Translate this page into:
Efficacy of erbium yttrium aluminium garnet laser on post-traumatic scars among Indian population – A non-randomized study

*Corresponding author: Ravi Kumar Chittoria, Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. drchittoria@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Chittoria RK, Nishad K, Parthiban BS. Efficacy of erbium yttrium aluminium garnet laser on post-traumatic scars among Indian population – A non-randomized study. CosmoDerma 2023;3:172. doi: 10.25259/CSDM_204_2023
Abstract
Objectives:
The post-trauma scar is a common problem; it can produce physical and psychological difficulties to the patient. The use of ablative and non-ablative lasers based on the fractional approach is emerging as a method to treat scars. However, very limited data are available of the same in patients of South India. In this study, the authors demonstrated the efficacy of ablative fractional resurfacing (AFR) for traumatic scars using a 2940-nm erbium: yttrium-aluminum-garnet (Er: YAG) laser for the treatment of post-traumatic scars in patients of south India.
Material and Methods:
Seventy-three scars were enrolled in adults of age between 18 and 60 years. Each scar was treated four times at 1-month intervals with a fractional ablative 2940-nm Er: YAG laser using the same parameters. Pre-treatment evaluation before the initiation of the treatment and post-treatment evaluation was performed 1 month after the fourth treatment session of laser. The scar was evaluated using Vancouver scar scale (VSS).
Results:
All 73 scars completed the study. After ablative fractional laser treatment, all treated portions of the scars showed improvements, as demonstrated by the VSS.
Conclusion:
This study shows that ablative fractional application of Er: YAG laser treatment of scars reduces scars fairly. The authors suggest that treatment using AFR can be a adjuvant scar management method for improving the quality of life of patients with post-traumatic scars in patients of south India.
Keywords
Post-traumatic scar
Laser therapy
Erbium yttrium-aluminum-garnet laser
INTRODUCTION
Scars following trauma are relatively common. The source of the trauma can vary, such as sharp cuts, lacerations, abrasions, or can be due to burns. Most of the patients are very concerned about scars.[1] There are many established treatments for improving the appearance of scars such as topical or intralesional corticosteroids, dermabrasion, surgical scar revision, chemical peeling, silicone gel or sheet application, compression therapy, and lasers. The laser therapy can be ablative or non-ablative. Lasers such as the carbon dioxide (CO2), erbium: yttrium-aluminum-garnet (Er: YAG), and pulsed dye lasers have all been used with differing success in the treatment of scars.[2] Significant side effects actually limit the use of ablative lasers such as CO2 and Er: YAG laser for skin resurfacing. Due to these potential risks, non-ablative lasers have been developed as a safe alternative to ablative laser resurfacing. However, results of using non-ablative have remained unsatisfactory or might require several treatments to achieve satisfactory results.[1,3] The exact mechanism by which a laser affects scar remodeling is not clear, but lasers may influence the secretion of various cytokines and growth factors by stimulating a variety of as yet unelucidated cellular responses and blood vessels.[1] Other opinion is that the fractional photo thermolysis causes controlled and limited dermal heating which initiates a cascade of events which normalize the collagenesiscollagenolysis cycle.[4] Recently, the use of ablative and non-ablative lasers based on the fractional approach is emerging as a strategy for the treatment of scars and has been demonstrated to be safe, and also, it improves the appearance of the scars. However, limited data are available on the efficacy of fractional laser treatment of post-traumatic scars in the South Indian population. In this study conducted in a tertiary care center in South India, the post-trauma scars were given 2940-nm Er: YAG laser and scars were followed up.
MATERIAL AND METHODS
The study was conducted in the department of plastic surgery in a tertiary care center in South India, from May 2020 to May 2021. Ethical committee clearance obtained before the starting of the study and informed consent from the patient was taken from all patients. Total of 73 scars were enrolled for the study. The scars were enrolled randomly; all well-healed post-traumatic scars in adults (18–60 years) were enrolled.
Inclusion criteria
The following criteria were included in the study:
Well-healed post-traumatic scars before development of abnormal scarring, hypertrophic scar and keloid
Adult population (18–60 years).
Any patients with history of photosensitivity, pregnancy, lactating-mothers, patients on immunosuppressants known keloidal tendency, patients on anticoagulant treatment, patients on isotretinoin therapy, and any patients who have already received ablative resurfacing treatment within 1 year were excluded from the study. The subjects who had steroid therapy and immunomodulator therapy for scar prevention were not included in our study. The well-healed scars were included randomly. The comparison was not made between new scar and old scar in our study. Informed consent was obtained from patients satisfying inclusion criteria. Clinical photograph was taken twice, one baseline before starting the treatment and one after 1 month post-treatment. The digital images of the scar was taken after getting consent using digital camera (dual 16MP + 20MP) 1× zoom from suitable height. The scar was examined and findings documented, the height of the scar was measured using calipers. Vascularity was tested using blanching with glass slide. Vancouver scar scale (VSS) score was calculated at baseline and 1 month after the completion of the treatment. The VSS was the first validated scar assessment tool for burn scars, introduced in 1990, and still widely used today. The scale evaluates four parameters: Scar height and thickness, pliability, vascularity, and pigmentation, resulting in a score from 0 to 13.
Each scar received four sessions of laser using Er: YAG .at one month of interval using it (Er: YAG laser, Twain 2940, Quanta System S.p.A., Italy) in ablative mode and thermal mode at wavelength 2940 nm, fluence 1–2 J/cm2, pulse width 300 ms, and spot diameter of 4 mm/9 mm. Two laser passes of 400 mJ in short pulse mode (pulse duration 0.30 ms) and one pass of 800 mJ in long pulse mode (pulse duration 1 ms) were performed on scars during each treatment session.
