Translate this page into:
How I manage resistant melasma?

*Corresponding author: Suruchi Garg, Aura Skin Institute, Chandigarh, India. gargsuruchi01@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Garg S, Tuknayat A, Hans T. How I manage resistant melasma? CosmoDerma 2022;2:8.
Abstract
Melasma is a cosmetic disorder with profound psychological impact. Multiple therapies are available for melasma but no therapy is the gold standard. The most of the patients suffer from relapses and recurrences which force the patient to opt for over-the-counter medications containing topical steroids or indigenous medications. Use of these has led to the emergence of complicated cases of melasma which are refractory to the treatment. Along with hyperpigmentation, such patients also have steroid-induced side effects such as rosacea, atrophy of skin, and telangiectasia. Many patients develop exogenous ochronosis due to prolonged use of hydroquinone-based therapies. The present article focuses on the management of these cases of melasma.
Keywords
Melasma
Resistant
Complicated
Platelet-rich plasma
Lasers
INTRODUCTION
Melasma is an acquired hyperpigmentary disorder characterized by well-circumscribed brownish macules to patches predominantly over the sun-exposed areas.[1] It is a cosmetic disorder with profound psychological impact. More than 80% of the patients are female.[2] A multitude of factors such as genetic predisposition, excessive sun exposure, pregnancy, thyroid disorders, drugs like phenytoin, and oral contraceptive pills are implicated in the causation of melasma, leading to an increase in melanogenesis but no major cause can be found in the majority of patients.[2] A number of topical and systemic therapies have come forth for the treatment of this disorder but no therapy has been able to completely cure the patient from this menace. The patient needs to be explained about chronic nature and long-term management plan as most of the patients relapse after stopping treatment.
In a country like India, where a number of over-the-counter medications are easily available to the patient, they end up abusing these agents, especially triple combinations which further complicate the situation. This has led to the emergence of steroid-dependent melasma, steroid-induced rosacea, acneiform eruptions, etc., which are more difficult to treat.
THERAPIES FOR MELASMA
