Translate this page into:
Managing patterned hair loss – a hair raising task!

-
Received: ,
Accepted: ,
How to cite this article: Sharma A, Shirolikar M, Mhatre M. Managing patterned hair loss – A hair raising task! CosmoDerma 2021;1:55.
Abstract
Diffuse alopecia wields a significant psychosocial burden by virtue of its clinical presentation and visibility. Patterned alopecia is an umbrella term with the focus point being androgen-mediated alopecias - androgenetic alopecia/male pattern baldness/male androgenetic alopecia and female pattern hair loss/female androgenetic alopecia, both of which have a genetic susceptibility that alters the follicular sensitivity to circulating androgens. Diffuse alopecia affects nearly half the population based on weighted averages. It may present with hair shedding and hair thinning (miniaturization) or a combination. With the female variant, the role of androgens is not fully delineated; hence, the term female pattern hair loss which has replaced prior nomenclature. Managing patterned hair loss has seen a sea change in the last decade, moving well beyond the FDA-approved modalities - topical minoxidil and oral finasteride. Through this short review, the authors have attempted to condense existing information into a ready reference.
Keywords
Diffuse hair loss
Androgenetic alopecia
Male pattern baldness
Alopecia management
INTRODUCTION
Although hair is a non-essential organ, it plays a huge role in our personality and serves as a means of expression for many people. Almost 50% of males are affected with pattern hair loss (PHL) by the age of 50 and even 50% of females. This hair loss can be a source of emotional distress for many.[1]
This article hopes to shed light on patterned hair loss in males and females, and the management modalities for the same.
WHAT IS PATTERNED HAIR LOSS?
PHL is a genetically determined, potentially reversible type of hair loss. It is limited largely to the top of the scalp and is characterized by recognizable patterns of hair loss in men and in some women.[2]
ANDROGENETIC ALOPECIA (AGA) – ERSTWHILE, MALE AGA (MAA) OR MALE PHL (MPHL)
Up to 50% of men have AGA by the age of 50, making it the leading cause of hair loss in males. There is a recognized familial tendency to have AGA with up to 80% of affected individuals have a hereditary predisposition to AGA. AGA does not require androgen levels to be in excess and even a normal level is enough to trigger hair loss in individuals who are prone. AGA characteristically occurs in the mid-front area of scalp and also involves temples and the vertex and this pattern is reproducible.[3]
The hair follicles affected by AGA show miniaturization and inflammation. There is also a variation in the hair cycle with anagen phase shortening each cycle whereas the telogen phase stays the same or increases. Eventually, the anagen phase time is so less that the hair does not reach the scalp surface and the follicular pore is vacant. This miniaturization of the hair follicle is the histological characteristic of AGA. Ultimately, all the primary follicles experience miniaturization and there is detachment of the arrector pili muscle from the secondary follicles. At this stage, the hair loss becomes irreversible.[3]
PATTERNS IN AGA
The clinical appearance of AGA is recognizable straightaway almost universally in most. The pattern of hair loss and its progression has been recorded by Hamilton[4] and Norwood[5] [Figure 1].

- The Hamilton-Norwood scale with extended anterior (A) and vertical (V) patterns for grading androgenetic alopecia in males.
FEMALE PHL (FPHL)
FPHL is the most prevalent form of hair loss in females. FPHL is the preferred term and not AGA in women as there is no certainty of the relationship between androgens and this condition.[6] Patients might start seeing symptoms during adolescence, which progress over time and lead to more pronounced hair loss. FPHL also has a peculiar hair loss pattern and is non-scarring in nature.[7] Just like MPHL, FPHL also shows follicular miniaturization leading to an eventual decrease in the number of hair. The pattern typically involves the frontal, parietal, and central portion of the scalp.[8]
FPHL has three patterns[9]
A generalized decrease in the hair vertex with conservation of the frontal hairline: there are two scales which outline the pattern: Ludwig scale (which has three grades)[6,10] [Figure 2] and the Sinclair scale (which has five grades)[11] [Figure 3]
The Christmas tree pattern, as represented by Olsen, has broadening of the central partition of the scalp. The frontal hairline is not preserved in this pattern[12]
The Hamilton-Norwood pattern which shows hair loss mainly in bilateral parietal and temporal areas.[13]

- The Ludwig scale for female pattern hair loss.