Statistical analysis
Statistical analysis was performed using IBM statistical software, SPSS Statistics version 27 (IBM Inc.). Normally distributed data were expressed as mean ± standard deviation. Data were expressed as median (interquartile range), when assumption of normality was violated (Shapiro–Wilk test, P < 0.001). Outliers were identified on visual inspection of the box plots. Chi-square tests were used for proportions. Independent t-tests were done to ensure group similarities at baseline. A one-way repeated measure analysis of variance (ANOVA) was done to determine whether there are any statistically significant differences between the means of three or more levels of a within-subjects factor over time. P <0.05 was considered statistically significant. The Pearson product-moment correlation was used to determine the strength and direction of a linear relationship between two continuous variables. Pearson correlation coefficient, denoted as r (i.e., the italic lowercase letter r), measured the strength and direction of a linear relationship between two continuous variables. Its value can range from −1 for a perfect negative linear relationship to +1 for a perfect positive linear relationship. A value of 0 (zero) indicates no relationship between two variables.
RESULTS
The mean age of patients was 35.2 ± 7.8 (range, 18–50 years), respectively. Table 1 and Figure 1 show age distribution of study participants.
| Age group | n(%) |
|---|---|
| Less than 20 | 2 (2.7) |
| 20–30 | 31 (42.5) |
| 30–40 | 19 (26) |
| More than 40 | 21 (28.8) |
| Total | 73 (100) |
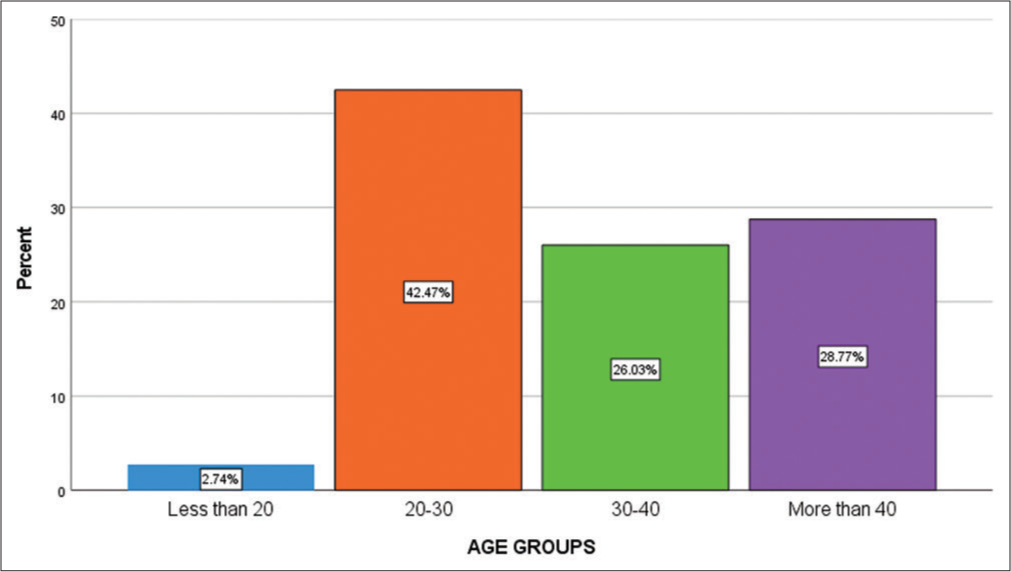
- Age groups.
There were 43 males with a male-female ratio of 1.4:1. Table 2 and Figure 2 show gender distribution.
| Gender | n(%) |
|---|---|
| Male | 43 (58.9) |
| Female | 30 (41.1) |
| Total | 73 (100) |
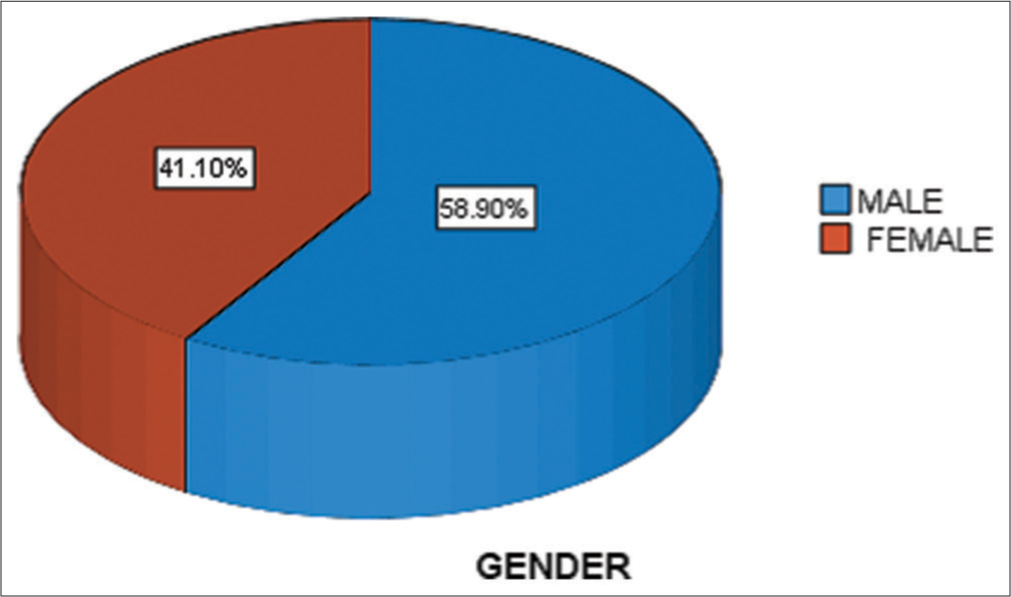
- Gender.
