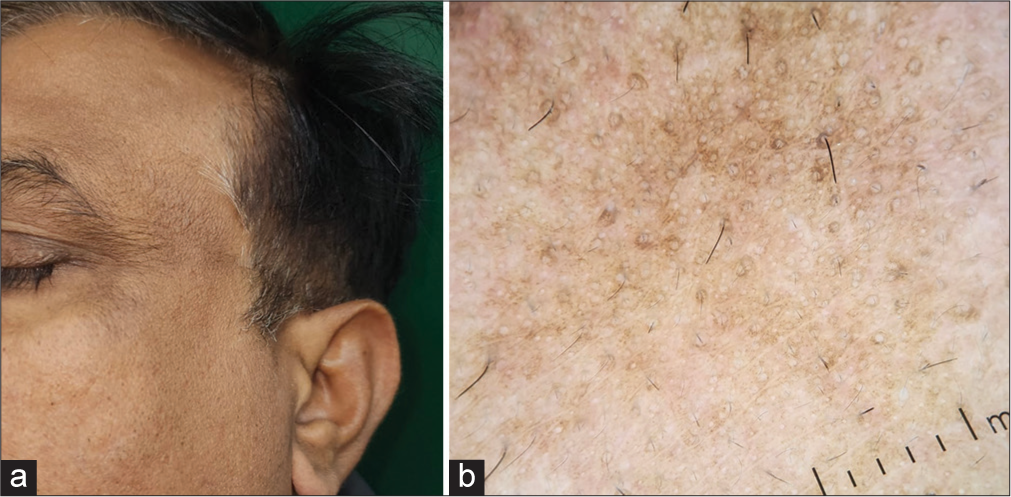
- (a) Presence of ill-defined, granular hyperpigmentation with indistinct margins involving the left forehead and lateral face in a case of maturational hyperpigmentation; (b) Dermoscopic examination revealed brown round to oval pigmentation around follicular opening with pseudoreticular pigment network (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification): Picture courtesy: Dr. Dilip Meena, Associate Professor, Dermatology, TMU Moradabad.
The various facial melanoses and their differentiating features are listed in Table 1 and Figures 2-5.
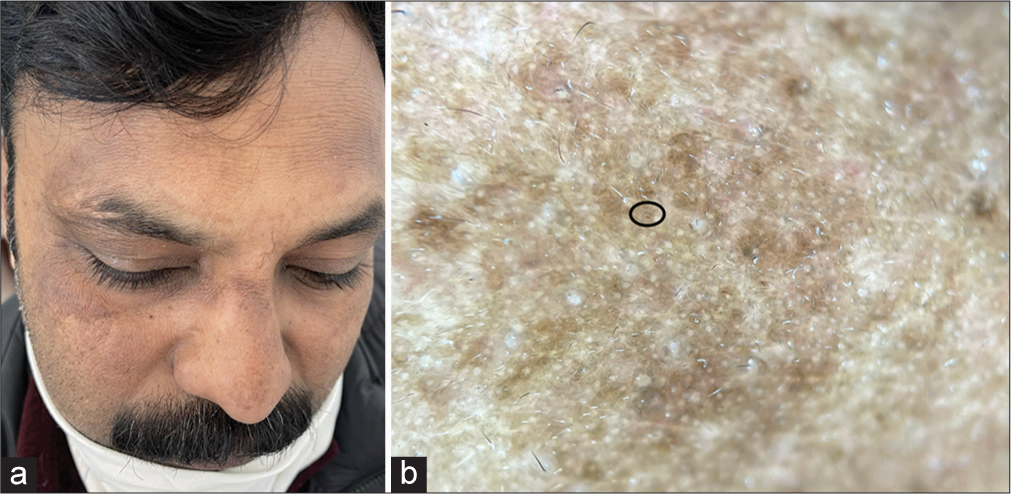
- (a) Presence of ill-defined, irregular, brownish patches of pigmentation symmetrically distributed over bilateral sides of forehead, lateral cheeks, nasal bridge and eyebrows in a case of melasma; (b) Dermoscopic examination revealed the presence of reticuloglobular pigment, with few brown dots (black oval), and unfocussed telangiectasia (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification).