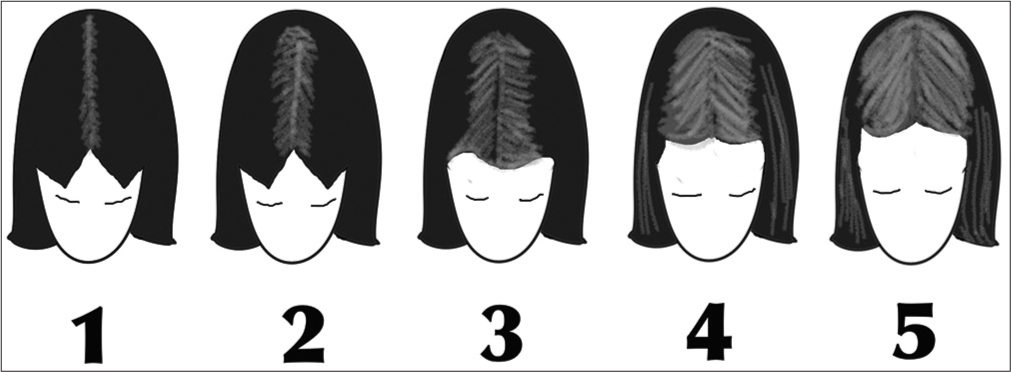
- The Sinclair visual analog scale for female pattern hair loss.
It is interesting to note that all three spare the occipital area.
DIAGNOSIS
History
History taking should include the age at which symptoms appeared, that is, age of onset. Further enquiries about the and period during which symptoms progress to the current state of hair loss should also be made. Family history should be elicited for similar symptoms as well as other hair disorders such as hirsutism or alopecia areata, keeping in mind that a negative family history does not exclude the diagnosis. General medical history and treatments taken should be inquired about with particular importance upon any disorders within 1 year before first signs of hair loss. Also ask for other conditions that could lead to hair fall, for example, iron deficiency, hyper or hypothyroidism, acute or chronic illnesses, dietary history, and medications such as anti-cancer drugs and hormonal supplementation. Lifestyle habits such as smoking and hairstyles that could lead to traction alopecia should also be asked for.[7,14]
For FPHL, an exhaustive gynecological and obstetrical history should be taken which includes age on onset of menses, regularity of menstrual cycle or amenorrhea, hormonal supplements, age of onset of menopause (if applicable), any abortions, births, obstetric or gynecological surgeries, fertility treatments, and signs of hyperandrogenism (hirsutism, hypertrichosis, and acne).[15]
General examination
General examination of the skin should be done including hair and nails so as to rule out other causes of hair loss such as lichen planus, alopecia areata (AA), and iron deficiency.[9] In females, the general examination should also focus on finding other signs of possibly associated hyperandrogenism.
Scalp examination
Scalp examination should identify the pattern of hair loss and the approximate diameter of hair in the commonly involved areas. Findings suggestive of PHL consist of observation of terminal hair loss, disparity of hair caliber, and miniaturization of hair. PHL does not exhibit scarring and should be ruled out if scarring is present. If increased inflammation or sebum production is seen, it could likely worsen the hair loss.[16] Pull test is usually negative in PHL unless performed in the active phase.