The type of scar is mentioned in Table 3 and Figure 3, respectively.
| Scar type | n(%) |
|---|---|
| Post-burn scar | 18 (24.7) |
| Post-traumatic scar | 8 (11) |
| Amputation stump scar | 5 (6.8) |
| LSCS scar | 2 (2.7) |
| Electrical burn scar | 7 (9.6) |
| ALT flap | 4 (5.5) |
| STSG | 7 (9.6) |
| FTSG | 3 (4.1) |
| Fasciotomy scar | 4 (5.5) |
| Healed scar | 5 (6.8) |
| Venesection scar | 2 (2.7) |
| Post-operative scar | 4 (5.5) |
| Keystone | 1 (1.4) |
| SFJ ligation | 1 (1.4) |
| Ischial rotation | 1 (1.4) |
| PBS scar | 1 (1.4) |
| Total | 73 (100) |
LSCS: Lower segment cesarean section, ALT: Anterolateral thigh flap, STSG: Split thickness skin graft, FTSG: Full-thickness skin graft, SFJ: Saphenofemoral junction, PBS: Post-burn scar
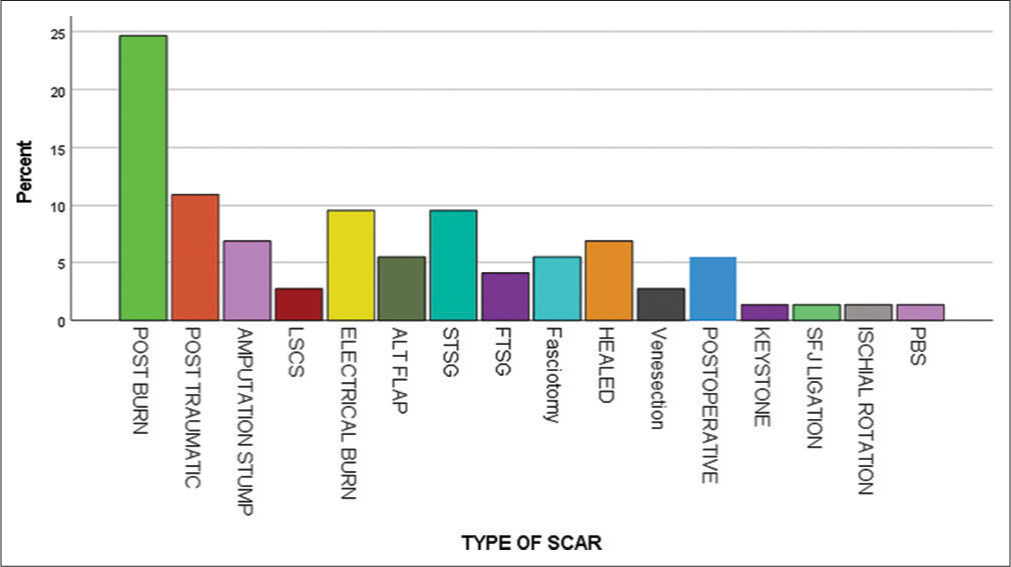
- Type of scar.
The socioeconomic status of study participants is shown in Table 4 and Figure 4. The co-morbidities status of study participants is shown in Table 5 and Figure 5.
| Socioeconomic status | n(%) |
|---|---|
| Low | 44 (60.3) |
| Middle | 24 (32.9) |
| High | 05 (6.8) |
| Total | 73 (100) |
| Comorbidity | n(%) |
|---|---|
| Traumatic paraplegia | 3 (4.1) |
| Venous thrombosis | 12 (16.4) |
| Nil | 58 (79.5) |
| Total | 73 (100) |
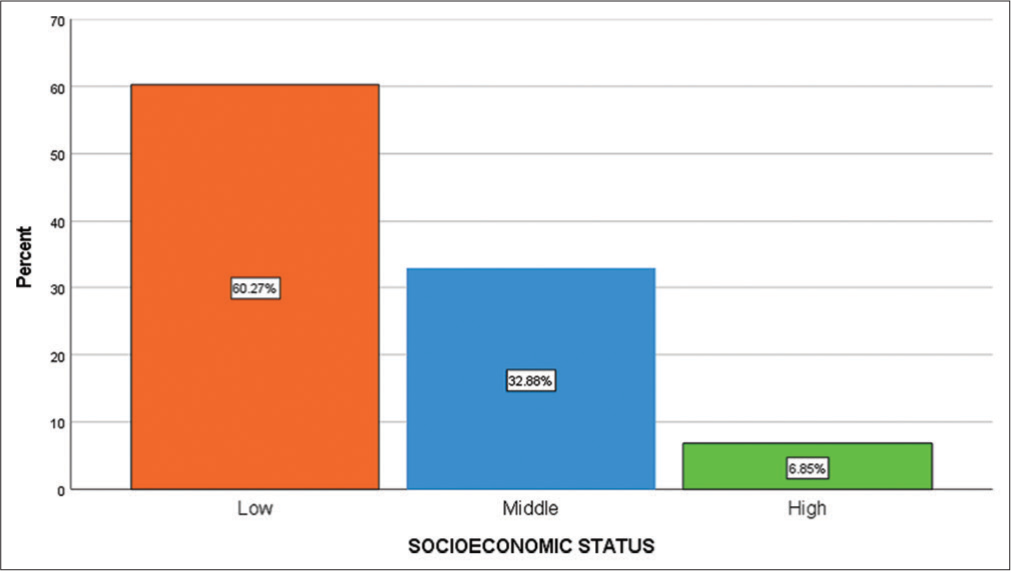
- Socioeconomic status.