- (a) Presence of dark gray patches of pigmentation with confetti-like areas of normal skin and underlying erythema distributed over the cheeks, nose, upper lip, and chin in a middle-aged female patient of exogenous ochronosis; (b) Dermoscopic examination revealed the presence of oval to oblong pattern of blue-gray globules with patchy areas of erythema and telangiectasia (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification).

- (a) Presence of velvety patches of skin with accentuation of skin surface over the right side of face, predominantly involving the forehead and cheek in a case of facial acanthosis nigricans; (b) Dermoscopic examination revealed linear crista cutis and sulcus cutis, with black dots in the cristae, and follicular plugging (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification).
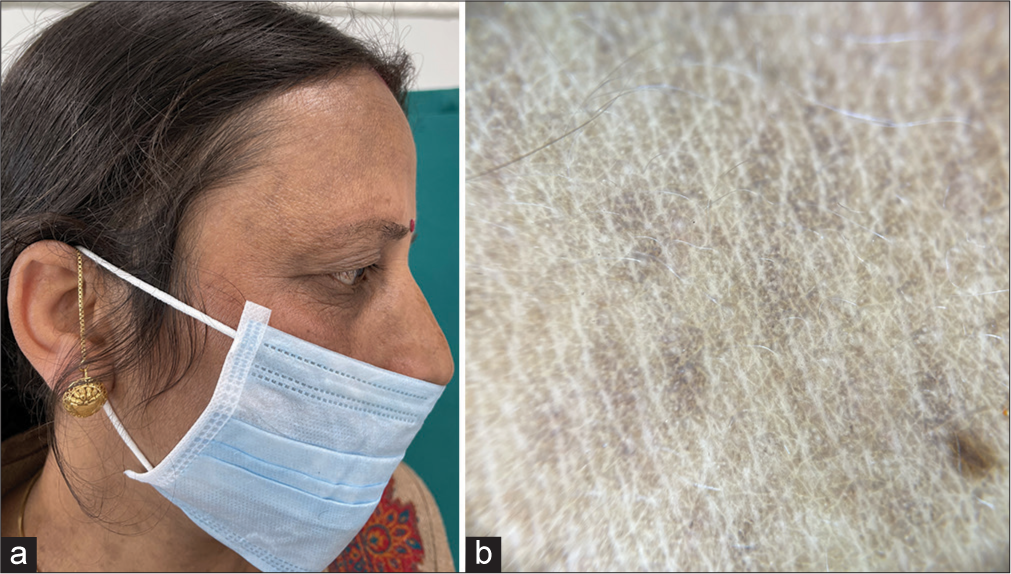
- (a) Presence of multiple brown macules over the temples, cheek, nose, and neck in a female with lichen planus pigmentosus; (b) Dermoscopic examination revealed the presence of perieccrine and perifollicular brown pigment globules with peppering distributed in hem-like pattern (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification).
| S. No. | Entity | Clinical features | Dermoscopy | Histopathology |
|---|---|---|---|---|
| 1. | Maturational hyperpigmentation | Asymptomatic pigmentation. Fine granular surface with indistinct margins blending into the surrounding normal skin. Predominantly involves the sun-exposed areas of the lateral face. |
Accentuated pseudoreticular pigment network, brown globules, and brown rings concentrated around follicular openings | Minimal hyperkeratosis, mild-to-moderate basal layer melanocytic proliferation with slight papillomatosis sans dermal inflammation |
| 2. | Melasma |
Asymptomatic Bilaterally symmetrical, irregular, hyperpigmented patches with blotchy areas of normal skin. Involvement of centrofacial, malar and mandibular areas |
Brown globules in reticular, reticulo-globular, and perifollicular pattern Poorly focused telangiectasias |
Melanin deposition in epidermis and dermis. Melanophages in superficial dermis (mainly appreciated in the dermal type) |
| 3. | Exogenous ochronosis |
Asymptomatic Slate-gray patches with confetti-like hypopigmentation. Involvement of cheeks, forehead, temporal and periorbital skin The use of hydroquinone application is usually present |
The curvilinear or worm-like pattern of gray-brown globules. Patchy erythema and linear telangiectasias |
Irregularly shaped banana-shaped yellowish-brown ochre bodies in reticular dermis |
| 4. | Facial acanthosis nigricans | Velvety patches of pigmentation with thickening and accentuation of skin lines | Linear crista cutis and sulcus cutis. Dark brown or black dots. Perifollicular hyperpigmentation and follicular plugging |
Basketweave hyperkeratosis, acanthosis, dermal papillomatosis, elongated and pigmented rete ridges. |
| 5. | Lichen planus pigmentosus | Symmetric brownish to gray-brown macules. Photo-exposed sites over the face (mainly forehead and temples), neck, and trunk. |
Perieccrine and perifollicular brown or bluish-gray pigment globules ± presence of diffuse, dotted, arcuate, annular, speckled, hem-like, or cobblestone patterns. |
Increased epidermal melanin. Flattening of rete ridges. Melanophages in papillary dermis. |
| 6. | Riehl’s melanosis | Reticulate brown/slate-gray pigmentation ± erythema or edema. Temples, forehead, and malar areas. Continued exposure to allergen present. |
Brown and bluish-gray pigment globules. Reticular network Superimposed brown globules. |