Pull test
Pull test is done by holding a bunch of approximately 50–60 strands of hair at their base near the scalp. A firm, but not forceful, pull is then given on the hair.[17] A positive test is when six, that is, 10% of hair are tugged out.[18] Any less than 10% are tugged out, it is considered physiological.[19] This test is performed in all the regions of the scalp, that is, frontal, bi-parietal, bi-temporal, and occipital regions. In telogen effluvium (TE), the test is positive in more than one area and TE should be ruled out. In cases of PHL, the test may be positive only in the affected regions which have active phase. Pull test is a noninvasive, easily performed and repeatable diagnostic technique. Drawbacks of the test include the potential of disparity between physicians performing the test, and that the results may change depending on habits such as shampooing.[7]
Investigations
Trichoscopy: Trichoscope is a scalp dermatoscope and is a non-invasive diagnostic tool. Trichoscopy of PHL shows hair diameter variability more than 20%[20]
Scalp biopsy: Scalp biopsies are not routinely done to diagnose PHL. They are only performed in cases where the clinical features do not provide a definitive diagnosis like in cases, when scalp changes suggestive of cicatricial alopecia or diffuse alopecia areata are present. A 4 mm punch bopsy is taken extending into the subcutaneous fat. The central scalp area is usually biopsied and both vertical and horizontal sections are examined[9]
Trichogram: This involves plucking of hair and analyzing them under the microscope. In cases, where other provisional diagnoses are being considered such as anagen-dysplastic effluvium or a loose anagen syndrome, trichogram may be useful. Trichogram may also be used to detect early stages of PHL which would be seen as inhomogeneous hair shafts. However, in a recent study, dermatoscopy was found to be more useful for the diagnosis of PHL than trichogram[21]
Phototrichogram/Trichoscan: In this technique, a small area of the scalp is trimmed and then photographed.[22] This area is usually tattooed to ensure that follow ups are taken of the same area.[18] The photos help to record the density of the hair and give an idea about the speed at which hair is growing. The division of anagen and telogen hair is also recorded. These photographs can also be stored and compared later.[23] The occipital density is greater than the density in the frontal area in PHL
Blood tests that may be done include – Ferritin, thyroid function test, and an endocrinological evaluation in women suspected of hyperandrogenism.[7]
A practical approach to the diagnosis of patterned hair loss is appended in Table 1 for ready reference.
| History |
|
| General examination |
|
| Scalp examination |
|
| Investigations |
|
TREATMENT
Topical treatment
-
Minoxidil: Minoxidil has been used to treat MPHL since 1984
-
Mechanism of action: There are several hypotheses for the mechanism of action of minoxidil.[24-27]
Vasodilatory hypothesis: Minoxidil solutions of varying concentrations (1%, 3%, and 5%) were applied to the scalp of men with hair loss. There was an increase in the blood supply to the scalp as seen on laser Doppler velocimetry[27]
Minoxidil increases the number of dermal papilla cells by upregulating the mRNA corresponding to vascular endothelial growth factor[28,29]
Minoxidil decelerates the age related degeneration of keratinocytes and decreases the speed at which they exit the germinative pool[1]
Minoxidil adds to DNA synthesis in the follicular and perifollicular cells. The same is not seen in the epidermal keratinocytes.[30]
-
Uses
AGA: Most dermatologists agree that 5% solution of minoxidil provides greater hair growth. An RCT comparing minoxidil 5% solution to 2% solution and a placebo shows an increase in hair growth by 45% in the 5% group compared to the 2% group at week 48.[31] Another RCT comparing minoxidil 5% solution to minoxidil 2% and placebo in women showed an increased hair growth in the minoxidil groups. The difference between 5% and 2% was statistically insignificant. The 5% group reported an increased incidence of local side effects such as itching, irritation, and hypertrichosis[32]
AA: Although minoxidil was first tested for AA, results have not shown sufficient efficacy to get FDA approval. Thus minoxidil is used off-label in AA[1,24,25]
Post hair transplant: A consensus of almost a dozen international hair transplant surgeons reported that the majority of physicians recommend minoxidil as primary treatment in patients who are and are not candidates for hair transplant. The surgeons mentioned that minoxidil increases anagen hair growth and density of hair. It also stabilizes hair loss and augments the growth of miniaturized hair follicles, which makes hair transplant more successful. Minoxidil also reduces the post-transplant TE. Minoxidil is usually withdrawn a few days before surgery so as to reduce any irritation at the site of surgery and minimize bleeding caused by cutaneous vasodilation. Minoxidil is restarted a fortnight later. Better results were seen with 5% minoxidil as compared to 2%[33]
Post-chemotherapy: A randomized, double blind study using 2% minoxidil solution was conducted on breast cancer patients. The patient used minoxidil throughout their chemotherapy and for up to 4 months post-chemotherapy. The study demonstrated that there was a significant reduction in the timespan of hair loss by almost 2 months.[34]
-
Side effects
-
Points to note
Patients are more likely to see results with minoxidil if they already have a large number of partially miniaturized follicles. Hair loss that has happened long ago is difficult to reverse
Minoxidil must be used for at least 6 months before terming it as treatment failure. This will allow hair in other phases of the hair cycle to come back into the anagen phase. Patients are informed that withdrawal of minoxidil will result in stoppage of hair growth. Discontinuation of minoxidil after using for several years will result in hair loss but they would only be those hair follicles that they were genetically programmed to lose.
