Translate this page into:
Dermoscopy of Becker’s nevus in two cases

*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, Maulana Azad Medical College, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Bahadur A, Tyagi H, Dev T, Yadav D, Barman KD. Dermoscopy of Becker’s nevus in two cases. CosmoDerma. 2024;4:103. doi: 10.25259/CSDM_108_2024
Dear Sir,
Becker’s nevus (BN) is a benign cutaneous hamartoma characterized by hyperpigmented, often hairy patches predominantly affecting young males.[1] Dermoscopy enhances the clinical assessment by revealing specific features of the nevus.[2] We report the clinical features, dermoscopic findings, histological characteristics, and dermoscopic-histopathologic correlation of two cases of BN.
Case 1: A 21-year-old male presented with a well-demarcated, hyperpigmented patch on his left arm, which he first noticed at age 18. The lesion measured approximately 15 × 8 cm and displayed increased hair growth [Figure 1a]. Dermoscopy revealed an irregular pigment network (brown reticular lines) and focal and skin furrow hypopigmentation. Perifollicular hypopigmentation and increased terminal hairs were also noted [Figure 1b]. Histological examination showed hyperkeratosis, basal layer melanization, and acanthosis with elongated, flattened, and fused rete ridges. Follicular hyperkeratotic plugs and sparse smooth muscle hyperplasia were observed [Figure 1c].
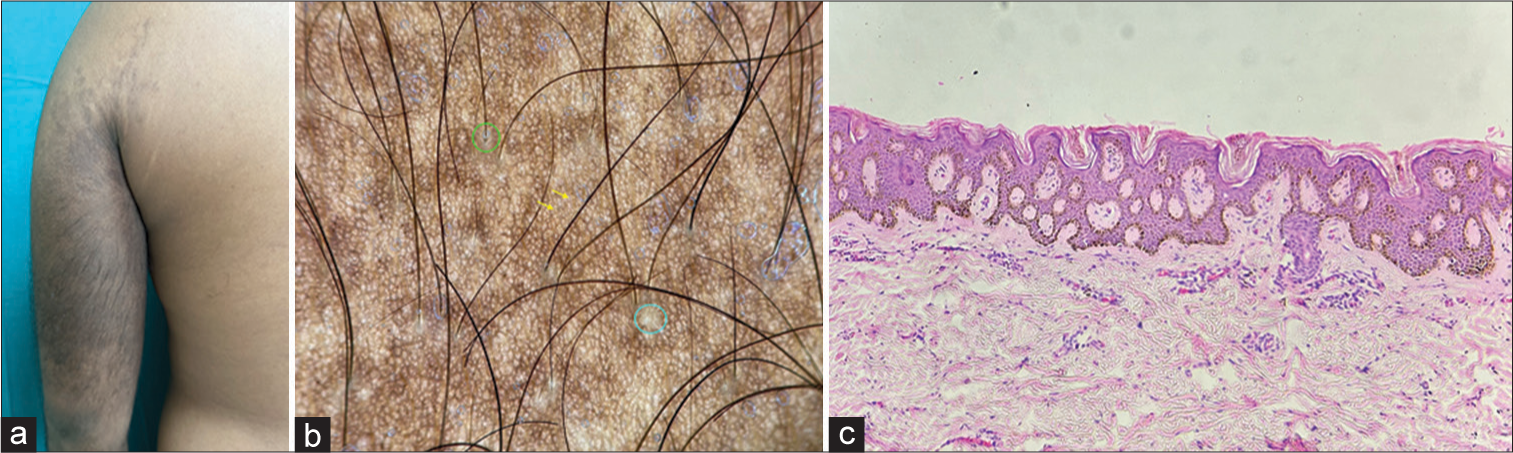
- (a) Well-demarcated, hyperpigmented, and hypertrichotic patch on the left arm; (b) polarized dermoscopy showing irregular pigment network (brown reticular lines), focal (blue circle) and skin furrow hypopigmentation (yellow arrow), perifollicular hypopigmentation (green circles), and increased terminal hairs (×20); (c) histological section showing hyperkeratosis, basal layer melanization, and acanthosis with elongated, flattened, and fused rete ridges along with follicular hyperkeratotic plugs (Hematoxylin and eosin; ×100).
Case 2: A 17-year-old female presented with a progressively enlarging hyperpigmented patch on her left leg, first noticed at age 15. The lesion measured approximately 10 × 7 cm with hypertrichosis [Figure 2a]. Dermoscopy revealed an irregular and coarser pigment network compared to the surrounding skin. Skin furrow and focal hypopigmentation were also evident along with perifollicular hypopigmentation and hypertrichosis [Figure 2b]. Histological examination demonstrated basal layer melanization and smooth muscle hyperplasia [Figure 2c].
