Translate this page into:
Fractional carbon dioxide LASER for acne scars

*Corresponding author: Dr Mala Bhalla, Department of Dermatology, Government Medical College & Hospital, Chandigarh 160030, India. malabhalla@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Bhalla M, Arora A. Fractional carbon dioxide LASER for acne scars. CosmoDerma 2022;2:22.
Abstract
Acne is a common disease and patients frequently suffer from its distressing sequela of scarring which affects their quality of life. The treatment strategy for acne scars is usually influenced by multiple factors and we need to choose the best fit from amongst the various therapeutic modalities available. Lasers are increasingly being used and fractional ablative lasers create microthermal zones leading to collagen regeneration and reorganization in the target area. Fractional carbon dioxide laser has shown clinical efficacy in skin renewal in atrophic acne scars. Patient selection, counseling, pre, and postprocedure care guidelines form essential factors influencing the procedure outcomes. Here we discuss practical aspects of the use of fractional carbon dioxide laser in acne scar management along with pointers on patient selection, pre and postprocedure care, and side effects.
Keywords
Acne scars
Fractional carbon dioxide LASER
LASER
Acne
INTRODUCTION
Acne is so common, with a prevalence of almost 90% in adolescents, that it is considered almost physiological in its mild form. It may persist to adulthood in about 20% of cases.[1] Though the inflammatory lesions of acne are temporary, post-acne scarring is permanent and has a distressing psychosocial impact with a negative effect on the quality of life.[2] Acne scars can be due to loss or accumulation of collagen, i.e., either atrophic (80–90%) or hypertrophic scars respectively. The more common atrophic scars are further classified morphologically as ice pick (65–70%), rolling (20–30%), or boxcar type (15–25%).[3] Residual scarring is seen in almost 95% of patients irrespective of severity, persistence, and inflammatory lesions of active acne. Usually, different scars coexist and the proportion of different types of scars may differ amongst the patients. The scars have been classified by Goodman and Baran into four types of severity depending on their visibility, skin contour change, and success of makeup for camouflage%[4] [Table 1]. As each patient is unique in their clinical presentation as well as associated factors so the treatment needs to be individualized to provide the best results.
| Grade | Severity | Clinical |
|---|---|---|
| 1 | Macular | Scars can be erythematous, hyper- or hypopigmented flat marks. They do not present a problem of skin contours but only of color |
| 2 | Mild | Mild atrophy or hypertrophic scars may not be visible at a distance of 50 cm or greater, and can be covered with makeup or shadow of shaved beard hair in men. |
| 3 | Moderate | Moderate atrophic or hypertrophic scars visible at social distance of 50 cm or greater, and not easily covered with mascara or shadow, but still can be flattened by manual pressure of the skin. |
| 4 | Severe | Severe atrophic or hypertrophic scars are evident at a distance greater than 50 cm and are not easy covered with makeup, and can not be flattened by manual stretching of the skin. |
Management of acne scars
A large armamentarium of therapeutic modalities is available for atrophic acne scars varying from chemical peels, tissue augmentation-hyaluronic fillers, adipose tissue fillers, collagen induction, and resurfacing with dermabrasion, microdermabrasion, micro-needling, dermatological procedures-scar revision, subcision, radiofrequency subcision, lasers, etc. Physical therapies for atrophic acne scars usually work by causing controlled wound to the skin which activates healing processes of the skin leading to new collagen formation. The patients usually have to undergo multiple sittings of the same therapy, different therapies sequentially, or a combination of multiple modalities depending on the initial presentation as well as response to treatment. Optimum treatment regimens are thus usually tailor-made influenced by multiple factors like the presence of active acne, duration, and type of scarring, available resources, downtime needed, patient affordability.
Role of lasers
Laser therapy has revolutionized the management of various dermatological conditions by virtue of targeting the specific causative agent while inflicting little damage on surrounding tissue. Both ablative and nonablative lasers have been used in the management of acne scars. Ablative carbon dioxide (CO2) laser was believed to be the gold standard for treatment of acne scars as it caused complete resurfacing of the skin leading to rejuvenation but its use was limited by long downtime, increased risk of side effects, and stringent precautions required till complete healing.