-
-
Finasteride
-
Mechanism of action
There are two types of the 5-alpha reductase enzyme. Type I is majorly found in the skin and scalp, while type II is seen on hair follicles and the prostate. Both the enzymes convert of testosterone to dihydrotestosterone (DHT).[37] Finasteride is a type II 5-alpha reductase inhibitor (ARI)
Finasteride reduces serum and scalp levels of DHT which increases scalp levels of testosterone.[38]
Topical finasteride minimizes the side effects of its oral form. This is particularly useful in women of reproductive age
Topical finasteride is also effective in males with AGA[39]
-
Supporting studies
-
A placebo-controlled trial was conducted on 52 patients (men and pre-menopausal women) with 0.005% topical finasteride solution. The solution was used twice daily for 16 months. The study demonstrated that the finasteride group had a significant reduction in hair loss, starting from the 6th month of treatment. This reduction continued for the entire duration of the study.[40]
A double-blind RCT study was done on 30 postmenopausal women suffering from FPHL to contrast the efficacy of 3% minoxidil solution alone and with the addition of 0.25% finasteride. Greater results were seen in the group receiving minoxidil and finasteride combination in terms of increased hair diameter at week 24 at week 24, clinical improvements were seen in more than 90% of volunteers in the combination therapy group but it was not statistically significant as compared to plain minoxidil group. The addition of 0.25% finasteride reduced the serum DHT levels after week 24 but the levels were maintained in the normal range throughout this study.[41]
-
-
Side-effects: The use of topical finasteride has shown no systemic adverse effects except lowered serum DHT levels in females suffering from PHL. Local adverse reactions include itching and irritation but have been reported as tolerable.[40,41] More data needed to ascertain the safety in females. Other topical treatment options are:
Prostaglandin analogues: Latanoprost and bimatoprost, both of which are PG-F2 analogs, have been known to prolong the anagen phase and stimulate hair growth.[42] A study in males with PHL using 0.1% latanoprost, showed a growth in hair density and pigmentation at 24 weeks. Whereas studies conducted on PG-D2, showed that an increased PG-D2 level corresponds to with miniaturization of hair follicles and its topical application inhibits hair growth[43]
Ketoconazole (KZ): KZ acts by virtue of two properties – it is anti-inflammatory and also acts as an androgen-receptor antagonist[44]
Melatonin: Melatonin applied topically in 0.1% concentration demonstrated an increase in hair in the anagen phase in PHL[45]
Procapil, Capixyl, Redensyl: A study comparing topical solution of minoxidil to a solution containing Redensyl, Capixyl and Procapil (RCP) demonstrated the RCP group to have a higher researcher score, photographic evaluation score and self-evaluation score than the minoxidil group.[46] However, an expert consensus surmised that more data are needed[47]
-
Oral medications
Minoxidil: Oral minoxidil was first used during the 1970s to treat refractory cases of high blood pressure.[48,49] Oral minoxidil is not the primary treatment protocol in PHL due to unwanted side effects such as postural hypotension, fluid retention, and hypertrichosis. However, FPHL remains an off-label indication for oral minoxidil at a dose of 0.25 mg. Increased hair density has been reported[50]
-
Finasteride
-
Supporting studies
A study conducted on 249 patients, it revealed that finasteride at a dose of 0.2 mg/day could also significantly diminish scalp DHT levels by 60%at week 6[51]
Finasteride was originally studied for re-growth of hair on the vertex.[52] However, a RCT revealed that hair growth was seen in anterior and midscale area as well in males taking oral finasteride 1 mg/day[53]
One RCT on 9 pairs of twins with MPHL revealed the volunteer who took oral finasteride 1 mg/ day had a significant increase in hair growth after 52 weeks than their twin counterpart[54]
Oral finasteride in females with PHL has not been studied as extensively as it can be teratogenic to male fetus. Finasteride in FPHL can be given in a dose of 1–5 mg/day. Finasteride has shown an improvement in hair density and decrease in hair loss in pre- and postmenopausal females[4,55-58]
However, a multicenter RCT conducted on 137 postmenopausal females with FPHL shown no significant change in hair loss by hair count between finasteride 1 mg and placebo after 1 year of treatment[59]
