Translate this page into:
Disseminated Kaposi’s sarcoma as the sole clinical manifestation in an intravenous drug abuse patient with acquired immunodeficiency syndrome

*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government Medical College, Trivandrum, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Swarnalekshmy TP, Nair PS, Viswanath V. Disseminated Kaposi’s sarcoma as the sole clinical manifestation in an intravenous drug abuse patient with acquired immunodeficiency syndrome. CosmoDerma 2023;3:106.
Abstract
A 31-year-old married acquired immunodeficiency syndrome (AIDS) male patient with clonal differentiation 4 count of 162 cells/mm3 and history of intravenous drug abuse presented with multiple discrete hyperpigmented and violaceus papules and plaques distributed on the trunk, upper and lower extremeties, medial canthi of the right eye, and the glans penis. He had also generalized lymphadenopathy. Biopsy of the papules and lymph node showed features of Kaposi’s sarcoma (KS). There were no other systemic or cutaneous manifestations. We are reporting an interesting case of AIDS acquired through I/V drug abuse and presenting only with dessiminated KS and no other features.
Keywords
Acquired immunodeficiency syndrome
Kaposi’s sarcoma
Intravenous drug abuse
INTRODUCTION
Acquired immunodeficiency syndrome (AIDS) is the stage 4 human immunodeficiency virus (HIV) disease where the clonal differentiation 4 (CD4) cell counts is <200 cells/mm3 and the patient presents with clinical signs and symptoms of severe immunosuppression. At present, AIDS patients are seldom encountered due to early diagnosis of HIV infection and initiating antiretroviral therapy (ART) soon after diagnosis. AIDS patients usually present with systemic features such as cryptococcal meningitis, tuberculosis, cryptosporoidal diarrohea, and AIDS-associated malignancies like Kaposi’s sarcoma (KS).[1] Herein, we are reporting an AIDS patient acquired due to intravenous drug abuse and presenting only with dessiminated KS and no other clinical features.
CASE REPORT
A 31-year-old married male IT professional presented with hyperpigmented lesions of 5 months duration. The lesions first started on the left calf as erythematous macules which later evolved into violaceous papules and plaques involving the trunk and upper and lower extremeties. Recently, the patient also noticed erythematous lesions on the right eye and glans penis.The patient did not give history of genital ulcers, discharge, or blood transfusion. Past history was non-contributory. There as no history of cough, weight loss or frequent diarrohea, or any other clinical features of severe systemic disease. The patient denied pre-marital (PMC) or extramarital contacts (EMC). On careful history taking, it was noted that he had a habit of intravenous drug abuse with his peers 4 years ago and had shared needles.
On examination, the patient had multiple well-defined discrete hyperpigmented and violaceus papules and plaques distributed on the trunk, upper and lower extremeties [Figure 1a and b]. The patient also had an erythematous papule on the medial canthi of the right eye and a violaceous plaque on the glans penis extending from the 4’O clock to 6’O clock position [Figure 2a and b]. There was no other cutaneous manifestation. The patient had bilateral multiple discrete non-tender, non-matted enlarged cervical, supraclavicular, axillary, and inguinal lymph nodes, the largest (right axilla) measuring 3 × 2 cm. The weight was 42 kg. There was no hepatosplenomegaly and the cardiovascular system, central nervous system, respiratory, and musculoskeletal systems were normal.

- Multiple well-defined hyperpigmented and violaceous papules and plaques on trunk and extremeties.
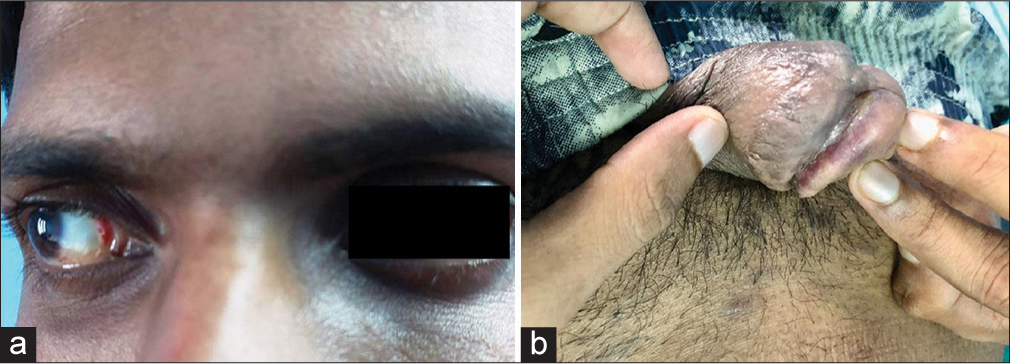
- (a) Erythematous papules on medial canthi and (b) violaceous plaque on glans penis.
