Translate this page into:
Erythematous plaque with ulceration on the scalp

*Corresponding author: Arunachalam Narayanan, Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Gorimedu, Puducherry, India. narayanan359@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Narayanan A, Abinaya K, Toi PC, Thappa DM. Erythematous plaque with ulceration on the scalp. CosmoDerma 2022;2:28.
A 58-year-old male farmer presented to our clinic with a red plaque with ulceration and oozing for 4 months. The patient noticed a red lesion over the scalp after a local trauma, which gradually progressed to result in an erythematous, indurated plaque of size 10 × 8 cm over the frontoparietal scalp [Figure 1] during the next 4 months. There were multiple smaller, skin-colored satellite papules, and plaques along the border. There was no lymphadenopathy. He visited a general practitioner who made a diagnosis of scalp psoriasis and treated him with apremilast and tar shampoo unsuccessfully. The patient visited our tertiary care center after developing ulcers and oozing over the lesion. There were no systemic symptoms or loss of weight. He had no headache or vision problems. Histopathology of a biopsy specimen taken from the scalp revealed numerous irregularly-shaped anastomosing vascular channels with atypical endothelial cells [Figure 2]. These atypical endothelial cells had an epithelioid morphology with vesicular nuclei and prominent nucleoli. These cells infiltrated the deeper tissues. There was an increase in mitotic activity (Ki-67 proliferative index-70%). There were numerous ectatic blood vessels surrounded by tumor cells. Few lymphocytic infiltrates were seen interspersed between these tumor cells. However, no necrosis/hyaline globules were identified. On immunohistochemistry, the tumor cells were positive for vimentin, CD31, and CD34, and negative for pan-CK.
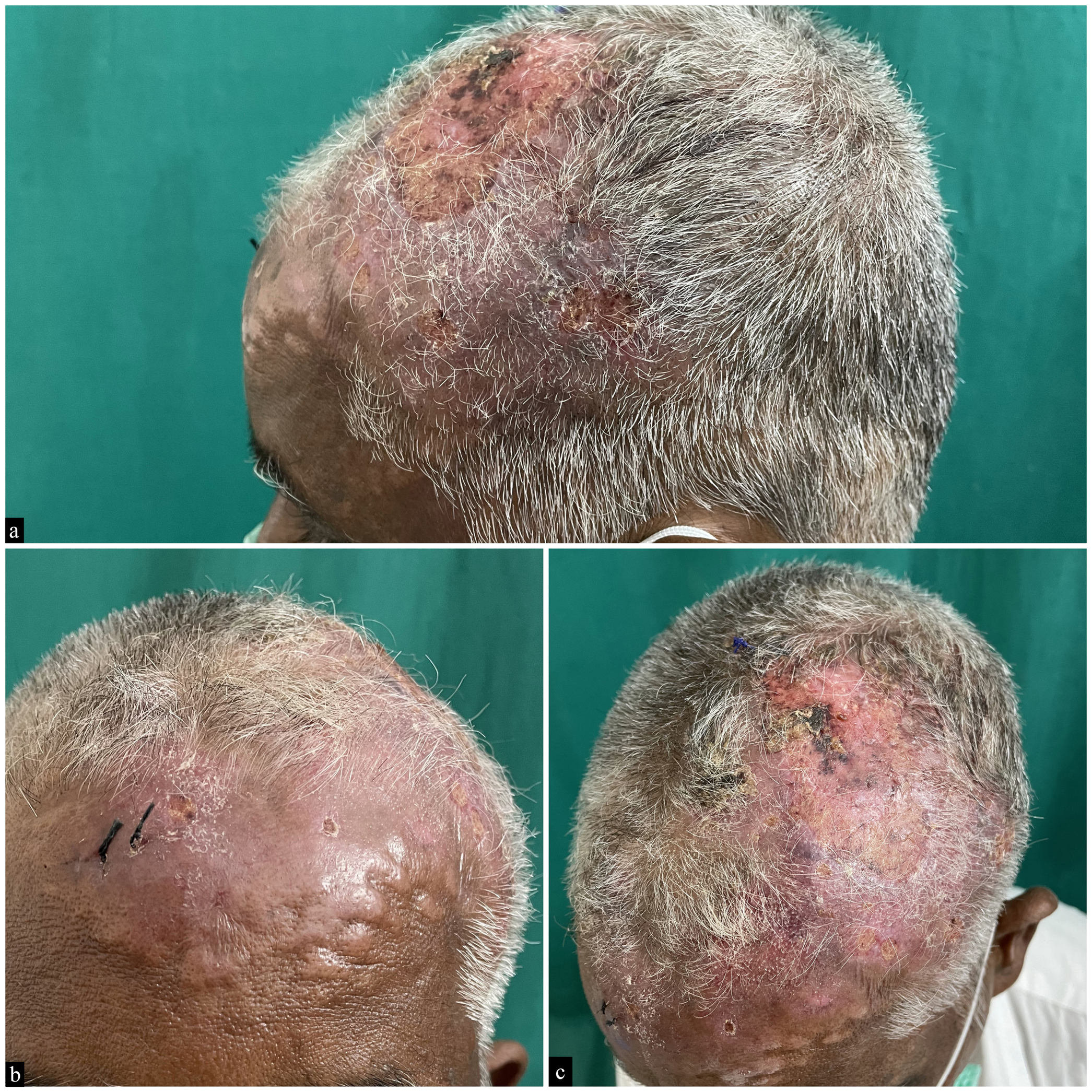
- Erythematous, indurated plaque of size 10 × 8 cm with central ulceration over the frontoparietal scalp, multiple smaller skin-colored plaques along the border.