The optimal dose of finasteride for male AGA has been identified as 1 mg/day[60]
There are no recognized drug interactions. It does not appear to affect the cytochrome P450-linked drug metabolizing enzyme
-
Side effects
In men with AGA, reported side effects include ejaculation disorders, decreased sex drive, erectile dysfunction, breast tenderness and enlargement, dizziness, allergic reactions, increased liver enzymes, and depression. Post-finasteride syndrome is also recognized[61-63]
Side effects in women need further study as finasteride is not commonly used to treat FPHL
There have been reports of decreased libido, dry skin, mild acne, headache, dizziness, irregular menstrual cycle, hypertrichosis, and increased liver enzymes.[65,66]
-
-
Dutaseride
-
Mechanism of action: Dutasteride is a second-generation 5α-reductase inhibitor that acts on both the 5α-reductase isoenzyme types. It is thrice as effective at inhibiting type I enzyme and 100 times more potent at inhibiting type II enzyme than finasteride.[67]
-
Supporting studies
A study conducted on 416 males with AGA revealed that dutasteride 2.5 mg/day had a greater efficacy compared to finasteride 5 mg/day and placebo at week 12 and week 24 of treatment[2]
Studies in females are few. A case study of a 46-year-old female with PHL who showed little response to minoxidil and finasteride showed clinical improvement after 6 months of dutasteride 0.5 mg daily and marked improvement after 9 months of therapy[68]
-
Side effects: In a study by Olsen et al., there were no significant differences in side effects in any of the treatment groups, including placebo.[2]
-
Procedures
Light therapy: The mechanism of low-level light therapy (LLLT) is not completely understood. It is thought that the cellular respiratory chain of mitochondria probably absorbs the light energy, causing an increased electron transport and the promotion of cellular signaling, leading to hair regrowth.[69] Various devices are available including a comb, hood, and helmet. However, the efficacy of LLLT devices remains unclear due to the lack of proper studies
Platelet rich plasma (PRP): PRP is an autologous concentration of platelets contained in a small volume of plasma. It contains many growth factors — platelet-derived growth factor, transforming growth factor-alpha, vascular endothelial growth factor, insulin-like growth factor 1, epidermal growth factor, basic fibroblast growth factor, transforming growth factor-beta1, and platelet-activating factor that is released through degranulation. Various studies have reported improvement in regrowth rates after PRP treatments as measured histologically[70]
Microneedling/Dermaroller: It is a minimally invasive procedure in which fine needles are rolled over the skin to puncture the stratum corneum. The needles cause micro-wounds which initiate the wound healing cascade. This stimulates collagen formation, neovascularization, and growth factor production in the treated areas. Micro needling can also be combined with other treatments such as minoxidil, PRP, and topical steroidal medications to increase their penetration[71]
Mesotherapy: This involves injections of growth factors, multivitamins, and amino acids into dermis/ subcutaneous tissue. Mesenchymal stem cells can also be used[72]
Camouflaging: Scalp micropigmentation is a nonsurgical procedure that mimics the appearance of hair follicles.[73] Camouflaging includes concealment of areas of visible hair loss. Hair fibers (keratin-made), masking lotions, topical shading, and scalp spray thickeners, and wigs may be used. Other items for camouflaging include hats, scarves, bandanas, and turbans may be used.[74]
CONCLUSION
Patterned hair loss, centred around the hair follicle is undergoing a tremendous amount of research with rapidly emerging management options in the therapeutic gambit. While existing licensed treatment modalities leave therapeutic need gaps, off-label usage has become more common. These need to be evaluated and positioned to maximise therapeutic outcomes in patients with patterned hair loss.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- Medical treatments for male and female pattern hair loss. J Am Acad Dermatol. 2008;59:547-66.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of dual 5alpha-reductase inhibition in the treatment of male pattern hair loss: Results of a randomized placebo-controlled study of dutasteride versus finasteride. J Am Acad Dermatol. 2006;55:1014-23.