The patient’s hemogram, liver, and renal function tests were normal. Serological test for syphilis and hepatitis B and C was negative. Tridot test for HIV was positive and the CD4 count was 162 cells/mm3. The patients wife was HIV negative. Chest X-ray showed hilar lymphadenopathy, but no evidence of tuberculosis (TB). Sputum, catridge-based nucleic acid amplication test was negative. Ultrasound abdomen showed mild hepatospenomegaly and Grade 3 fatty liver. Computed tomography scan of chest, abdomen, and pelvis showed cervical, mediastinal, axillary, intra-abdominal, and inguinal lymphadenopathy. Skin biopsy taken from a plaque on the trunk showed the entire dermis packed with vascular spaces and interwining spindle-shaped cells [Figure 3a], while high power showed numerous vascular spaces containing red bllod cells and atypical plump endothelial cells [Figure 3b]. Immunohistochemistry (IHC) was positive for CD34 [Figure 4], suggestive of KS. Deoxyribonucleic acid polymerase chain reaction for human herpes virus-8 (HHV-8) could not be done due to non-availability. Lymph node biopsy also showed effacement of the architexture by collections of vascular spaces lined by atypical plump endothelium surrounded by spindle shaped cells suggestive of KS, with no features of TB [Figure 5a and b]. The patient was started on ART (Dolutegravir 50 mg, Lamivudine 300 mg, and Tenofovir 300 mg), and in the oncology department, he was started on liposomal doxorubicin. The papules, plaques, and the lesion on the right eye and glans penis showed reduction in size during last follow-up. Further, follow-up could not be done as the patient was lost to follow-up and on enquiry, it was noted that he has not attended the ART clinic for collecting the drugs.
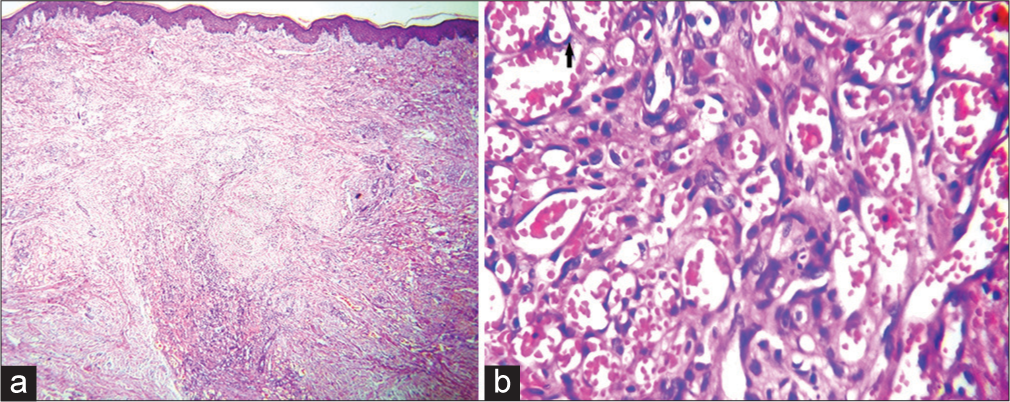
- (a) Skin biopsy showing the dermis packed with vascular spaces and spindle cells, H & E ×100 and (b) high power showing the vascular spaces with plumb atypical endothelial cells (arrow) and filled with red blood cells, H & E, ×400.