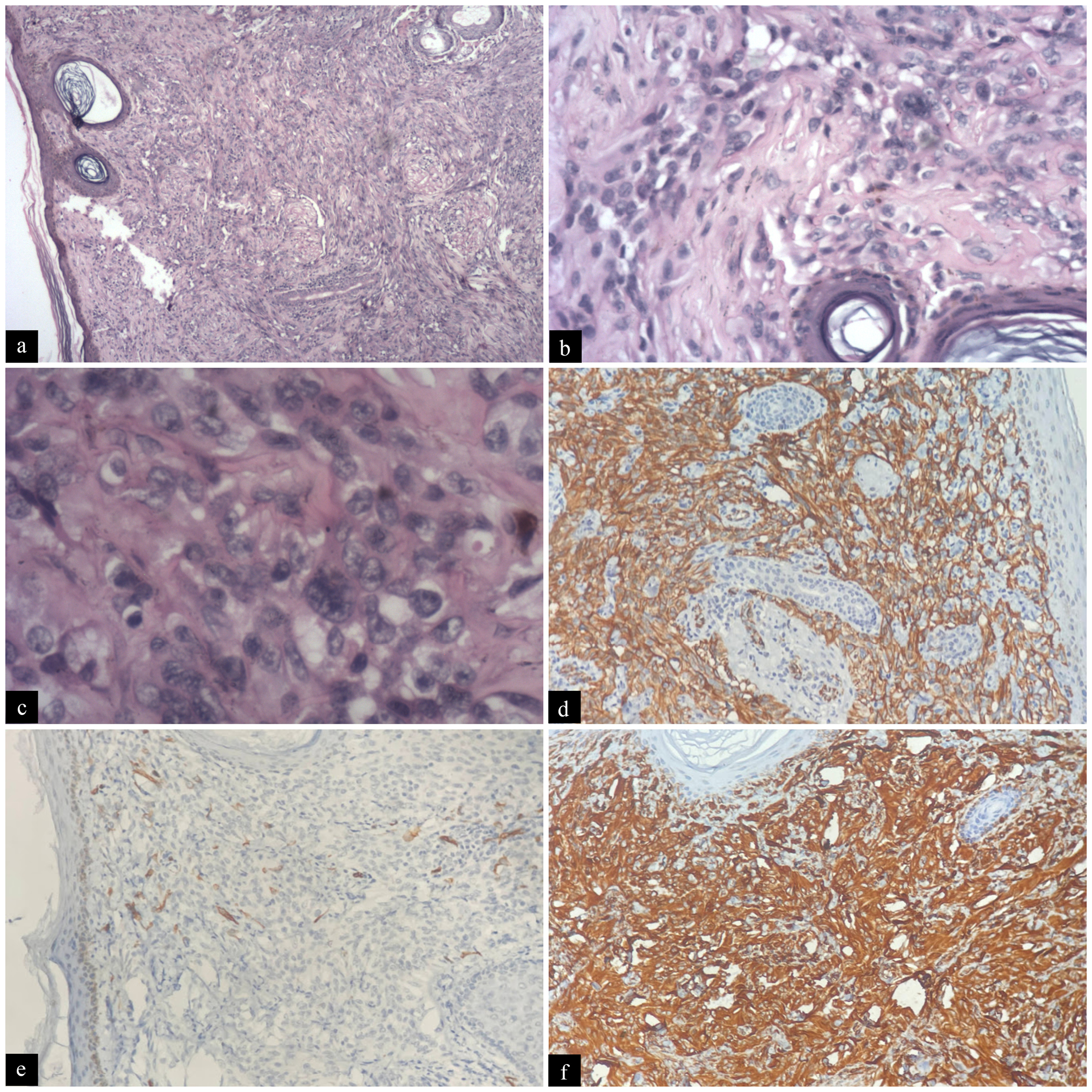
- (a) Histopathology revealed numerous irregularly-shaped anastomosing vascular channels with atypical endothelial cells infiltrating the deeper tissues. (H&E, ×4), (b) There were numerous ectatic blood vessels surrounded by tumor cells. (H&E, ×20), (c) The atypical endothelial cells had an epithelioid morphology with vesicular nuclei and prominent nucleoli, and increased mitotic activity. (H&E, ×40), few lymphocytic infiltrates were seen interspersed between these tumor cells. However, no necrosis/hyaline globules were identified, (d) Immunohistochemistry revealed positive for CD31, (e) CD34, and (f) vimentin.
