Translate this page into:
Giant pretibial cellular fibrous histiocytoma colliding with an epidermal cyst

-
Received: ,
Accepted: ,
How to cite this article: Wollina U, Schönlebe J, Nowak A. Giant pretibial cellular fibrous histiocytoma colliding with an epidermal cyst. CosmoDerma. 2024;4:42. doi: 10.25259/CSDM_27_2024
Abstract
Histiocytomas are common benign tumors of the skin. In contrast, giant histiocytomas are a rarity. We report a 43-year-old male patient, who presented with a 7 × 6 cm large firm tumor on his left lower leg. This was a long-standing lesion, but within the last three months, the tumor developed an exophytic nodule. A skin biopsy revealed an atypical spindle-cell tumor. We decided to perform a complete excision with a safety margin. Complete histopathological analysis confirmed the diagnosis of a collision tumor composed of a cellular fibrous histiocytoma and an epidermal cyst. The resulting defect was temporarily closed by vacuum-assisted closure before eventually a meshed split skin graft was transplanted. Proliferating fibrohistiocytic lesions should be surgically removed, and a careful histopathologic analysis is necessary to avoid delayed diagnosis of possible malignant lesions.
Keywords
Giant histiocytoma
Collision tumor
Surgery
Differential diagnosis
INTRODUCTION
Dermatofibroma or dermal histiocytoma is a common benign mesenchymal tumor occurring worldwide. The peak incidence is between the 2nd and 4th decade of life with a female-to-male ratio of 2:1. This tumor occurs as a slowly growing, well-circumscribed, and firm solitary lesion with a diameter of ≤ 1 cm in about 90% of cases. It is composed of fibroblastic cells with a Grenz zone to the overlying epidermis. Sometimes, the tumor extends into the subcutaneous tissue. The epidermis has a variable degree of acanthosis and hyperpigmentation. The cellular variant is rare. A few recurrent and metastatic cellular histiocytomas have been reported.[1,2]
Their etiopathology is not completely understood, but reactive proliferations after minor trauma (such as insect bites) or clonal proliferations are discussed. There are numerous histological variants including common fibrous, cellular, epithelioid, plexiform, angiomatous, and atypical. Most histiocytomas remain asymptomatic.[1,2]
We report on a long-standing histiocytoma that showed a more rapid growth leading to a large pretibial tumorous lesion.
CASE REPORT
A 43-year-old man presented with a long-standing pretibial tumor on his left leg that showed an unexplained enlargement during the last three months. His medical history was unremarkable despite a thrombophilia that was treated by phenprocoumon 3 mg/d to prevent embolism. He did remember a minor trauma to the tumor site that led to a purulent discharge for some days. The lesion was almost asymptomatic except for a feeling of tension during the last months. On examination we observed a 7 × 6 cm large firm lesion with a central nodule on an erythematous plaque [Figure 1]. We took a skin biopsy, which suggested atypical spindle-cellular proliferations. Therefore, we decided to remove the lesion completely with a safety margin of 2 cm [Figure 2]. Laboratory investigations: Microbiology from a swab of the lesion detected Enterococcus faecalis and anerobic germs, not further specified. They were both sensitive to ampicillin/sulbactam, which was used primarily intravenously and later orally. Thrombocyte count was 223 Gpt/L (normal range 120–340) under treatment. Cholesterol was elevated at 5.9 mmoL/L (normal range <5.2). Differential blood count, sodium, potassium, creatinine, triglycerides, and thyroid-stimulating hormone were all in normal range. The defect was primarily closed by vacuum-assisted closure for 10 days before a meshed skin graft transplantation was performed [Figure 3]. Healing was unremarkable. A complete histopathological examination of the tumor nodule and plaque was performed on hematoxylin eosin-stained sections. In addition, iron staining and immunoperoxidase staining for smooth-muscle actin, desmin, pan-cytokeratin, epithelial membrane antigen (EMA), S-100, Ki-67, CD 31, CD 34, CD 68, and CD 99 were performed [Figure 4]. The nodular part was composed of spindle-type cells without any atypia or mitotic activity. There was a central necrosis of epitheloid cells suggesting remnants of an epidermal cyst. The tumor cells were arranged in a storiform pattern and intermingled with vascular spaces. In the neighborhood, we observed hemosiderin depots and chronic inflammation with numerous capillary blood vessels. The tumor cells were positive for CD 68 and CD 99, but negative for CD 34, smooth-muscle actin, keratin, desmin, and EMA. Some histiocytic cells co-expressed CD 68 and S-100. The endothelial cells expressed CD 31 and CD 34. The diagnosis of a cellular benign histiocytoma in collision with an epidermal cyst was confirmed, while angiomatoid or aneurysmatic histiocytoma or malignant fibrous tumors could be excluded from the study.

