Translate this page into:
How I treat acne scars?

*Corresponding author: Renita Lourdhurajan, Department of Dermatology, RENDER Skin and Hair, Chennai, Tamil Nadu, India. drrajan@renderclinic.com
-
Received: ,
Accepted: ,
How to cite this article: Lourdhurajan R, Selvadurairaj S. How I treat acne scars? CosmoDerma 2021;1:46.
Abstract
The approach to managing acne scars is unique to every dermatologist. This depends on the skin type of his/her clientele, the tools, techniques and devices available and/or used, and the protocols developed based on his/her experience with treating acne scars, developed over a period of time. Herein, we share our algorithmic treatment approach to acne scars, which allows for a consultative decision-making together with the patient, while offering adequate flexibility to modify the plan based on treatment response. Eventually, a customized and comprehensive system works best, and a partnership approach signified by a robust self-care home plan, helps accelerate the scar revision process.
Keywords
Acne scars
Key factors
Treatment
Lasers
Microneedling
Treatments and procedures for acne scars are among the most rewarding and the most frustrating of dermatosurgical procedures. Rewarding, because almost any and every modality of scar revision treatment, provides some level of improvement. Frustrating, because the process of scar remodeling is a long drawn, time intensive process, and often requires several sessions before a good clinical end point, can be achieved.
The beginning of any scar revision treatment plan is the establishment of a synchrony between the clinical severity of scarring and the patient’s perception of his/her scars. This sets the stage for planning the treatment sessions, to be able to deliver results matched to realistic expectations. This process becomes easy with an algorithmic approach detailed below.
The key factors to consider are
Scar type
Duration of the scarring process
Gender
Available downtime
Time constraints
Affordability
Infrastructure (energy-based devices) availability
It is common knowledge that recent scars are easier to treat, than well-established scars. With guidelines and clinical experience supporting the concurrent use of isotretinoin to control acne,[1] and procedural treatments like lasers, to work on tissue remodeling, it is always advisable to start acne scar treatment as early as feasible.
Early acne scars, especially those with prominent post-acne erythema, are ideally treated from the first visit. Our approach involves the use of a 1064 nm, picosecond laser, for both acne scars and active acne, or a fractional Co2 laser treatment with topical application of epidermal growth factor, or a combination of these two modalities. To enhance the remodeling, addition of a 4% topical retinol peel also contributes to better resurfacing with faster clearance of lesions. Addition of a home LED device, where feasible, hastens wound repair, and the blue and the red light options are used, twice to thrice weekly. Use of scar repair creams containing allantoin, Cepae extract, and/or Centella extracts, provides an additional support to the home care leg of the scar treatment protocol.
In patients who do not desire to have visible changes from the scar treatment process as considered above, and in those who cannot afford any significant downtime, the modality of choice is a plasma radiofrequency (RF) treatment followed by a fractional picosecond laser toning. Microneedling RF at a low intensity, set to superficial penetration depths, may also work to provide some scar remodeling, when downtime is not available. While this may work for more superficial and early scars, it may be better to consider more robust treatment options for deeper, larger, and well-established scars.
Scars are broadly classified into atrophic and hypertrophic scars [Figure 1].[2] We treat hypertrophic scars with the following options, intralesional triamcinolone acetonide 5–10 mg/ml, and intralesional bleomycin diluted to 1–1.5 U/ml. Intralesional botulinum A neurotoxin is considered for scars located in areas, which are less likely to have significant cosmetic or functional impairment from the toxin. Botulinum toxin at a 1:10 dilution may be considered. When the scars have partially flattened, the above intralesional agents may also be delivered using lasers or microneedling, to prevent complications such as ulcers, dermal atrophy, or pigmentation. Sequential use of the intralesional options may also be considered, [Figure 2]. Papular scars on the chin may benefit from RF microneedling, where other modalities may not be adequate [Figure 3].
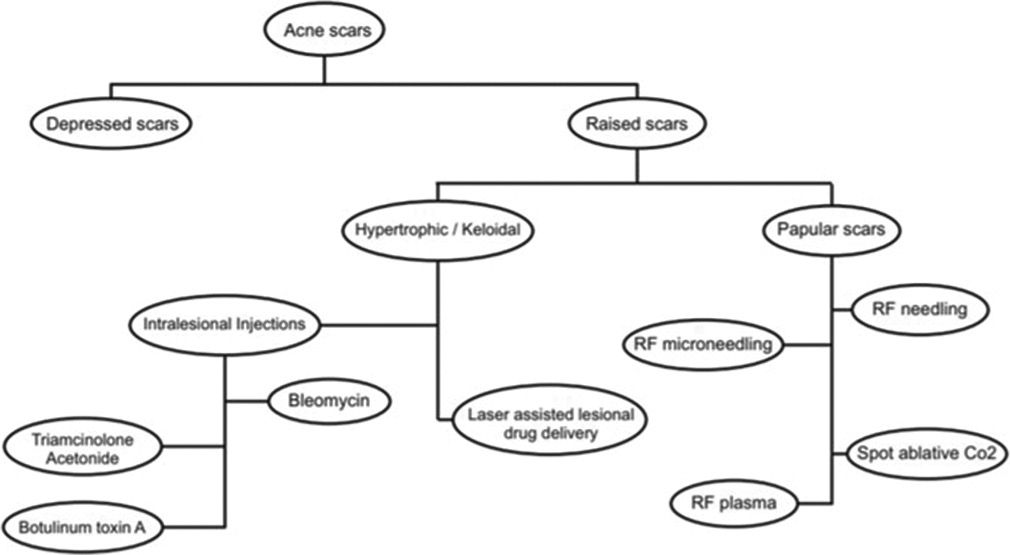
- Approach for raised scars.

