Translate this page into:
Dermoscopy of dermatitis cruris pustulosa et atrophicans

*Corresponding author: Arun Somasundaram, Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. arunsomasundaram25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Somasundaram A. Dermoscopy of dermatitis cruris pustulosa et atrophicans. CosmoDerma 2023;3:166. doi: 10.25259/CSDM_219_2023
A 35-year-old male consulted the outpatient department for itchy pustular skin lesions over bilateral lower legs for 1 year. He gave a history of application of coconut oil regularly for his lower legs and forearm for the past 5 years. There were no drugs before the onset of skin lesions and had no known comorbidities. Cutaneous examination revealed multiple symmetrically distributed follicular pustules leaving behind surrounding exfoliation, atrophy, and loss of hair over both lower legs [Figure 1]. Dermoscopy (DermLite, ×10, polarized mode) showed a folliculocentric pustule with surrounding erythema [Figure 2a], white scaling around the follicle, and coiled hairs [Figure 2b]. Based on clinical findings, dermatitis cruris pustulosa et atrophicans (DCPA) was considered. Culture was sent from the pustule which grew Staphylococcus aureus that was sensitive to oxacillin and tetracyclines. The patient was initiated on oral doxycycline 100 mg twice a day along with mupirocin ointment thrice a day for 2 weeks and to follow up.

- Multiple symmetrically distributed follicular pustules leaving behind surrounding exfoliation, atrophy, and loss of hair over both lower legs.
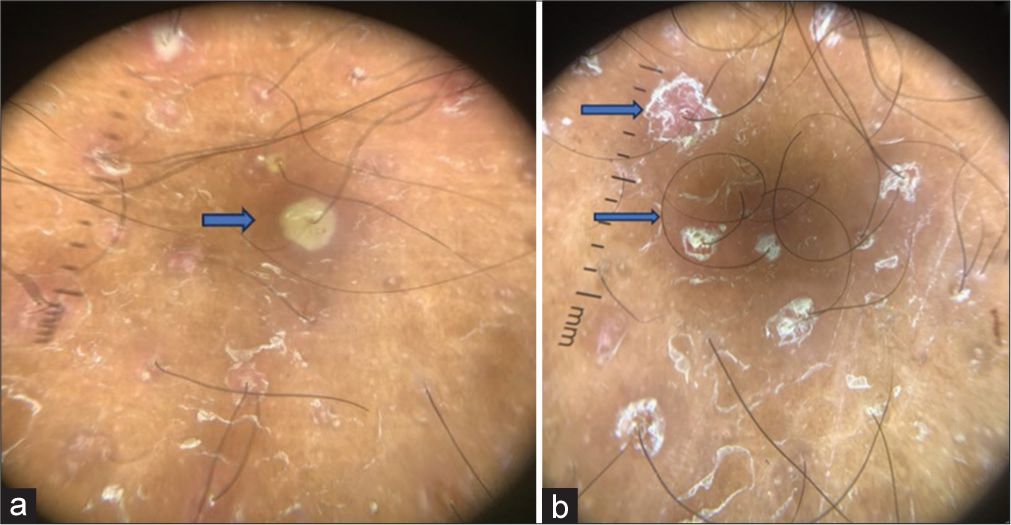
- (a) Dermoscopy (DermLite, ×10, polarized mode) showed a folliculocentric pustule with surrounding erythema, (b) White scaling around the follicle and coiled hairs evident in dermoscopy.
DCPA is a chronic superficial folliculitis with unknown etiology. S. aureus is thought to be one of the prime causative agents.[1] It is usually symmetrical, involving bilateral legs. Rarely, other sites such as the upper limb, beard, and axilla can also be involved. Triggering factors include climate, occlusion, and clothing.[2,3] Occlusion may be one of the triggers that our patient would have had. Dermoscopy findings of this superficial folliculitis DCPA have not been reported in the literature to the best of our knowledge except for anecdotal reports on viral and pityrosporum folliculitis. Our case highlights the features of superficial folliculitis which would add a piece of supportive evidence for the diagnosis as a non-invasive modality and to manage accordingly.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermatitis cruris pustulosa et atrophicans. Indian J Dermatol Venereol Leprol. 2009;75:348-55.
- [CrossRef] [Google Scholar]
- Dermatitis cruris pustulosa et atrophicans revisited: Our experience with 37 patients in south India. Int J Dermatol. 2009;48:1082-90.
- [CrossRef] [Google Scholar]
- Dermatitis cruris pustulosa et atrophicans: Scarring alopecia beyond scalp hair. Skin Appendage Disord. 2022;8:280-6.
- [CrossRef] [Google Scholar]





