Translate this page into:
Idiopathic multiple eruptive milia: Clinical and dermoscopic correlation: A case report

*Corresponding author: Mohita Mahajan, Department of Dermatology, Government Medical College, Amritsar, Punjab, India. mohitamahajan96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahajan M, Mahajan BB. Idiopathic multiple eruptive milia: Clinical and dermoscopic correlation: A case report. CosmoDerma. 2023;3:179. doi: 10.25259/CSDM_236_2023
Abstract
Milia are multiple, small, benign keratin-filled superficial epidermoid cysts, which may be primary when they occur spontaneously or secondary when they result from skin trauma or disease. Multiple eruptive milia (MEM) refer to a condition characterized by a sudden eruption of multiple milia. MEM may be familial, may occur as part of genodermatosis, or occur spontaneously when they are termed idiopathic. Idiopathic MEM is a rare disease. Hence, we present a case of 14-year-old male having multiple milia on the face along with dermoscopic correlation.
Keywords
Milia
Idiopathic
Eruptive
INTRODUCTION
Milia are multiple, small (1–2 mm), benign, keratin-filled superficial epidermoid cysts derived from pilosebaceous apparatus or eccrine sweat ducts. They are classified as primary when they arise spontaneously or secondary when they result from skin trauma such as burns, subepidermal blistering skin disease, dermabrasion and radiotherapy, topical steroids, or a systemic medication (cyclosporine).[1] Primary milia are very common and may affect up to 50% of neonates; they are common in older children and adults and occur around the eyes, on the cheeks, and forehead.[1] Milia en plaque is a rare form of primary milia that occurs on an erythematous, edematous, or infiltrated base, usually on periauricular and periorbital regions of adults.[2] Multiple eruptive milia (MEM) refer to a condition characterized by the sudden eruption of a large number of milia over a period of weeks to months and may arise spontaneously without any cause when it is described as idiopathic; it may be familial or may be part of a genodermatosis.[3] Idiopathic MEM is a rare skin disease; hence, we present a case of a 14-year-old male having multiple milia on the face along with dermoscopic correlation.
CASE REPORT
A 14-year-old male presented with a history of multiple 1–2 mm skin-colored to pearly white dome-shaped firm, discrete, scattered, papules on the forehead, and cheeks for 1 year. [Figure 1]. Lesions appeared rapidly over a few weeks, were asymptomatic, and were not preceded by any trauma or skin disease. There were no similar lesions elsewhere. There was no history of excessive sun exposure or a similar condition in any family member. The patient was otherwise healthy and had no significant medical history. Dermoscopic examination revealed white clods and homogeneous blue pigmentation (HBP) [Figures 2 and 3].

- Clinical image showing multiple milia on the face.
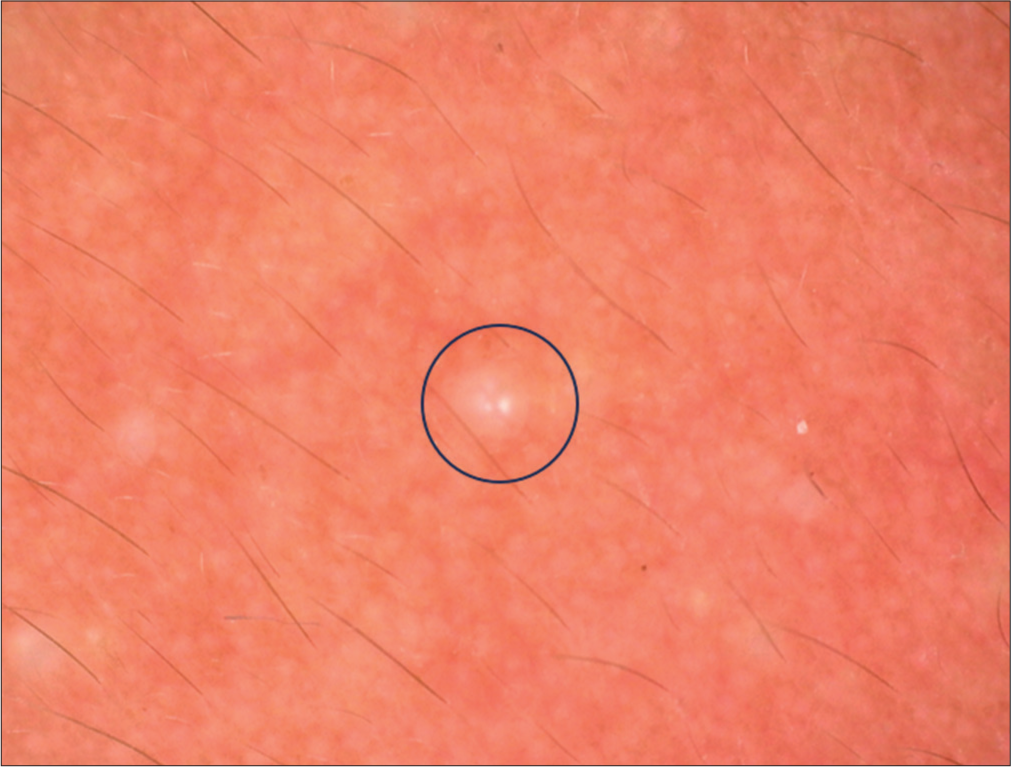
- Dermoscopy of milia showing White clods (Blue circle).