- Before and after image showing improvement in scarring, treated by fractional Co2 laser plus 4% retinol peel and laser-assisted triamcinolone acetonide application for areas of hypertrophic and pre-keloidal scarring (arrows), 3 sessions done 2 months apart, in a patient on low-dose isotretinoin for acne management.

- Before and after image showing improvement in papular acne scars on the chin, using radiofrequency microneedling, 6 weeks after 2 sessions, spaced 6 weeks apart.
For atrophic scars, our algorithmic approach is as below [Table 1]. Although listed as device-based options and dermatosurgical options, quite often and practically, more than 1 modality may be offered at one treatment session, depending on scar type, affordability, and the available downtime [Figure 4].

- Before and after image showing improvement in acne scars, 4 weeks after a single session of radiofrequency needling.
| Scar type | Device-based options | Dermatosurgical options |
|---|---|---|
| Macular erythematous | RF needling Spot ablative CO2 laser |
Chemical peels (retinol based) Microneedling |
| Macular hyperpigmented | Picosecond laser 1064 nm Q switched Nd YAG laser |
Chemical peels |
| Rolling scars without significant volume loss | Fractional Co2 laser Fractional picosecond laser (532 nm and 1064 nm) Jet volumetric remodeling RF needling Microneedling RF |
Chemical peels PRP Microneedling Subcision Dermal graft |
| Box car (superficial) | Fractional Co2 laser Jet volumetric remodeling Microneedling RF |
Subcision±Suction Scar excision PRP |
| Box car (Deep) | Fractional Co2 laser Jet volumetric remodeling Microneedling RF |
Subcision±Suction PRP Dermal filler Beard area – FUE for men |
| Ice pick | Spot ablative Co2 laser High fluence picosecond laser (1064 nm) |
Retinol peels TCA peels Minipunch excision Beard area – FUE |
| Superficial elastolysis | Fractional Co2 laser Plasma RF |
Microneedling |
| Predominant volume loss | Jet volumetric remodeling Microneedling RF |
Subcision followed by hyaluronic acid dermal filler Fat grafting |
RF: Radiofrequency, PRP: Platelet-rich plasma, FUE: Follicular unit extraction, TCA: Trichloroacetic acid
Certain standard recommendations always stand. The number of sessions needed to provide significant improvement, remains widely variable between different patients, and between different scar types in the same individual. A customized approach which is constantly updated based on the results and the response of the previous session works much better over, an “x” number of sessions package approach. Furthermore, to allow ideal and adequate collagen remodeling between sessions, a duration of 4–8 weeks between sessions is recommended. The lower gap is suitable for when simultaneously treating active acne, and 8–10 weeks are an ideal spacing between treatments planned for established scars. No individual is likely to have just a single type of scar regardless of the classification system used[3,4] – so a customized approach has to be made and updated periodically based on the clinical response. For example, in men with marginated, boxcar scars in the beard region, a more practical plan would be even to begin the scar treatment with a follicular unit grafting. This would address the problem directly and may even obviate the need for a global rejuvenation, especially if the patient is very clear about his exact goals.
Sun protection remains the cornerstone of a scar treatment program, and a diet rich in antioxidants, collagen, and protein with adequate hydration, use of gentle cleansers, and appropriate post-procedure topical applications that promote faster wound healing, all must be covered in the self-care plan given to the patient. In our experience, weekly use of low strength chemical exfoliators and topical retinol creams has been found to enhance and quicken the remodeling process.
To conclude, a comprehensive and holistic approach works best to provide measurable results in a reasonable time period.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Isotretinoin and dermatosurgical procedures. Indian J Dermatol Venereol Leprol. 2019;85:18-23.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [CrossRef] [PubMed] [Google Scholar]
- ECCA grading scale: An original validated acne scar grading scale for clinical practice in dermatology. Dermatology. 2007;214:46-51.
- [CrossRef] [PubMed] [Google Scholar]