Fractional carbon dioxide laser (FCO2)
Carbon dioxide has a wavelength of 10,600 nm and its chromophore is water. It works on the principle of fractional photothermolysis by which microthermal zones causing homogenous thermal damage at a particular level of skin are created. The CO2 beam has limited depth penetration due to its high absorption by the tissue water but by increasing irradiance with very small spot size in fractional approach (120 µm) and using higher or lower pulse energies depths of over 2 mm can be achieved. FCO2 is, thus, a bridge between frankly full ablative and nonablative systems. For maximum results with minimal thermal damage, high peak powers (5J/ cm2) with a short pulse width (<1 ms) are used as 1 millisecond is the thermal relaxation time of skin.[5] This is helpful in reducing the risk of postinflammatory hyperpigmentation.
Carbon dioxide laser causes dermal remodeling, encourages wound healing initiated by extremely high levels of matrix metalloproteinases, and incites increased production of myofibroblasts and matrix proteins such as hyaluronic acid. Clinical and histological studies have shown the efficacy of CO2 laser skin renewal in atrophic acne scars, with an improvement of 50–80%.
Patient selection
Correct patient selection is most important for determining the treatment outcome of any dermatological or aesthetic procedure as the final result is greatly influenced by patient compliance of pre and postprocedure instructions. The patient’s expectations from the treatment should be explored and realistic goals described and agreed upon. Patients with unrealistic expectations, psychological disturbances, and with whom there is a difficult/poor doctor-patient relationship be discouraged from undergoing any kind of procedure as they have an increased tendency to be dissatisfied with the results and more prone to taking legal recourse. The patient should be counseled about the need for multiple sittings and the usual time taken for results to be visible. The patient should preferably not have a major life event in following 1-month minimum and be counseled about expected downtime of 5–7 days even for FCO2 treatment.
Patients with active acne should be advised to wait till the resolution of active lesions before undergoing any procedure as sometimes there may be a flare-up of lesions. A detailed history should include the history of infections (HSV, bacterial, and fungal) especially over treatment site, hypertrophic or keloid scars, and medications. The use of systemic retinoids in the preceding 6 months is no longer considered a contraindication to FCO2 treatment with some studies even showing beneficial effects with concurrent use. Patients on minocycline, nicotine, photosensitizing agents, with active infections, history of hypertrophic or keloid scars, and immunosuppressed should be dealt with great caution.
Preprocedure care
Patients should be advised to avoid excessive sun exposure from 2 weeks prior to treatment. They should also be informed about the need to avoid medications such as ibuprofen, aspirin, and vitamin E around the time of the procedure as they affect the clotting time. Smoking should also be avoided.
Treatment protocol
Written informed consent is essential. Clinical photographs of standardized views should be taken at a standardized distance and with the same camera so that comparison with follow-up photographs is easier. Prior to the procedure, local anesthetic cream is applied for 30–45 minutes and then cleaned with mild cleanser and 70% ethanol. Adequate eye protection needs to be ensured for all present in the treatment room and smoke evacuators deployed.
The laser parameters like pulse energy, power, density, and number of passes need to be set which depends on the type, depth, and duration of scars as well as the device being used. Usually, the static method is used directly on the lesion and dynamic module at the periphery. A less aggressive approach needs to be followed in darker skin types and over-sensitive areas. Laser parameters may be varied for different passes within the same session and also between different sessions depending on patient response.
Our department uses Alma’s Pixel CO2 and recommended parameters with Lite scan handpiece are- Power- 8–12, Energy- 10–30 mj/pixel, Density- 1, Dwell time- 1–2, Passes- 2–3, and a number of sessions- 4 [Figure 1].