The treatment of melasma requires an individualized approach [Figure 1]. Each patient should be evaluated thoroughly and proper history should be taken regarding the onset, exacerbating factors, and amount of sun exposure to figure out the underlying cause. It is also important to understand the nature of past treatments taken to delineate the further course of action. Along with this, proper nutritional history should be taken to calculate the total protein intake and to look for any signs of vitamin or mineral deficiencies. Role of nutrition in melasma is controversial but a number of recent studies have demonstrated a significant advantage of high-protein diet and good nutrition in the management of such patients. Garg et al. proposed a “hypothesis of conscious selective self-destruction and non-renewal of relatively non-essential tissues.” The hypothesis states that when the body is depleted of important macronutrients such as proteins, body copes up by non-renewal or self-destruction at relatively less important sites such as skin and hair to conserve proteins for more active, and vital tissue like muscles.[3] Following the same ideology, the authors invest a lot of effort planning a high-protein diet calculated based on individual physical activity and lifestyle modifications such as avoiding prolonged starvations or skipping meals. Patients are also recommended early morning breakfast within 2 h of sunrise, respecting the circadian rhythm and hormonal surge. The rationale enables to take care of underlying dietary causes if any. This also helps in building up the skin tissue, thus tolerating the additional treatment options such as chemical peels and lasers and at the same time, minimizing the additional risk of post-inflammatory hyperpigmentation as well as preventing future recurrences in some cases. It is also recommended to test hemoglobin, Vitamin D, B12, iron studies, and thyroid function tests in all patients of melasma.[3]
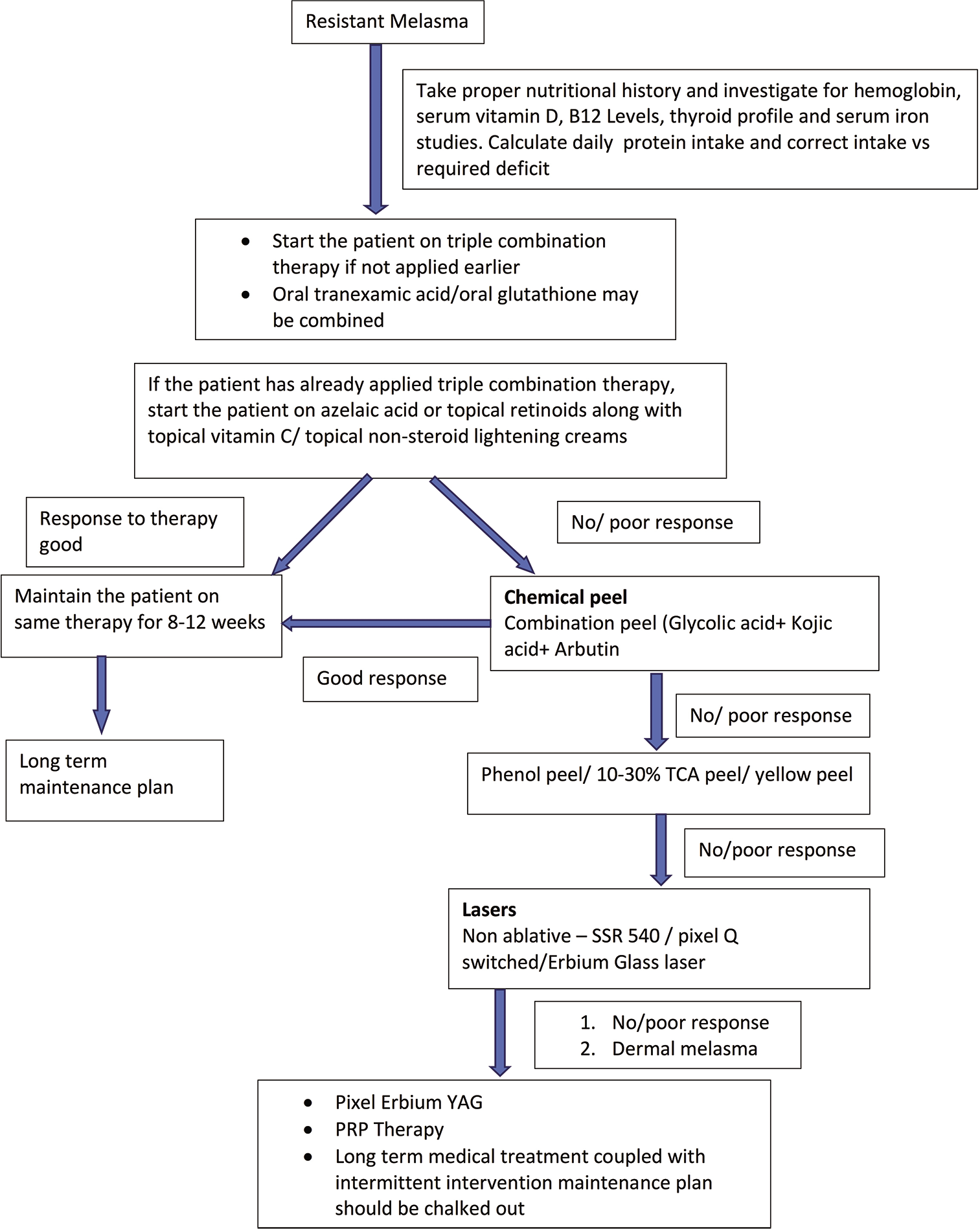
- Approach to a patient of melasma.
After taking detailed history, next step is the assessment of severity in terms of clinical score (mMASI), quality of life score (MelasQoL), and dermoscopy which should be done to maintain baseline data and to assess the response to the treatment. The patient should be photographed in standard five angles at the same background with proper light at every visit in the clinic. All the patients should be counseled about the chronic course of the disease and the necessity for adherence to a long-term treatment plan and lifestyle modifications.