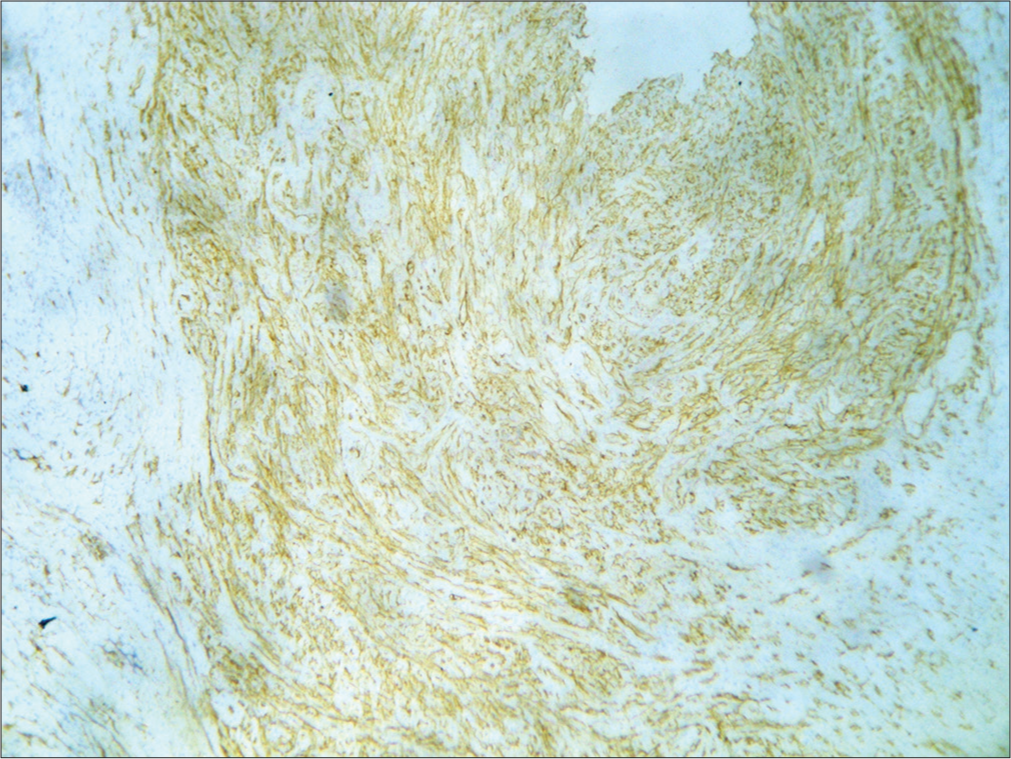
- Immunohistochemistry (IHC) showing vascular spaces staining positive for CD34, IHC stain ×400.
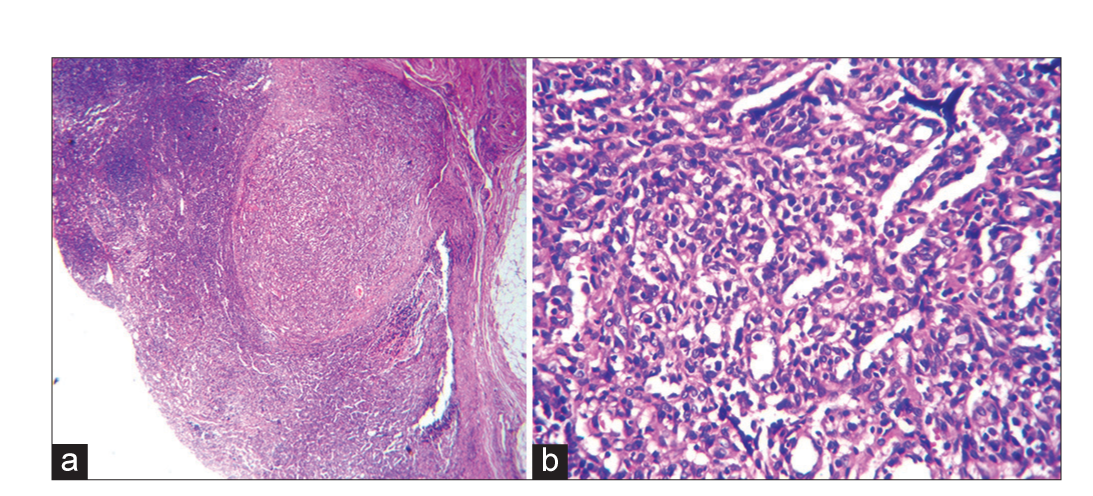
- (a) Lymph node biopsy showing architexture effaced by multiple vascular spaces, H & E, 100, high power showing and (b) high power showing vascular spaces with plump endothelial cell, H & E, ×400.