- Clinical presentation of the cellular histocytoma with epidermal cysts.
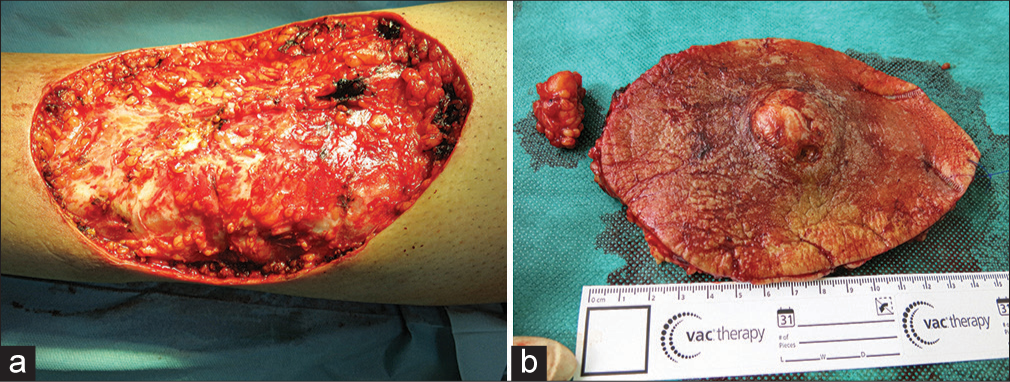
- Surgery of the tumor. (a) Surgical defect resulting after wide excision. (b) Surgical specimen of the lesion.
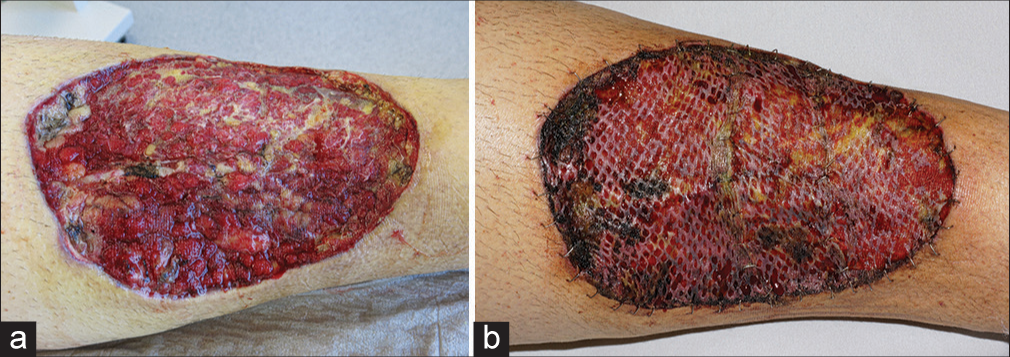
- (a) Stimulated granulation of the wound ground by vacuum-assisted closure. (b) Stable meshed split skin graft on the 6th day after surgery.