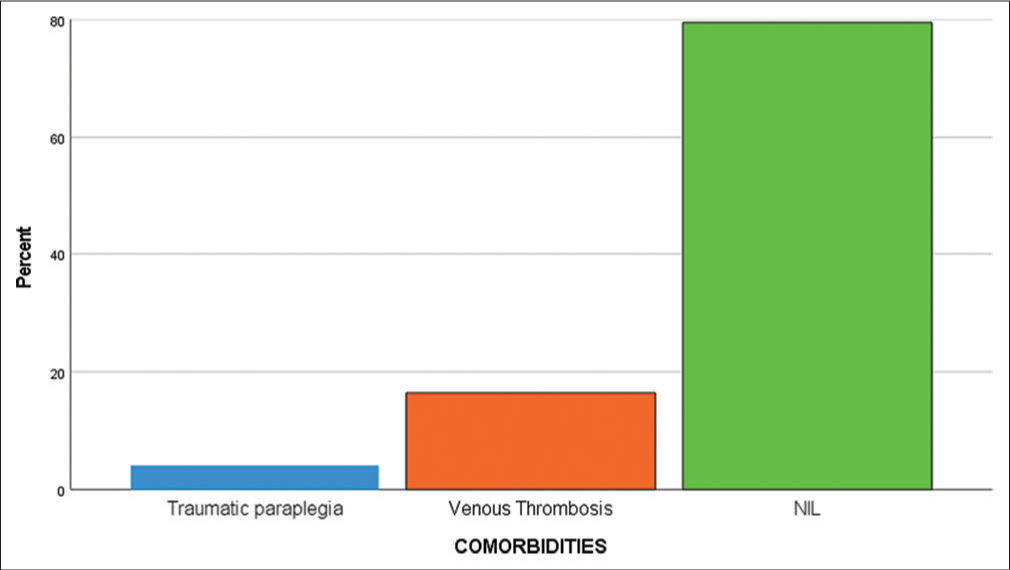
- Co-morbidities.
The pre-procedural and post-procedural VSS parameters are compared in Table 6 and Figure 6. There was a significant difference in vascularity, pigmentation, pliability, and height after laser application (paired t-test, P = 0.001, 0.006, 0.001, 0.001, and 0.001, respectively).
| VSS parameter | Pre-procedural | Post-procedural | P-value |
|---|---|---|---|
| Vascularity | 2±0.8 | 1.3±0.7 | 0.001 |
| Pigmentation | 1.47±0.6 | 1.2±0.6 | 0.006 |
| Pliability | 2.1±0.8 | 1.5±0.7 | 0.001 |
| Height | 1.6±0.7 | 1±0.6 | 0.001 |
| Total score | 6.6±1.6 | 3.2±1.9 | 0.001 |
VSS: Vancouver scar scale
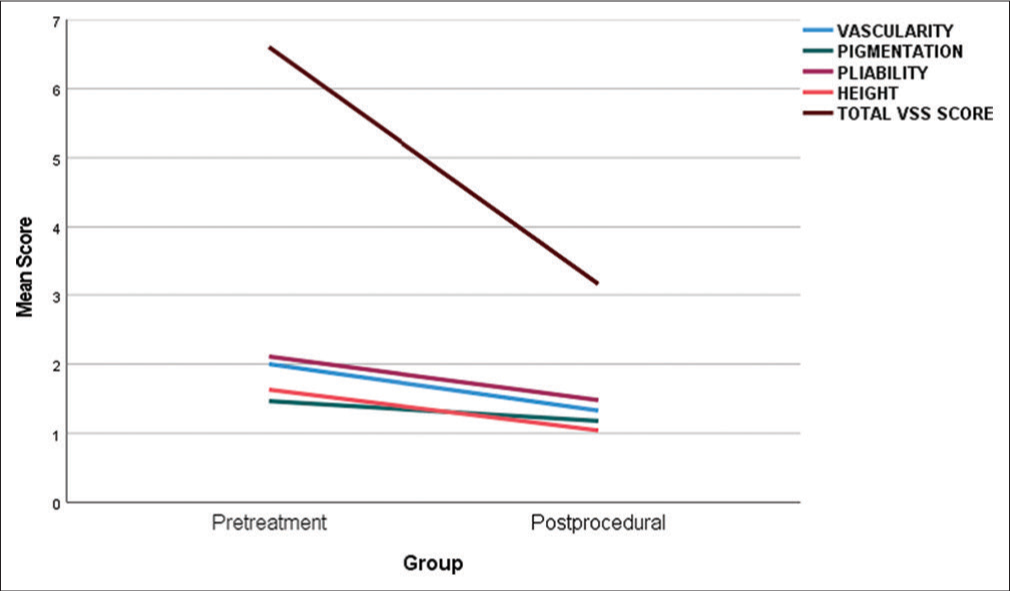
- VSS score Pre-procedural vs Post-procedura.