DISCUSSION
Our patient gave history of multiple intravenous drug abuse with sharing of needles, while denying PMC and EMC. He was retro positive with a CD4 count of 162 cells/mm3. The patient presented with multiple discrete hyperpigmented violaceous papules and plaques on the trunk, extremeties, eyes, and glans penis with histopathology and IHC diagnostic of KS. Lymph node biopsy also showed features of KS. There were no other cutaneous or systemic features of AIDS. Therefore, we made a diagnosis of AIDS acquired by I/V drug abuse and disseminated KS as the skin, mucosa, and lymph nodes were affected. AIDS presenting with only KS is rare though reported in the literature.[2] The other highlight of this case is that investigations did not reveal any other systemic involvement in spite of the patient having AIDS and low CD4 counts. The patient did not have any cutaneous manifestations, other than KS, which is again unusual in a case of AIDS. KS is now considered to be caused by HHV-8, along with coinfection with HIV virus.[3] HHV-8 is usually acquired through sexual route, but, in our patient, the only risk factor was I/V drug abuse and not PMC or EMC, this being another highlight of this case, also indicating that HHV-8 can be transmitted through needle sharing.[4,5] KS is a multicentric malignant proliferation of the endothelium initiated by HHV-8/HIV coinfection involving primarly the skin and mucosa of the oral cavity, eyes, and genitals and an AIDS defining condition. Common site of dessimination is to the lymph nodes which lead to lymphedema. The other organs involved are the small intestine causing massive hemorrage, the lungs, heart, and liver. The skin lesions are classified into patch, plaque, and tumor stage. Histopathology is classical with the entire dermis packed with slit such as vascular spaces lined by atypical plump endothelium and the vascular spaces are surrounded by spindle cells, hence the term sarcoma. Extension of these vascular structure into normal vasculature is known as “promontory sign.”[6] There may also be extravasated RBCs and a sparse mononuclear infiltrate. Dermoscopy shows bluish-red color, scaly surface, and brown globules, while polarizing dermoscope shows variable colors known as “rainbow pattern.”[7]
Localized lesions respond to radiotherapy.[8] Alitretinoin, a retinoid X receptor binding retinoid, showed efficacy in localized lesions of KS.[9] ART by itself reduces the size of the lesions. Dessiminated lesions require chemotherapy, with best response to pegylated liposomal doxorubicin, which was given to our patient. The other agents are vinca alkaloids, etoposide, paclitaxel, and interferon alpha.
CONCLUSION
KS is rare in India with few case reports. We are reporting an AIDS patient acquired due to intravenous drug abuse and presenting only with dessiminated KS and no other clinical features – an interesting and rare presentation and also that HHV-8 can be transmitted through needle sharing also in addition to sexual contact.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Clinical characteristics, predictors of immune reconstitution inflammatory syndrome and long-term prognosis in patients with Kaposi sarcoma. AIDS Res Ther. 2017;14:30.
- [CrossRef] [PubMed] [Google Scholar]
- Kaposi's sarcoma as a presenting manifestation of HIV. Indian J Sex Transm Dis AIDS. 2011;32:108-10.
- [CrossRef] [PubMed] [Google Scholar]
- Kaposi's sarcoma: An interesting case report in a human immunodeficiency virus-positive heterosexual male. Indian J Sex Transm Dis AIDS. 2022;43:179-81.
- [CrossRef] [PubMed] [Google Scholar]
- Recapitulation of acquired immuno deficiency syndrome associated Kaposi's sarcoma. Indian J Sex Transm Dis AIDS. 2016;37:11522.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated violaceous plaques in a HIV-1-positive patient from Eastern India: A manifestation of Kaposi's sarcoma. Indian J Sex Transm Dis AIDS. 2021;42:69-72.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated Kaposi's sarcoma in a human immunodeficiency virus-infected homosexual Indian man. Indian J Dermatol Venereol Leprol. 2017;83:78-83.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated Kaposi's sarcoma as a presenting sign of HIV in an Indian male: A case report with dermoscopic findings. Indian J Sex Transm Dis AIDS. 2020;41:102-5.
- [CrossRef] [PubMed] [Google Scholar]
- Radiotherapy in the management of Kaposi's sarcoma: Comparison of 8 Gy versus 6 Gy. J Natl Med Assoc. 2006;98:1136-9.
- [Google Scholar]
- Topical treatment of cutaneous lesions of acquired immunodeficiency syndrome-related Kaposi sarcoma using alitretinoin gel: Results of phase 1 and 2 trials. Arch Dermatol. 2000;136:1461-9.
- [CrossRef] [PubMed] [Google Scholar]






