Translate this page into:
Dermoscopy of nevus sebaceous

*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, Maulana Azad Medical College, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Dev T, Thakur SS, Guglani A. Dermoscopy of nevus sebaceous. CosmoDerma. 2024;4:82. doi: 10.25259/CSDM_94_2024
A 14-year-old female presented to the dermatology outpatient with a persistent lesion on the scalp, since birth. The lesion had become more pronounced and slightly elevated over the past year. There was no history of pain, itching, or discharge from the lesion. The patient had no significant medical history or family history of similar lesions. On examination, a well-demarcated, yellowish, verrucous plaque measuring 3 cm in diameter was noted on the vertex of the scalp [Figure 1]. The surface appeared waxy and slightly raised without ulceration or signs of inflammation. Dermoscopy revealed a uniform yellow background corresponding to the sebaceous components of the lesion, a convoluted, cerebriform pattern indicative of epidermal hyperplasia, and multiple comedo-like openings scattered across the lesion [Figure 2]. Histopathological examination revealed papillomatosis and acanthosis of the epidermis along with follicular plugs. Multiple sebaceous lobules were noted adjacent to the epidermis in the superficial and mid-dermis [Figure 3]. These clinical, dermoscopic, and histologic features were consistent with the diagnosis of nevus sebaceous. The patient as well as her parents were counseled about the benign nature of the lesion and the possible treatment options. Given the absence of any secondary neoplastic changes in this case, a conservative approach with regular monitoring was adopted.

- A well-demarcated, yellowish, verrucous plaque on the vertex of the scalp.
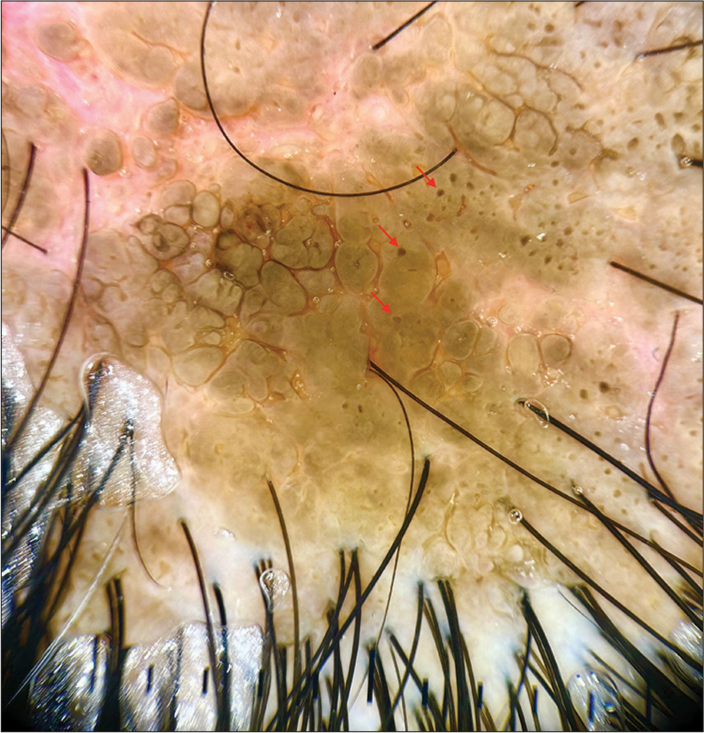
- Dermoscopy showing a uniform yellow background corresponding to the sebaceous components of the lesion, a convoluted, cerebriform pattern indicative of epidermal hyperplasia, and multiple comedo-like openings (red arrows) scattered across the lesion (polarized, ×20).
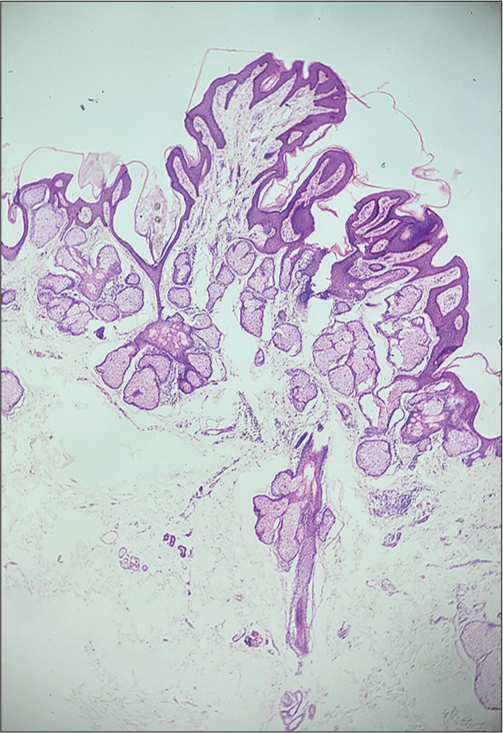
- Histologic section showing papillomatosis and acanthosis of the epidermis along with follicular plugs. Multiple sebaceous lobules are noted adjacent to the epidermis in the superficial and mid-dermis (H and E; ×40).
Nevus sebaceous is a hamartoma comprising sebaceous glands, hair follicles, and epidermal elements. It typically presents at birth or in early childhood as a solitary papule, or a linear, or oval plaque on the scalp or face. It is characterized by a yellowish, verrucous plaque that may change during puberty due to hormonal influences. The primary concern is the potential for secondary neoplastic transformations, particularly during or after puberty. These may include benign tumors such as trichoblastoma or syringocystadenoma papilliferum, and rarely, malignant tumors such as basal cell carcinoma.[1] Regular monitoring and dermoscopic evaluation are essential for early detection of these changes, assisting in diagnosis and monitoring. Surgical excision may be considered, especially if there are signs of neoplastic transformation or for cosmetic reasons.[1,2]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Sebaceous nevus of Jadassohn: Review and clinical-surgical approach. An Bras Dermatol. 2022;97:628-36.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic analysis of nevus sebaceus of Jadassohn: A study of 13 cases. Skin Appendage Disord. 2017;3:83-91.
- [CrossRef] [PubMed] [Google Scholar]