The mean pre-procedural total VSS score and post-procedural VSS score [Table 7 and Figure 7] did not significantly differ between age groups (ANOVA P = 0.358 and 0.573), respectively.
| Age group | Pre- procedural VSS | P-value | Post- procedural VSS | P-value |
|---|---|---|---|---|
| Less than 20 | 8±1.4 | 0.358 | 5.5±0.7 | 0.573 |
| 20–30 | 6.8±1.5 | 5.7±1.2 | ||
| 30–40 | 6.6±1.6 | 5.7±1.6 | ||
| More than 40 | 6.2±1.7 | 5.2±1.5 |
VSS: Vancouver scar scale
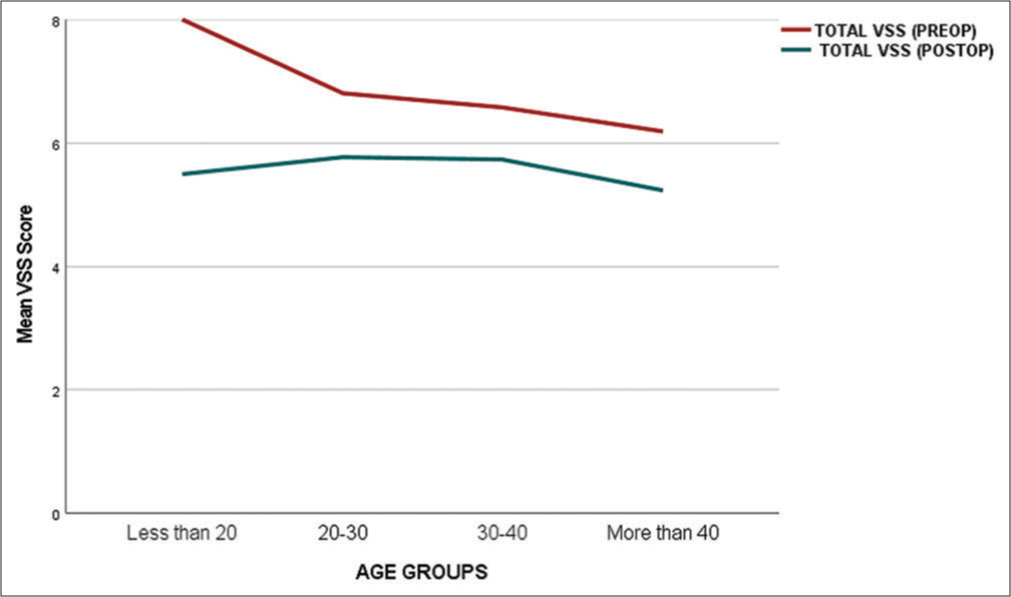
- Relation of VSS score with age groups.
The mean pre-procedural total VSS score and post-procedural VSS score [Table 8 and Figure 8] was significantly different between males and females (independent t-test, P = 0.28 and 0.029), respectively.
| Gender | Pre- procedural VSS | P-value | Post- procedural VSS | P-value |
|---|---|---|---|---|
| Male | 6.2±1.7 | 0.028 | 2.9±0.9 | 0.002 |
| Female | 7±1.4 | 3.5±0.8 |
VSS: Vancouver scar scale
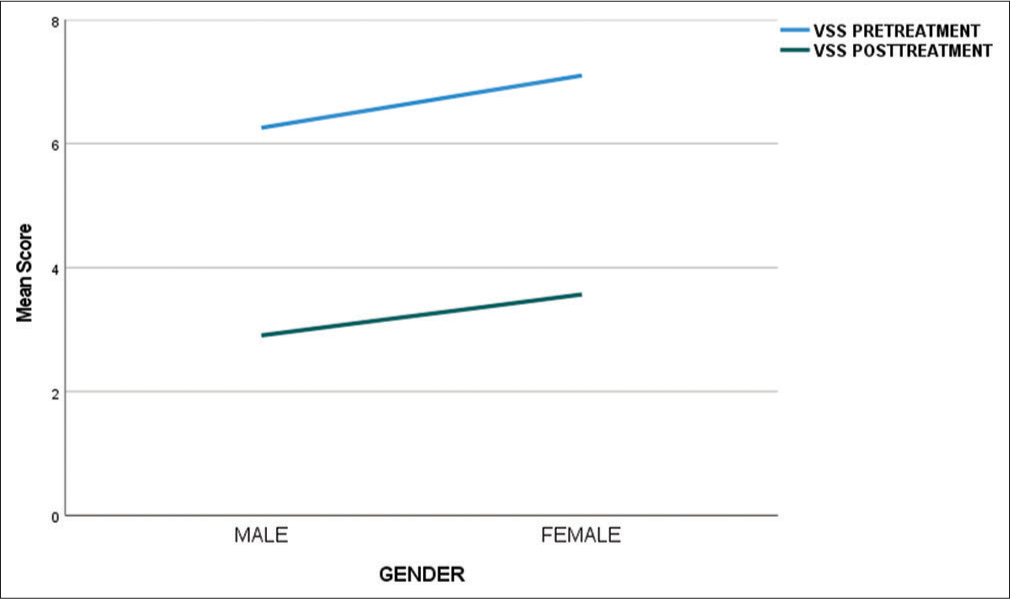
- Relation of VSS score with gender.