TOPICAL TREATMENT
The use of sunscreen blocking ultraviolet, visible light, and infrared rays is of paramount importance. The individuals with prolonged computer and mobile exposure should be suggested to use sunscreen with additional blue light protection. It is mandatory to prescribe sunscreen with SPF more than 30 to all the Indian patients. Topical depigmenting agents are the first-line therapy for melasma. Triple combination creams containing retinoid, hydroquinone, and steroid are still the mainstay of the treatment.[4] Hydroquinone is a tyrosinase inhibitor and is used in 2–5% in creams. Retinoids reduce tyrosinase transcription and melanin synthesis, thus targeting multiple pathways in synthesis and dispersion of melanin. They also increase epidermal keratinocyte turnover and thus stimulate a decrease in melanosome transfer and loss of melanin. In addition to their synergistic effect, topical steroids also reduce irritation from products such as retinoids. Many side effects are associated with the long-term use of triple combination such as irritation, erythema, and exogenous ochronosis and confetti like hypopigmentation.[4] Thus, many dermatologists prefer to use non-hydroquinone non-triple combination therapies over hydroquinone-based therapies because of greater safety, lesser irritant potential, and better efficacy of these products. Azelaic acid is another plant-based depigmenting agent which also acts by inhibiting tyrosinase enzyme.[5] It is commonly used in combination with a number of agents such as kojic acid and arbutin. Its main side effect is irritation and initial short contact therapy just like retinoids helps in containing irritation part. Topical Vitamin C is a new therapy which is being used rampantly for hyperpigmentation as well as improving the texture of the skin. It works by chelating copper ions which serve as enzymatic cofactors for melanogenesis.[5]
ORAL TREATMENT
Systemic therapies such as tranexamic acid work very well in patients responding poorly to topical treatment. It inhibits plasminogen activator from converting plasminogen to plasmin, decreases the release of basic fibroblast growth factor, and decreases alpha-melanocyte-stimulating hormone.[6] Glutathione, a free radical scavenger, is another systemic therapy which may be tried in such patients with good results.[6]
ADJUVANT TREATMENTS
In patients who are refractory to topical therapies or have deeper component (dermal), chemical peels are a very good option. Glycolic acid in different concentrations can act as a superficial or a medium depth peel which can be used according to the depth of melasma. It can be used as stand-alone peel or in combination with kojic acid peel, citric acid, arbutin, arginine, lactic acid, and salicylic acid or with lasers. Trichloroacetic acid peels (15–30%), low concentration phenol peel (8–10%), yellow peel, pyruvic, and lactic acid combination peels can be used as medium depth peel in dermal melasma.[5]
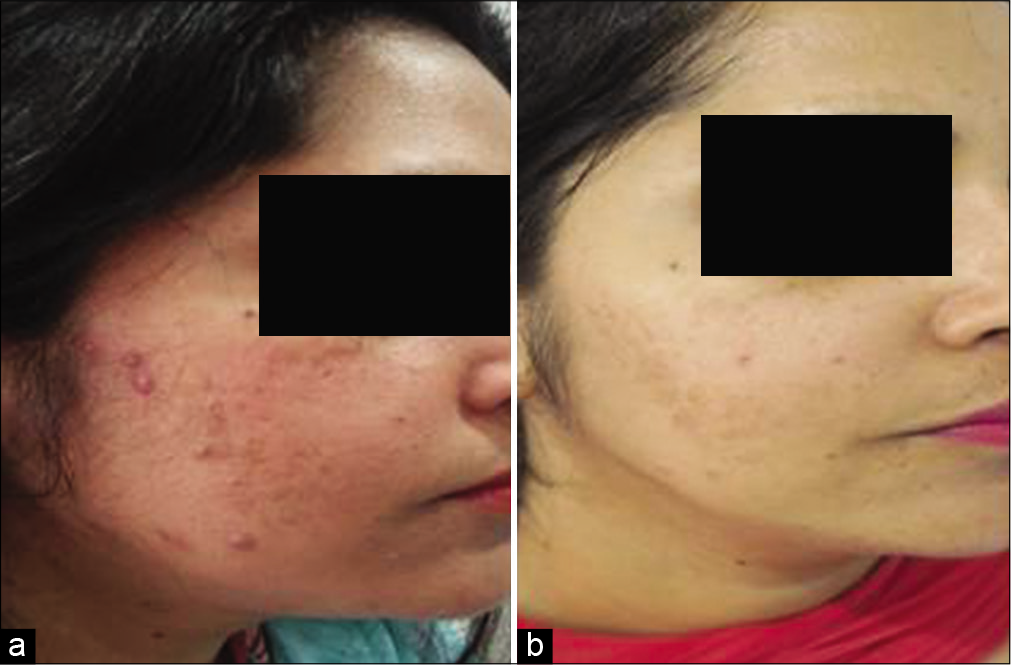
Lasers come forth as the third-line treatment for patients of melasma who are refractory to all kinds of treatments or who require faster results for an impending personal event, etc. Pixel QS Nd: YAG (Harmony XL platform) is the most widely used laser in our practice for the treatment of melasma. The fluence used is <1200 mj/cm2 with 4–5 passes and delivered through pixelated tip. Single pass of Q switch laser with 5 mm conventional tip delivering 1000 mJ/cm2 (laser toning) over pigmented area and 3–4 passes of pixel Q switch delivering 1200 mJ/cm2 over rest of the area can also be used for more resistant areas.[7] The number of treatment sessions varies from 4 to 5 and each session is repeated after every 3–4 weeks. Two to three passes of low fluence, non-ablative lasers like SSR-540 (7–8 J/cm2, double passes) are recommended for more dry, sensitive, and unpredictable skin type [Figure 2a and b]. For dermal melasma resistant to aforementioned lasers, non-ablative erbium glass laser or ablative lasers are usually recommended. Erbium glass laser is recommended to be used at an output of 8–10 W with energy of 24 mJ/pixel, pulse width of 3 msec, and accumulative energy of 600–1200 J (Alma Hybrid). Ablative laser like pixel Erbium: YAG laser (Harmony XL platform) can be used at a fluence of 1100–1200 mJ/p and five passes can be delivered over pigmented area.[8]

- (a) Baseline melasma (b) after two sessions of combination glycolic peel and one session of SSR 540 laser along with conventional treatment of melasma and nutritional support with a significant improvement in MASI score.