What is your diagnosis?
Angiosarcoma
DISCUSSION
Angiosarcomas are a clonal proliferation of malignant cells with endothelial differentiation. They occur commonly in Caucasian men and individuals >70 years of age.[1] Angiosarcoma can be primary, post-lymphedema, or postradiotherapy.[2] Exposure to vinyl chloride, thorium dioxide, arsenic, radium, and anabolic steroids have been linked to the development of angiosarcoma. The most common form of angiosarcoma is cutaneous angiosarcoma in the elderly. More than 50% of lesions involve the head and neck area.
The lesions typically start appearing as a benign-appearing bruise-like patch on the central face, forehead, or scalp. Later on, patients start developing facial edema, and with time, lesions progress into violaceous nodules that bleed easily and ulcerate. The lesions spread centrifugally, covering large areas of the head and neck. On the other hand, pediatric cutaneous angiosarcomas are small, unifocal, and occur in the lower extremities in girls.
Angiosarcomas that occur following chronic lymphedema appear as firm, coalescing violaceous nodules or plaques against a background of non-pitting edema.[3] More than 90% of such cases occur following mastectomy and lymph node dissection (Stewart-Treves syndrome). In such cases, the most common site is the inner aspect of the upper arm. Usually, lymphedema occurs 4-27 years before the onset of angiosarcoma.
Angiosarcoma can also occur following radiotherapy.[4] The greater incidence of breast-sparing surgery has resulted in post-irradiation angiosarcoma arising within breast parenchyma and overlying skin. They present as infiltrated plaques or nodules over the irradiated area. The average time for the development of angiosarcoma after radiation is 6 years.
Histopathology of angiosarcoma demonstrates well-differentiated areas of the anastomosing network of sinusoidal vessels lined by a single layer of endothelial cells with nuclear atypia. These cells infiltrate collagen bundles and adipose tissue splitting them apart. The cells have more nuclear pleomorphism and mitotic activity in less well-differentiated areas. They form papillary projections. Poorly differentiated regions don’t have luminal formation. Angiosarcomas stain positively for CD31, CD34, ERG, c-MYC, and Fli-1.[5]
Patients have a poor prognosis with <15% survival over a 5-year period. Patients with angiosarcoma require surgical excision with wide margins. The recurrence rate and metastasis risk are high. Other treatment options include paclitaxel chemotherapy, propranolol plus vinblastine-based metronomic therapy, thalidomide, and radiotherapy.[6] Early recognition of this condition is essential for prompt diagnosis and appropriate treatment.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous angiosarcoma presenting as band-shaped erythematous plaques on the neck. Clin Case Rep. 2021;9:e04925.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary cutaneous angiosarcoma of the scalp with cranial invasion in a patient with metastatic breast cancer. J Clin Aesthetic Dermatol. 2021;14:22-4.
- [PubMed] [Google Scholar]
- Stewart-Treves Syndrome in obesity-associated chronic lymphedema: A case report. J Med Cases. 2021;12:395-9.
- [CrossRef] [PubMed] [Google Scholar]
- S1-Guideline Cutaneous Angiosarcomas—Update 2021. JDDG. 2021;19:1801-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma: A case report. Int J Surg Case Rep. 2021;88:106506.
- [CrossRef] [PubMed Central] [Google Scholar]
- Efficacy of a combination of paclitaxel and radiation therapy against cutaneous angiosarcoma: A single-institution retrospective study of 21 cases. J Dermatol. 2022;49:383-6.
- [CrossRef] [PubMed] [Google Scholar]