The mean pre-procedural total VSS score [Table 9 and Figure 9] was not significantly different between comorbidities (ANOVA P = 0.369). However, post-treatment VSS score was significantly different between the comorbidities (ANOVA, P = 0.028).
| Comorbidity | Pre- procedural VSS | P-value | Post- procedural VSS | P-value |
|---|---|---|---|---|
| Traumatic paraplegia | 7±2 | 0.369 | 4±1 | 0.028 |
| Venous thrombosis | 7.2±1.5 | 3.7±0.5 | ||
| No comorbidity | 6.5±1.6 | 3±0.9 |
VSS: Vancouver scar scale
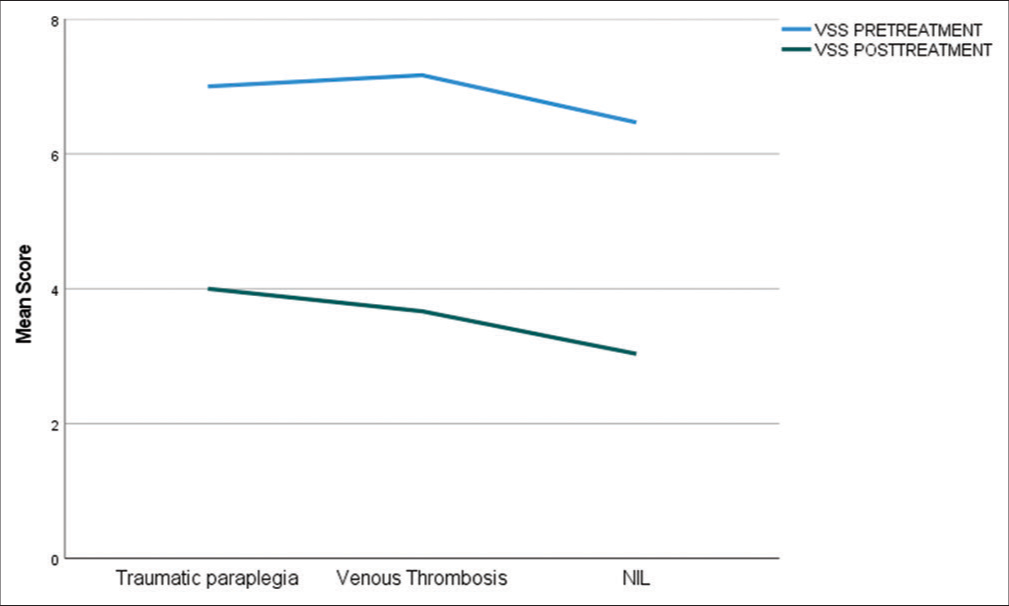
- Relation of VSS score with co-morbidities.
The mean pre-procedural total VSS score and post-procedural VSS score [Table 10 and Figure 10] were significantly different between socioeconomic status (ANOVA P = 0.050 and 0.027), respectively.
| SES | Pre- procedural VSS | P-value | Post- procedural VSS | P-value |
|---|---|---|---|---|
| Low | 6.2±1.5 | 0.050 | 2.9±0.8 | 0.027 |
| Middle | 7.2±1.6 | 3.6±0.8 | ||
| High | 7±2.3 | 3.2±1.6 |
VSS: Vancouver scar scale
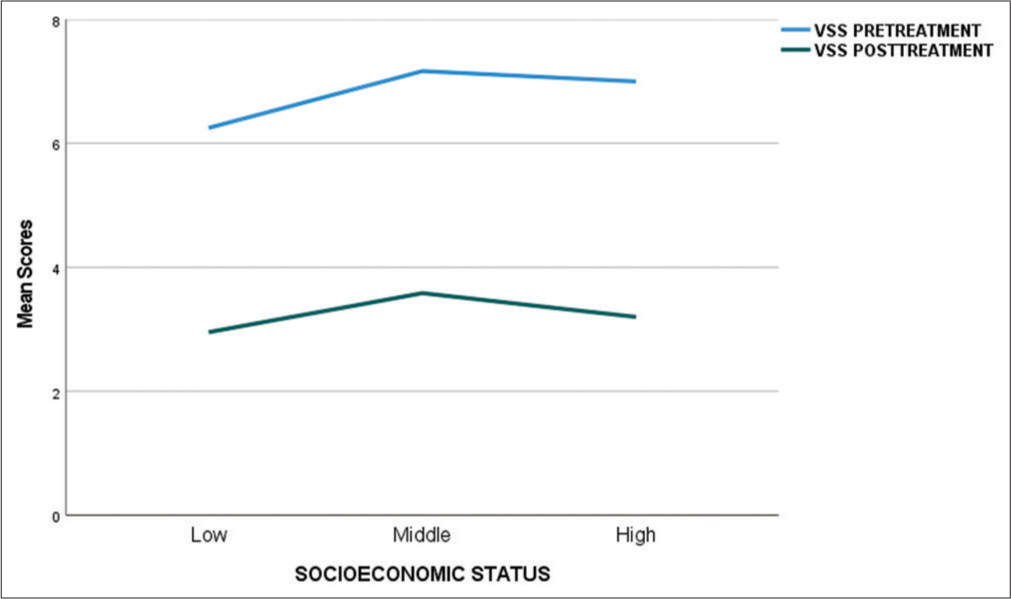
- Relation of VSS score with socio-economic status.
The degree of improvement in total VSS score after treatment is mentioned in [Table 11].
| Improvement grade | n(%) |
|---|---|
| Excellent | 38 (52.1) |
| Good | 20 (27.4) |
| Fair | 12 (16.4) |
| Poor | 3 (4.1) |
| Total | 73 (100) |
VSS: Vancouver scar scale
DISCUSSION
The present prospective interventional study investigated the efficacy and safety of ablative 2,940-nm Er: YAG laser on traumatic scars after primary repair during the post-traumatic period. The study also evaluated the effect of clinical factors on patients treated for these scars by Er: YAG laser. The clinical assessment was objectively based on clinical photography before treatment and 1 month after laser treatment by means of clinical improvement.