Flattened rete ridges, basal layer degeneration in focal areas, melanin incontinence in the dermis with eosinophils and lymphocytes. |
| 7. | Pigmentary demarcation lines | V or W-shaped hyperpigmented persistent patches on bilateral sides of the face | Accentuated reticular pseudo-network, brown globules. | Increased basal layer melanin with increase seen in the vertical arms of rete ridges. |
| 8. | Frictional melanosis | Symmetric Predominantly over bony prominences of face Uniform dark brown pigmentation |
Dilated follicular ostia with keratotic plugs. Perifollicular brown and blue-gray pigment globules. Broken hair, hair with split ends. White scales |
Irregular acanthosis with antler-like projections of rete ridges. Basal layer melanization, patchy melanin incontinence, and patulous follicular openings. |
| 9. | Post-inflammatory hyperpigmentation | Darker skin types and heterogeneous Hyperpigmentation in prior areas of inflammation or injury. |
Non-specific brown pigment pattern | Increased epidermal pigmentation, melanophages in dermis, perivascular lymphohistiocytic infiltrate. |
Treatment includes the screening for metabolic syndrome along with the use of broad-spectrum sunscreens, topical skin-lightening agents such as hydroquinone, microdermabrasion, chemical peels containing glycolic or salicylic-mandelic acids,[2,3] and the use of camouflage techniques. Given the relatively recent description of the entity with only a few sporadic reports to date, no recommendations or exact guidelines exist in the literature outlining the exact duration of treatment needed for noticeable changes in this psychologically disturbing facial melanosis. However, like other facial melanoses, depending on the type of treatment modality used, treatment should be continued for at least three to six months before switching treatment.
In addition to the disease’s metabolic consequences, the resulting cosmetic disturbances, which are particularly upsetting and undesirable for women, meet the urgent need for raising awareness among dermatologists regarding this relatively new, under-recognized, and frequently misdiagnosed entity. Facial hyperpigmentation is cosmetically and emotionally disturbing to the patients owing to its easy visibility. While no studies are available to directly assess the psychosocial impact of maturational hyperpigmentation, data is available for other disorders such as melasma and post-inflammatory hyperpigmentation. These include embarrassment, anxiety, and depression. Therefore, psychological counseling should also be an important component of management given the associated social stigma.[5] It is important to highlight the metabolic complications associated with the disorder, mandate a timely screening for underlying hyperglycemia, dyslipidemias, and hypertension, if any, followed by prompt referral and intervention accordingly.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Facial hyperpigmentation in skin of color: Special considerations and treatment. Am J Clin Dermatol. 2017;18:215-30.
- [CrossRef] [Google Scholar]
- Maturational hyperpigmentation-a novel cutaneous marker of metabolic syndrome. J Cosmo Trichol. 2017;3:e106.
- [CrossRef] [Google Scholar]
- Maturational hyperpigmentation: Clinico-dermoscopic and histopathological profile of a new cutaneous marker of metabolic syndrome. Pigment Int. 2018;5:54-6.
- [CrossRef] [Google Scholar]
- Clinico-investigative study of facial acanthosis nigricans. Indian Dermatol Online J. 2022;13:221-8.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial impact of acne and post-inflammatory hyperpigmentation. An Bras Dermatol. 2017;92:505-9.
- [CrossRef] [PubMed] [Google Scholar]