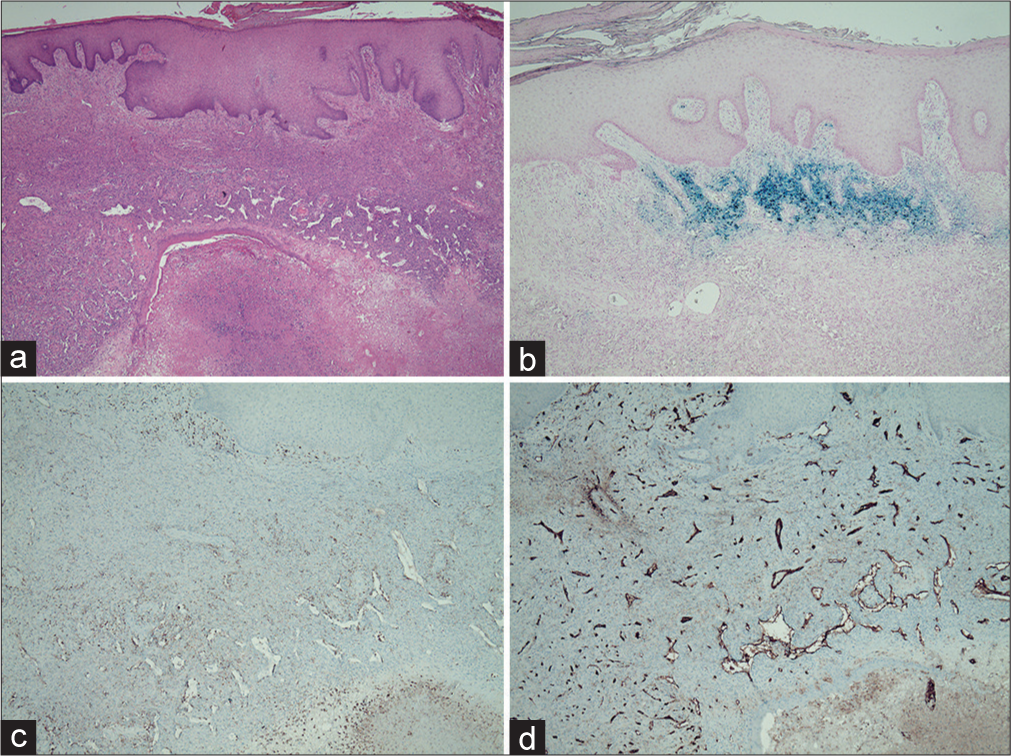
- Histopathology of the tumor lesion. (a) Cellular fibrous histiocytoma with a storiform pattern covered by acanthotic epidermis. On the bottom is a necrotic area where the remnants of an epidermal cyst are still visible (Hematoxylin and Eosin ×2). (b) Iron staining (×4). (c) Positive immunostaining for CD68 (×4) mostly in the periphery. (d) Positive immunostaining for CD31 in the vascular endothelium (×4).
DISCUSSION
We reported a patient with a long-standing pretibial tumorous mass presenting after rapid enlargement. Histological analysis revealed a cellular fibrous dermatofibroma (CFD). The CFD is a rare variant presenting <5% of all cutaneous histiocytomas in histopathological files. The CFD is highly cellular, composed of sheets of eosinophilic, storiform, and fascicularly arranged spindle cells and sclerotic collagen fibers. Small foci of central necrosis can be found in around 10% of cases. There might be a mixed infiltrate of macrophages and lymphocytes at the tumor periphery. The typical localization of CFD is within the dermis, although it can frequently infiltrate subcutaneous tissue. It has a propensity for localization on the extremities without any clear gender predominance as illustrated in the present case report. Relapse of CFD is common (about 10–20% of cases), especially after incomplete resection.[3-5]
Since these tumors are usually self-limited small solitary lesions, the rapid growth of a long-standing pretibial lesion in our patient was a red flag for a possible malignant fibrous proliferation such as Bednar tumor, atypical fibroxanthoma or sarcoma. CFD may show even CD43-positive cells in some cases, which are – in contrast to dermatofibrosarcoma protuberans – localized in the tumor periphery or the bottom of the lesion.[5-7]
Giant tumors are usually defined as lesions exceeding 5 cm in diameter and have rarely been observed among fibrous histiocytomas [Table 1]. Not all tumors reported as “giant” fulfilled the criteria, but 11 tumors between 6 and 40 cm in diameter have been identified.[8-16] Giant benign histiocytomas are a rarity. The exophytic growth seen in the present case might have been due to the collision tumor, that is, an epidermal cyst. Nevertheless, proliferating fibrohistiocytic tumors should be evaluated carefully including a complete histological evaluation to exclude the occurrence of malignancy. We also recommend a complete excision of these lesions since malignant transformations of primary benign lesions have been documented.[2,17,18]
| Reference | Tumor type | Patient/Localization | Treatment |
|---|---|---|---|
| Kaloudis and Spyropoulou 2023 | Nodular | Male/Shin | Surgery with meshed skin graft |
| Panicker et al. 2017 | Plaque-like | Female/Scapular region | Surgery with meshed skin graft |
| Kang et al. 2015 | Deep-infiltrating | Male/Scapular region | Surgery |
| Shi et al. 2015 | Angiomatoid | Female/Abdominal wall | Surgery |
| Angiomatoid | Male/Retroperitoneum | Surgery | |
| Pusztaszeri et al. 2011 | Hemosiderotic | Male/Foot | Surgery |
| Lang et al. 2010 | Cellular | Male/Groin | Surgery |
| Leow et al. 2008 | Plaquze like | Male/Leg | - |