- [CrossRef] [PubMed] [Google Scholar]
- Male androgenetic alopecia In: Eingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, eds. Endotext. South Dartmouth, MA: MDText.com, Inc;
- [Google Scholar]
- Patterned loss of hair in man: Types and incidence. Ann N Y Acad Sci. 1951;53:708-28.
- [CrossRef] [PubMed] [Google Scholar]
- Male pattern baldness: Classification and incidence. South Med J. 1975;68:1359-65.
- [CrossRef] [PubMed] [Google Scholar]
- Female pattern hair loss. J Am Acad Dermatol. 2001;45(Suppl 3):S70-80.
- [CrossRef] [PubMed] [Google Scholar]
- The female pattern hair loss: Review of etiopathogenesis and diagnosis. Biomed Res Int. 2014;2014:767628.
- [CrossRef] [PubMed] [Google Scholar]
- Female pattern hair loss: A clinical, pathophysiologic, and therapeutic review. Int J Womens Dermatol. 2018;4:203-11.
- [CrossRef] [PubMed] [Google Scholar]
- S1 guideline for diagnostic evaluation in androgenetic alopecia in men, women and adolescents. Br J Dermatol. 2011;164:5-15.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97:247-54.
- [CrossRef] [PubMed] [Google Scholar]
- The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair loss in women. J Am Acad Dermatol. 2004;51:189-99.
- [CrossRef] [Google Scholar]
- Current and novel methods for assessing efficacy of hair growth promoters in pattern hair loss. J Am Acad Dermatol. 2003;48:253-62.
- [CrossRef] [PubMed] [Google Scholar]
- Patterned loss of hair in man: Types and incidence. Ann N Y Acad Sci. 1951;53:708-28.
- [CrossRef] [PubMed] [Google Scholar]
- Association of androgenetic alopecia with smoking and its prevalence among Asian men: A community-based survey. Arch Dermatol. 2007;143:1401-6.
- [CrossRef] [PubMed] [Google Scholar]
- European Consensus on the evaluation of women presenting with excessive hair growth. Eur J Dermatol. 2009;19:597-602.
- [CrossRef] [PubMed] [Google Scholar]
- Nudging hair shedding by antidandruff shampoos. A comparison of 1% ketoconazole, 1% piroctone olamine and 1% zinc pyrithione formulations. Int J Cosmet Sci. 2002;24:249-56.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitating hair loss in women: A critical approach. Dermatology. 1997;194:12-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of hair disorders. Semin Cutan Med Surg. 2009;28:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hair diameter diversity: A clinical sign reflecting the follicle miniaturization. Arch Dermatol. 2001;137:641-6.
- [Google Scholar]
- Value of trichoscopy versus trichogram for diagnosis of female androgenetic alopecia. Int J Trichol. 2012;4:19-22.
- [CrossRef] [PubMed] [Google Scholar]
- Critical study of hair growth analysis with computer-assisted methods. J Eur Acad Dermatol Venereol. 2006;20:578-83.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the trichoscan to assess female pattern hair loss. Dermatol Surg. 2009;35:651-5.
- [CrossRef] [PubMed] [Google Scholar]
- Topical minoxidil in the treatment of alopecia areata. Br Med J (Clin Res Ed). 1983;287:1015-7.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia areata treated with topical minoxidil. Arch Dermatol. 1984;120:457-63.