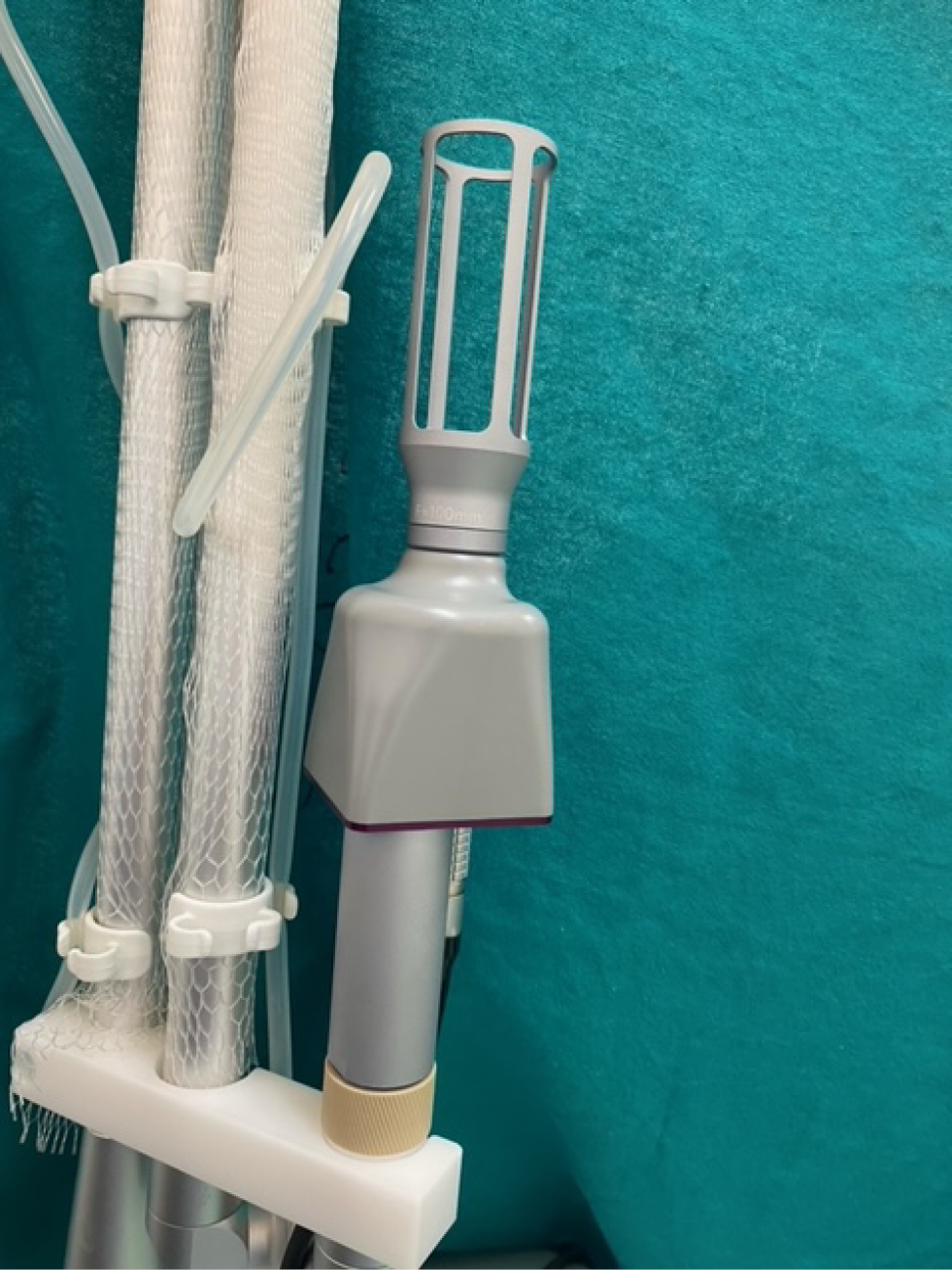
- Articulated arm and handpiece of carbon dioxide machine.
The patient usually feels a burning or tingling during the procedure. Skin cooling with ice packs should be provided 5–10 min after the end of the procedure. Usually, patients may need to undergo about one to three sessions with a duration of 4–6 weeks between two treatments.
Postprocedure precautions
A combination of antibiotics with topical steroids may be given for 2–3 days postprocedure to reduce inflammation and help with barrier repair.[6,7] Studies have shown that postprocedure use of topical steroid cream reduces the risk of postinflammatory pigmentation. Strict photoprotection with sunscreen application postprocedure is advised and should be adhered to for a minimum of 4–6 weeks. Use gentle cleanser and moisturizer with skin-repairing properties. Application of harsh products, makeup, activities such as swimming, and workouts, where infection may be contracted should be avoided.
FCO2 causes transient skin barrier disruption characterized by decreased skin hydration and increased transepidermal water loss so various topical soothing and healing applications have been studied to show improved outcomes. Application of topical 0.5% timolol maleate twice daily has been shown to improve skin barrier function and might promote re-epithelialization.[8] Soothing and repairing creams containing various additives like 5% panthenol, copper-zinc-manganese, and glycoproteins have also been tried in the immediate postprocedure period with beneficial results.[9,10]
Side effects
Pain during the procedure is usually minimal and often described as a pricking sensation. Redness or swelling in the treated area is observed in all which settles in 3–4 days but few patients may have prolonged erythema persisting for a month. Crusting and scaling resolve by 9–10 days.[11] Hyperpigmentation, especially in grid patterns may be observed in patients, more in darker skin types, and may take up to 2 months to resolve. There may be aggravation of inflammation of acne at end of 2 months with acneiform eruption seen in 16% patients [Figures 2 and 3].