COMPLICATED MELASMA WITH ROSACEA AND ACNE
In patients with complicated melasma such as steroid-dependent melasma and steroid-induced rosacea, SSR-540 or IPL-based technology can be used to target hemoglobin and oxyhemoglobin as a chromatophore, thus reducing erythema as well as inducing collagenesis in these patients so as to repair the damaged skin besides improving melasma [Figure 3a and b].[8]
- (a) Baseline pictures – melasma with steroid-induced acneiform eruptions and rosacea (b) after three sessions of SSR540 laser and conventional treatment along with nutritional support.
Platelet-rich plasma (PRP) is an autologous blood product containing platelet alpha-granules which contain multiple growth factors such as platelet-derived growth factor, transforming growth factor beta 1 and 2 (TGF), epidermal growth factor (EGF), platelet-derived angiogenesis factor, and fibrinogen. TGF decreases melanogenesis by downregulating microphthalmia-associated transcription factor promoter activity and inhibiting the expression of paired-box homeo-c gene (PAX 3), which at the protein level, reduces the production of tyrosinase and tyrosinase-related protein 1 and 2.[9] EGF inhibits prostaglandin-E2 expression and tyrosinase enzyme activity.[10] PRP can be used stand alone and with microneedling, radiofrequency, and lasers.[11]
CONCLUSION
Melasma is a complex disorder with multifactorial etiopathogenesis, identification of which will help developing sustainable treatment options with efficacy, lesser side effects, and longer periods of remission. Triple combination continues to be one of the most effective treatments for melasma but reserved only as a pulse therapy (twice a week) and in small quantity in most resistant cases as a long-term plan to minimize the side effects. Relapse rates seem to be most closely tied to severity of melasma at presentation. Chemical peels and lasers are very effective second and third line of treatment for pigment debulking, respectively. Newer treatment options such as tranexamic acid, glutathione, and PRP are also rapidly gaining popularity. Treatment plan of melasma not only requires excellent clinical skills but also correction of underlying nutritional deficiencies, persistent psychological counseling, and lot of patience and hand holding.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
References
- Melasma: A clinical and epidemiological review. An Bras Dermatol. 2014;89:771-82.
- [CrossRef] [PubMed] [Google Scholar]
- Melasma and its impact on health-related quality of life in hispanic women. J Dermatol Treat. 2007;18:5-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary protein deficit and deregulated autophagy: A new clinico-diagnostic perspective in pathogenesis of early aging, skin, and hair disorders. Indian Dermatol Online J. 2019;10:115-24.
- [Google Scholar]
- Melasma treatment: An evidence-based review. Am J Clin Dermatol. 2020;21:173-225.
- [CrossRef] [PubMed] [Google Scholar]
- Melasma: An up-to-date comprehensive review. Dermatol Ther. 2017;7:305-18.
- [CrossRef] [Google Scholar]
- Melasma: Systematic review of the systemic treatments. Int J Dermatol. 2017;56:902-8.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of lowfluence 1064-nm Q-switched Nd: YAG laser with topical 20% azelaic acid cream and their combination in melasma in Indian patients. J Cutan Aesthet Surg. 2012;5:266-72.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective randomized comparative study on 60 Indian patients of melasma, comparing pixel Q-switched NdYAG (1064 nm), super skin rejuvenation (540 nm) and ablative pixel erbium YAG (2940 nm) lasers, with a review of the literature. J Cosmet Laser Ther. 2019;21:297-307.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous intralesional platelet rich plasma improves melasma. Dermatol Ther. 2021;34:e14881.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma is a promising therapy for melasma. J Cosmet Dermatol. 2021;20:2431-6.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: A simultaneous split-face trial. Dermatol Surg. 2011;37:931-8.
- [CrossRef] [PubMed] [Google Scholar]