- [CrossRef] [PubMed] [Google Scholar]
- Topical minoxidil for hair regrowth. J Am Acad Dermatol. 1984;11:416-21.
- [CrossRef] [Google Scholar]
- Minoxidil stimulates cutaneous blood flow in human balding scalps: Pharmacodynamics measured by laser Doppler velocimetry and photopulse plethysmography. J Invest Dermatol. 1984;82:515-7.
- [CrossRef] [PubMed] [Google Scholar]
- Minoxidil upregulates the expression of vascular endothelial growth factor in human hair dermal papilla cells. Br J Dermatol. 1998;138:407-11.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of minoxidil on proliferation and apoptosis in dermal papilla cells of human hair follicle. J Dermatol Sci. 2004;34:91-8.
- [CrossRef] [PubMed] [Google Scholar]
- Direct effects of minoxidil on epidermal cells in culture. J Invest Dermatol. 1984;82:90-3.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol. 2002;47:377-85.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, placebo-controlled trial of 5% and 2% topical minoxidil solutions in the treatment of female pattern hair loss. J Am Acad Dermatol. 2004;50:541-53.
- [CrossRef] [PubMed] [Google Scholar]
- The potential role of minoxidil in the hair transplantation setting. Dermatol Surg. 2002;28:894-900. discussion 900
- [CrossRef] [PubMed] [Google Scholar]
- A randomized trial of minoxidil in chemotherapy-induced alopecia. J Am Acad Dermatol. 1996;35:74-8.
- [CrossRef] [Google Scholar]
- Diffuse hypertrichosis during treatment with 5% topical minoxidil. Br J Dermatol. 1997;136:118-20.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of topical minoxidil in the management of androgenetic alopecia. J Am Acad Dermatol. 1987;16(3 Pt 2):677-85.
- [CrossRef] [Google Scholar]
- Tissue distribution and ontogeny of steroid 5 alpha-reductase isozyme expression. J Clin Invest. 1993;92:903-10.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of finasteride (Proscar) on hair growth, hair cycle stage, and serum testosterone and dihydrotestosterone in adult male and female stumptail macaques (Macaca arctoides) J Clin Endocrinol Metab. 1994;79:991-6.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, double-blind controlled study of the efficacy and safety of topical solution of 0.25% finasteride admixed with 3% minoxidil vs. 3% minoxidil solution in the treatment of male androgenetic alopecia. J Eur Acad Dermatol Venereol. 2018;32:2257-63.
- [CrossRef] [PubMed] [Google Scholar]
- Topical finasteride in the treatment of androgenic alopecia, Preliminary evaluations after a 16-month therapy course. J Dermatolog Treat. 1997;8:189-92.
- [CrossRef] [Google Scholar]
- Efficacy of topical combination of 0.25% finasteride and 3% minoxidil versus 3% minoxidil solution in female pattern hair loss: A randomized, double-blind, controlled study. Am J Clin Dermatol. 2019;20:147-53.
- [CrossRef] [PubMed] [Google Scholar]
- New investigational drugs for androgenetic alopecia. Expert Opin Investig Drugs. 2013;22:573-89.
- [CrossRef] [PubMed] [Google Scholar]
- Prostaglandin D2 inhibits hair growth and is elevated in bald scalp of men with androgenetic alopecia. Sci Transl Med. 2012;4:126ra34.
- [CrossRef] [PubMed] [Google Scholar]
- Ketoconazole shampoo: Effect of long-term use in androgenic alopecia. Dermatology. 1998;196:474-7.
- [CrossRef] [PubMed] [Google Scholar]
- topical melatonin for treatment of androgenetic alopecia. Int J Trichol. 2012;4:236.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study between topical 5% minoxidil and topical redensyl, capixyl, and procapil combination in men with androgenetic alopecia. J Cosmetol Trichol 2019:150370987.
- [Google Scholar]
- Expert consensus on the management of androgenetic alopecia in India. Int J Trichol. 2019;11:101-6.