- (a) Preprocedure image with acne scars. (b) Immediately postprocedure with red arrow showing erythema and blue arrow showing the ablated area in grid pattern.

- Microthermal zones of FCO2 created in a grid pattern.
Adjuvant therapies
Fractional carbon dioxide laser has been studied for use in combination with autologous platelet-rich plasma, human adipose tissue autografts, autologous adipose-derived stem cells, hyaluronic acid fillers, radiofrequency ablation, and subcision and shown promising results.[12-16]
Expert tips and observations
Thin scars respond better than thick ones
Young skin responds better as it is capable of producing more collagen than old skin
Older and more severe scars may be more refractory for therapy.
Stretching scars while treating may improve results
Individualize parameters
Initially always better to err on side of caution.
CONCLUSION
There is a multitude of options for the management of acne scars and treatment needs to be individualized. There is no magic wand or one-stop quick solution to tackle acne scars. Usually, multiple sittings of multiple modalities are required to produce the best results. FCO2 has shown efficacy and safety in the management of acne scars and may be used alone or in combination with other therapies. The optimum result for each patient depends not only on the device being used but the expertise of the physician as well as patient response and compliance.
Authors contributions
Prof. Mala Bhalla–
Concept and design
Revising it critically for important intellectual content
Final approval of the version to be published.
Dr Astha Arora–
Concept, design, and compilation of data.
Drafting the article.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Acne in Indian population: An epidemiological study evaluating multiple factors. IP Indian J Clin Exp Dermatol. 2020;6:237-42.
- [CrossRef] [Google Scholar]
- Assessment of life quality index among patients with acne vulgaris in a suburban population. Indian J Dermatol. 2016;61:163-8.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of acne vulgaris–a hospital-based study from south India. Indian J Dermatol Venereol Leprol. 2009;75:272-8.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser resurfacing. Semin Plast Surg. 2012;26:125-30.
- [CrossRef] [PubMed] [Google Scholar]
- Fusidic acid cream comparatively minimizes signs of inflammation and postinflammatory hyperpigmentation after ablative fractional CO2 laser resurfacing in Chinese patients: A randomized controlled trial. J Cosmet Dermatol. 2021;20:1692-99.
- [CrossRef] [PubMed] [Google Scholar]
- Topical corticosteroids minimise the risk of postinflammatory hyper-pigmentation after ablative fractional CO2 laser resurfacing in Asians. Acta Derm Venereol. 2015;95:201-5.
- [CrossRef] [PubMed] [Google Scholar]
- Topical 0.5% timolol maleate significantly enhances skin-barrier restoration after fractional carbon dioxide laser treatment for acne scars. Lasers Surg Med. 2021;53:610-5.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of moisturizer containing 5% panthenol, madecassoside, and copper-zinc-manganese versus 0.02% triamcinolone acetonide cream in decreasing adverse reaction and downtime after ablative fractional carbon dioxide laser resurfacing: A split-face, double-blinded, randomized, controlled trial. J Cosmet Dermatol. 2019;18:1751-7.
- [CrossRef] [PubMed] [Google Scholar]
- Snail soothing and repairing cream improves skin hydration after ablative fractional CO2 laser: A split-face randomized double-blinded placebo-controlled trial. Skin Pharmacol Physiol. 2021;34:262-70.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patients. Dermatol Surg. 2009;35:1955-61.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: A split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of atrophic post-acne scars: A split-face comparative study. J Cutan Aesthet Surg. 2021;14:41-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser combined with intradermal injection of autologous platelet-rich plasma versus noncross-linked hyaluronic acid in the treatment of atrophic postacne scars: A split face study. J Cosmet Dermatol. 2020;19:1341-52.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of CO2 laser with subcision in patients with acne scars. J Cosmet Laser Ther. 2016;18:367-71.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of conditioned media of adipose-derived stem cells combined with ablative carbon dioxide fractional resurfacing for atrophic acne scars and skin rejuvenation. J Cosmet Laser Ther. 2016;18:138-48.
- [CrossRef] [PubMed] [Google Scholar]