Our study found that there was a significant improvement (P <0.001) in vascularity, pigmentation, pliability, height, and total VSS scores at 1 month post-treatment. Independent investigator was asked to select which image represented the post-treatment image and to rate the percent improvement in the appearance of the surgical or post-traumatic scar. The scars were graded on a four-point scale (excellent, 75–100% improvement; good, 50–75% improvement; fair, 25–50% improvement; poor, 0–25% improvement; than the pre-treatment results). Our study found that the improvement was excellent in 38 (52.1%), good in 20 (27.4%), fair in 12 (16.4%), and poor in 3 (4.1%) scars, respectively.
Scars may be hypertrophic appearing as hypopigmented or erythematous raised nodules or plaques containing excessive amounts of collagen, fibrin, and proteoglycans or may atrophic; these are dermal depressions with overlying thinned epidermis resulting from a loss of dermal collagen after inflammation (post-traumatic wounds or surgery).[5,6] Superficially, scars may have only cosmetic value; however, on deeper introspect, scars seemingly impact the patient physically as well as psychologically. Physically, scars can impair range of motion, can be painful, and cause dysesthesia and pruritus.[7,8] Patients with scars causing disfigurement scars may lower patient’s self-esteem leading to psychosocial isolation.[9-11]
Various treatment modalities have been developed to improve scar appearance. Some of these also address adverse effects; these include silicone gel sheets, pressure garments, corticosteroid therapy, dermabrasion, surgical excision, chemical peels, and, more recently, laser treatments.[12,13] It is needless to say that certain laser therapies have yielded positive results, others, such as the Nd: YAG and traditional ablative lasers, have also worsened scar cosmesis.[14,15] Furthermore, traditional ablative treatments cause adverse events such as oozing, infection, and hyper-pigmentation.[16] Non-ablative fractional photothermolysis (at 1550 nm wavelength) has been found to be effective for the treatment of conditions melasma, rhytides, acne scars, surgical scars, and even poikiloderma of Civatte. However, this modality has been found to be time-consuming and is painful, and moreover, the results are sometimes unpredictable.[17,18]
Recently, ablative fractional photothermolysis using the Er: YAG laser (2940 nm) has been introduced as a novel means of providing treatment that would be as effective as traditional ablative laser while avoiding their risks. The laser produces thousands of microscopic, clinically inapparent wounds on the skin surface that is rapidly re-epithelialized by the surrounding, undamaged tissue, sparing the epidermis.[19,20]
Modena et al. conducted a review of published studies (n = 338) till 2019, to elucidate the efficacy, safety, and benefits of applying fractional lasers erbium glass and Er: YAG to different type of scars. The authors found that both lasers were effective in the short term, with minimal side effects; however, the long-term efficacy and safety had several limitations. This has paved the way for further research in this field.[21]
Kunzi-Rapp K et al. investigated an Er: YAG 2940 laser with thermal mode in 12 patients with scars including post-traumatic scars and fascial atrophic scars. Two treatments were applied 2 months apart. At 3–6 months follow-up, the authors found that scars were graded as excellent in 50%, good in 25%, fair in 25%, and no improvement in 0%. In our study, we applied four treatments 1 month apart in ablative and thermal mode. The explanation of such difference can be attributed to the use of different mode (they used thermal mode with sub-ablative fluences of 2.1 and 3.1 J/cm2) and follow-up periods (1 month vs. 3–6 months).[22] Weiss et al. investigated the efficacy of ablative fractional CO2 laser in 15 patients with post-operative and traumatic scars. Each scar received 3 ablative fractional resurfacing (AFR) treatments at 1–4 month intervals; at 6-month follow-up, scars were graded as 16% of the treated scars achieving excellent 76% or greater overall improvement and 89% of treated scars achieving 51% or greater overall improvement. In the present work, at 1-month follow-up, 52.1% of patients had excellent improvement and 27.4% had good improvement. Such difference may be explained by the fact that, we used a greater number of sessions of laser treatment (four treatment sessions at monthly interval) and Weiss et al. used different laser type (fractional CO2).[23]
Sobhy et al. conducted a study to assess the efficacy and safety of fractional Er: YAG laser for the treatment of surgical and post-traumatic scars; both clinically and histopathologically. Twenty subjects received two to five treatments at 1 month interval and a follow-up period for 3 months. The authors found that almost all patients improved both clinically and histopathologically. Clinical improvement of scars according to investigator assessment was 40% with excellent improvement, 50% with good improvement, and 10% with fair improvement at 3 month follow-up. Although the results were comparable with our study, Sobhy et al. had a greater number of sessions of laser treatment (up to five), used higher laser energy (up to 1100 mJ) and follow-up duration was longer (3 months vs. 1 month).[24]
Kim et al. assessed the efficacy and safety of ablative fractional resurfacing (AFR) for traumatic scars using a 2940-nm Er: YAG laser for traumatic scars after primary repair during the early post-traumatic period. Twelve patients with 15 scars were enrolled. All had a history of facial laceration and primary repair by suturing on the day of trauma. Laser therapy was given after 4 weeks of primary repair. Each patient received four treatment sessions at 1-month intervals with a fractional ablative 2940-nm Er: YAG laser. Patients were evaluated at 1 month after the fourth treatment session. The authors found that all treated portions of the scars showed improvements, as assessed by the VSS scores and the overall cosmesis.[25] The results were in agreement with our study.