- Dermoscopy of milia showing homogeneous blue pigmentation (Blue arrow).
DISCUSSION
Idiopathic (spontaneous) MEM is a rare disease, and to date, only a few cases have been reported in the medical literature. The age of patients presenting with idiopathic MEM ranges from 9 to 91 years, and no gender difference has been noted in the cases. Lesions have been reported to occur on other body parts such as the scalp, neck, arms, shoulders, upper chest, back, abdomen, and axillae.[4] The trigger for idiopathic MEM is unclear. Sun exposure has been proposed as a trigger for lesions on the face, neck, and shoulders, and scratching and rubbing is other suggested cause for lesions on the covered parts of the body.[4] Familial cases of MEM have also been described and are believed to be transmitted in an autosomal dominant fashion.[1] MEM may be associated with genodermatoses such as Rombo syndrome, basal-cell nevus syndrome, Bazex-DupreChristol syndrome, pachyonychia congenita, and Gardner syndrome.[1] Milia may also be associated with diseases causing subepidermal blistering, such as hereditary forms of epidermolysis bullosa, epidermolysis bullosa acquisita, bullous pemphigoid, bullous lichen planus, and porphyria cutanea tarda. The clinical differential diagnosis of MEM includes eruptive syringoma, miliaria crystallina, eruptive vellus hair cysts, and generalized milia-like idiopathic calcinosis cutis.[4] Dermoscopic examination of milia shows HBP and blue globules.[5] Blue globules and HBP under dermoscopy have been described in basal cell carcinoma, spiradenoma, cylindroma, spiradenocylindroma, ectopic hidradenoma papilliferum, seborrheic keratosis, trichoblastoma, melanocytic nevus, blue nevus, Spitz nevus, and metastatic melanoma (dermoscopic differential diagnosis).[5] Physical treatments often used for milia, such as expression of lesions, curettage, electrodessication, and cryotherapy may be unsuitable for idiopathic MEM because of the large number of lesions requiring treatment which may cause discomfort for the patient. Topical tretinoin cream has been successfully used to clear lesions in 6 weeks in one case.[6] Milia en plaque has been successfully treated with oral etretinate,[7] and it is possible that it may be effective in MEM. Pulse oral azithromycin has been used with great success in a patient.[8] Carbon dioxide and Er: YAG lasers have been used with variable success.[4]
CONCLUSION
MEM is a rare skin condition characterized by the sudden onset of multiple milia occurring mainly on the head, neck, and trunk. Milia are small, benign, 1–4 mm, white keratinous cysts. The lesions are generally asymptomatic and may arise spontaneously or secondary to some underlying condition. They are cosmetically troublesome and difficult to treat. Hence, knowledge about this condition is necessary for early diagnosis and treatment of milia.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Milia: A review and classification. J Am Acad Dermatol. 2008;59:1050-63.
- [CrossRef] [PubMed] [Google Scholar]
- Milia en plaque-milia on erythematous plaque. An Bras Dermatol. 2010;85:895-8.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple eruptive milia: Report of a case, review of the literature, and a classification. J Am Acad Dermatol. 1997;37:353-6.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic multiple eruptive milia occurred in unusual sites. Ann Dermatol. 2010;22:465-7.
- [CrossRef] [PubMed] [Google Scholar]
- Milia: A dermoscopic pitfall. J Am Acad Dermatol. 2017;77:e29-31.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive milia and rapid response to topical tretinoin. Arch Dermatol. 2008;144:816-7.
- [CrossRef] [PubMed] [Google Scholar]
- A case of milia en plaque successfully treated with oral etretinate. Br J Dermatol. 2007;157:1287-9.
- [CrossRef] [PubMed] [Google Scholar]
- Azithromycin therapy for multiple eruptive milia: A report of a case, new treatment option, and review of the literature. Internet J Dermatol. 2009;7:1-5.
- [CrossRef] [Google Scholar]