| Hueso et al. 2007 | Classical | Male/Scapular region | Surgery |
| Sehgal et al. 2004 | Deep penetrating | Male/Scapular region | Surgery with meshed skin transplant |
CONCLUSION
Proliferation skin tumors need a histological investigation to exclude malignant transformation. In uncommon cases, a second tumor, independent from the primary may be responsible for tumor growth. Here we presented a rare collision tumor with surgical treatment.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Uwe Wollina is a member of editorial board of the journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Recurrent and metastatic cellular cutaneous fibrous histiocytoma: A case report and literature review. J Cutan Pathol. 2024;51:214-20.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous soft tissue tumors: How do we make sense of fibrous and “fibrohistiocytic” tumors with confusing names and similar appearances? Mod Pathol. 2020;33(Suppl 1):56-65.
- [CrossRef] [PubMed] [Google Scholar]
- Cellular dermatofibroma: Clinicopathologic review of 218 cases of cellular dermatofibroma to determine the clinical recurrence rate. Dermatol Surg. 2019;45:1359-64.
- [CrossRef] [PubMed] [Google Scholar]
- A 10-year analysis of cutaneous mesenchymal tumors (sarcomas and related entities) in a skin cancer center. Int J Dermatol. 2013;52:1189-97.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatofibrosarcoma protuberans: Retrospective single center analysis over 16 years. Open Access Maced J Med Sci. 2018;6:35-7.
- [CrossRef] [PubMed] [Google Scholar]
- Giant cutaneous cellular benign fibrous histiocytoma. J Cutan Aesthet Surg 2023 doi: 10.4103/JCAS.JCAS_179_21
- [CrossRef] [Google Scholar]
- Plaque like giant dermatofibroma: A case report. J Cutan Aesthet Surg. 2017;10:51-3.
- [CrossRef] [PubMed] [Google Scholar]
- A giant, deep, benign fibrous histiocytoma with a palisading pattern. Ann Dermatol. 2015;27:643-5.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological features of angiomatoid fibrous histiocytoma: A series of 21 cases with variant morphology. Int J Clin Exp Pathol. 2015;8:772-8.
- [Google Scholar]
- Giant hemosiderotic dermatofibroma: A case report and review of the literature. Case Rep Dermatol. 2011;3:32-6.
- [CrossRef] [PubMed] [Google Scholar]
- Rapidly evolving giant dermatofibroma. Case Rep Med. 2010;2010:620910.
- [CrossRef] [PubMed] [Google Scholar]
- Plaque-like dermatofibroma: A distinct and rare benign neoplasm? Australas J Dermatol. 2008;49:106-8.
- [CrossRef] [PubMed] [Google Scholar]
- Giant dermatofibroma: Case report and review of the literature. Actas Dermosifiliogr. 2007;98:121-4.
- [CrossRef] [PubMed] [Google Scholar]
- Giant combined dermatofibroma with satellitosis. Clin Exp Dermatol. 2004;29:147-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transformation of benign fibrous histiocytoma into malignant fibrous histiocytoma in the mandible: Case report. J Oral Maxillofac Surg. 2011;69:e285-90.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant dermatofibroma: Clinicopathological, immunohistochemical, and molecular analysis of seven cases. Mod Pathol. 2013;26:256-67.
- [CrossRef] [PubMed] [Google Scholar]