Other studies have reported comparable results. A study by Hu et al. demonstrated the successful treatment of atrophic facial acne scars using the two modes of ablation and coagulation of fractionally delivered Er: YAG (2,940-nm) laser with acceptable downtime and minimal side effects. Another study by Chapas et al. discovered a mean 66.8% improvement in 13 patients with facial atrophic acne scarring within two to three treatment sessions.[26-29]
Our study had several limitations. The sample size was small (n = 73) leading to type II error and consequently overestimation. We acknowledge the inherent limitations related to non-randomized study design like selection bias. Controlled studies are warranted to better understand the efficacy of ablative fractional photothermolysis for the treatment and prevention of scars and to determine optimal parameters. The follow-up period was relatively small (1 month). Moreover, treated patients were not assessed histopathologically. In addition, a split-scar study to compare the effects of laser assisted and natural healing would be more informative. Finally, the patient’s satisfaction could have been assessed.
A detailed pre-procedure history and physical examination can prevent problems. Correct patient selection is crucial. Positive outcomes are also improved by patient education. Sun protection is crucial to preventing post-inflammatory pigmentation alterations. Post-procedure wound management and healing changes should be explained to patients. Infection, scars, and healing delays should be stated.[30-32]
CONCLUSION
The present study shows that ablative fractional Er: YAG laser treatment improved scars fairly well based on objective results. Even though AFR cannot be the only method for scar management, we believe that early scar treatment using AFR can be an adjuvant scar management method for improving the quality of life of patients with traumatic scars. Finally, we suggest that a long-term study with a larger number of patients in multiple centers should be conducted to compare scars treated with AFR and those that are not.
Authors’ contributions
All authors made contributions to the article.
Availability of data and materials
Yes.
Ethical approval
Approved by the Research Ethics Committee at JIPMER, Pondicherry. Institutional Ethics Committee number JIP/ IEC/2020/08, dated 25th June 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Early postoperative treatment of thyroidectomy scars using a fractional carbon dioxide laser. Dermatol Surg. 2011;37:217-23.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of surgical scars with the cryogen-cooled 595 nm pulsed dye laser starting on the day of suture removal. Dermatol Surg. 2006;32:13-20.
- [CrossRef] [Google Scholar]
- Treatment of atrophic scars with fractional photothermolysis: Short-term follow-up. J Dermatolog Treat. 2011;22:43-8.
- [CrossRef] [PubMed] [Google Scholar]
- The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33:295-9.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer's skin tension lines. Plast Reconstr Surg. 2005;116:1648-56.
- [CrossRef] [PubMed] [Google Scholar]
- Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;2013:CD003826.
- [CrossRef] [Google Scholar]
- Psychopathology and psychological problems in patients with burn scars: Epidemiology and management. Am J Clin Dermatol. 2003;4:245-72.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006;297:433-8.
- [CrossRef] [PubMed] [Google Scholar]
- Silicones in the rehabilitation of burns: A review and overview. Burns. 2001;27:205-14.
- [CrossRef] [PubMed] [Google Scholar]
- Laser treatment of hypertrophic scars, keloids, and striae. Dermatol Clin. 1997;15:419-29.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical management of hypertrophic scars: Evidence-based therapies, standard practices, and emerging methods. Aesthetic Plast Surg. 2007;31:468-92.
- [CrossRef] [PubMed] [Google Scholar]
- The short-and long-term side effects of carbon dioxide laser resurfacing. Dermatol Surg. 1997;23:519-25.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998;24:315-20.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical trial of a laser device called fractional photothermolysis system for acne scars. J Dermatol. 2006;33:623-7.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional photothermolysis for the treatment of surgical scars: A case report. J Cosmet Laser Ther. 2006;8:35-8.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:96-107.
- [CrossRef] [Google Scholar]
- Novel use of erbium: YAG (2940-nm) lasers for fractional ablative photothermolysis in the treatment of photodamaged fascial skin: A pilot study. Dermatol Surg. 2008;34:1023-53.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy, safety, and guidelines of application of the fractional ablative laser erbium YAG 2940 nm and non-ablative laser erbium glass in rejuvenation, skin spots, and acne in different skin phototypes: A systematic review. Lasers Med Sci. 2020;35:1877-88.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive skin rejuvenation with erbium: YAG laser used in thermal mode. Lasers Surg Med. 2006;38:899-907.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: Quantitative volumetric scar improvement. Arch Dermatol. 2010;146:133-40.
- [CrossRef] [PubMed] [Google Scholar]
- Study of fractional ablative laser in surgical and post traumatic scar. Our Dermatol Online. 2012;3:188-95.
- [CrossRef] [Google Scholar]
- The efficacy and safety of ablative fractional resurfacing using a 2,940-Nm Er: YAG laser for traumatic scars in the early posttraumatic period. Arch Plast Surg. 2012;39:232-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg. 2011;37:939-44.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40:381-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of post-burn scars of the face by Er: YAG laser. Egypt J Plast Reconstr Surg. 2019;43:85-92.
- [CrossRef] [Google Scholar]
- Laser erbium-YAG resurfacing In: Statpearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- Complications and post-treatment care following invasive laser skin resurfacing: A review. J Cosmet Laser Ther. 2018;20:168-78.
- [CrossRef] [PubMed] [Google Scholar]
- Laser fitzpatrick skin type recommendations In: Statpearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- Keys to building a safe and effective healthcare laser program. Laser Ther. 2018;27:11-20.
- [CrossRef] [PubMed] [Google Scholar]