- [CrossRef] [PubMed] [Google Scholar]
- Severe hypertension, Treatment with minoxidil. JAMA. 1975;233:249-52.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of a new antihypertensive agent: Minoxidil. JAMA. 1980;244:73-5.
- [CrossRef] [PubMed] [Google Scholar]
- Female pattern hair loss: A pilot study investigating combination therapy with low-dose oral minoxidil and spironolactone. Int J Dermatol. 2018;57:104-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of finasteride on scalp skin and serum androgen levels in men with androgenetic alopecia. J Am Acad Dermatol. 1999;41:550-4.
- [CrossRef] [Google Scholar]
- Long-term effects of the treatment of polycythemia vera with recombinant interferon-alpha. Cancer. 2006;107:451-8.
- [CrossRef] [PubMed] [Google Scholar]
- Finasteride in the treatment of men with frontal male pattern hair loss. J Am Acad Dermatol. 1999;40(6 Pt 1):930-7.
- [CrossRef] [Google Scholar]
- Finasteride improves male pattern hair loss in a randomized study in identical twins. Eur J Dermatol. 2002;12:32-7.
- [Google Scholar]
- Finasteride for female androgenetic alopecia. Br J Dermatol. 2002;147:812-3.
- [CrossRef] [PubMed] [Google Scholar]
- Finasteride in the treatment of female pattern (androgenic) alopecia: A case report and review of the literature. Cutis. 2012;90:73-6.
- [Google Scholar]
- A woman with iatrogenic androgenetic alopecia responding to finasteride. Br J Dermatol. 2007;156:754-5.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized pruritus: A manifestation of iron deficiency. Arch Dermatol. 1983;119:630.
- [CrossRef] [PubMed] [Google Scholar]
- Lack of efficacy of finasteride in postmenopausal women with androgenetic alopecia. J Am Acad Dermatol. 2000;43(5 Pt 1):768-76.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical dose ranging studies with finasteride, a type 2, 5 alpha-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999;41:555-63.
- [CrossRef] [Google Scholar]
- Side effects related to 5 a-reductase inhibitor treatment of hair loss in women: A review. J Drugs Dermatol. 2016;15:414-9.
- [Google Scholar]
- Atypical post-finasteride syndrome: A pharmacological riddle. Indian J Pharmacol. 2016;48:316-7.
- [CrossRef] [PubMed] [Google Scholar]
- Finasteride: A review of its use in male pattern hair loss. Drugs. 1999;57:111-26.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of finasteride 5 mg (Proscar) on acne and alopecia in female patients with normal serum levels of free testosterone. Gynecol Endocrinol. 2007;23:142-5.
- [CrossRef] [PubMed] [Google Scholar]
- 5 mg/day finasteride treatment for normoandrogenic Asian women with female pattern hair loss. J Eur Acad Dermatol Venereol. 2011;25:211-4.
- [CrossRef] [PubMed] [Google Scholar]
- Finasteride 5 mg/day treatment of patterned hair loss in normo-androgenetic postmenopausal women. Int J Trichol. 2013;5:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Marked suppression of dihydrotestosterone in men with benign prostatic hyperplasia by dutasteride, a dual 5alpha-reductase inhibitor. J Clin Endocrinol Metab. 2004;89:2179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Effective treatment of female androgenic alopecia with dutasteride. J Drugs Dermatol. 2005;4:637-40.
- [Google Scholar]
- Alopecia: A review of laser and light therapies. Dermatol Online J. 2012;18:3.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of platelet-rich plasma for androgenetic alopecia: A review of the literature. Ski Appendage Disord. 2018;4:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of microneedling with platelet-rich plasma plus topical minoxidil (5%) and topical minoxidil (5%) alone in androgenetic alopecia. Int J Trichol. 2017;9:14-8.
- [CrossRef] [PubMed] [Google Scholar]
- Micropigmentation: Camouflaging scalp alopecia and scars in Korean patients. Aesthetic Plast Surg. 2014;38:199-204.
- [CrossRef] [PubMed] [Google Scholar]
- Female pattern hair loss: Current treatment concepts. Clin Interv Aging. 2007;2:189-99.
- [Google Scholar]