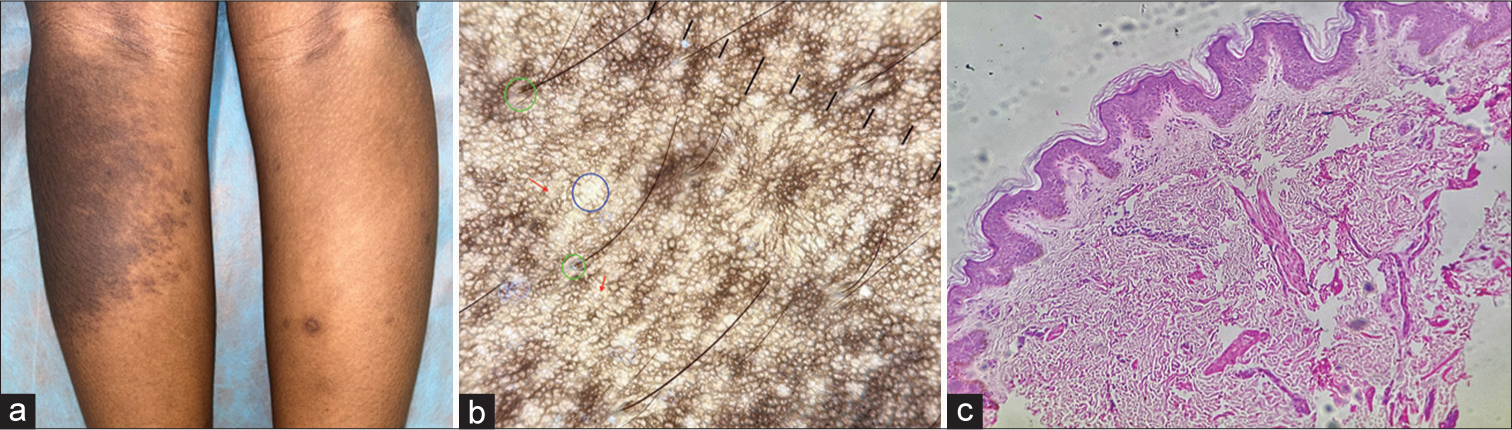
- (a) Well-demarcated, hyperpigmented, and hypertrichotic patch on the left leg; (b) polarized dermoscopy showing an irregular and coarser pigment network, skin furrow (red arrows), focal hypopigmentation (blue circle), and perifollicular hypopigmentation (green circles) (×20); and (c) histological section showing basal layer melanization and smooth muscle hyperplasia (Hematoxylin and eosin; ×100).
BN can present with varying clinical features, including congenital onset, bilateral distribution, and occurrence on unusual sites such as the face.[3] An uncommon follicular variant has also been reported.[4] It typically appears during the first or second decade of life, although there have been instances of congenital cases. The condition is more commonly diagnosed in males, likely because females often exhibit milder pigmentation and less noticeable hypertrichosis, which is influenced by androgen levels.[5] BN syndrome is a rare condition characterized by the presence of BN associated with other anomalies, such as ipsilateral hypoplasia of the breast or other musculoskeletal anomalies including scoliosis, spina bifida, and limb hypoplasia.[1] It underscores the importance of a comprehensive assessment for associated abnormalities in patients with BN. The etiopathogenesis of BN is not completely understood. It is believed to result from androgen receptor hypersensitivity, explaining the male predominance and association with hypertrichosis. Hormonal factors may play a role, particularly in lesions that appear or become more prominent during puberty. The development of BN is believed to involve increased androgen receptor expression in the affected skin. Elevated mRNA and protein levels of estrogen receptors alpha and beta in the hair follicles of lesional skin have been documented within BN. Progesterone receptor immunostaining was also higher in hair follicles than in sebaceous glands, indicating a folliculocentric pattern. Recurrent actin-beta (ACTB) gene mutations have been demonstrated within arrector pili muscles. The ACTB gene, coding for beta-actin, is crucial for cell functions such as migration and proliferation. Previous ACTB mutations have been linked to developmental syndromes and musculoskeletal abnormalities. These findings suggest that ACTB mutations in BN might enhance Hedgehog signaling, affecting hair follicles and pilar muscles. Further, research is necessary to understand the pathways influenced by these mutations.[6]
The dermoscopic features of BN, including an irregular pigment network, correlate well with histological findings of basal layer melanization. The presence of perifollicular hypopigmentation on dermoscopy corresponded to follicular hyperkeratotic plugs observed histologically.[7]
Smooth muscle hamartoma can resemble a BN. Both conditions can present as pigmented plaques with hypertrichosis and display acanthosis, basal layer hyperpigmentation, and dermal smooth muscle proliferation on histology. However, BN usually appears during puberty, whereas SMH is present at birth or early infancy. BN typically shows increasing pigmentation and hypertrichosis over time, unlike SMH. Dermoscopy of SMH often reveals prominent follicular openings with numerous vellus hairs on a background of normal to increased pigmentation. Histologically, BN shows more pronounced epidermal changes and variable dermal smooth muscle, while SMH features well-defined, thickened smooth muscle fibers randomly arranged in the reticular dermis, sometimes encircling or connecting to hair follicles, with narrow spaces between muscle bundles and adjacent collagen. The significant overlap between BN and SMH has sparked discussions about whether they are distinct entities or different manifestations of a spectrum.[8] Other differential diagnoses of BN include congenital melanocytic nevus, Café-au-lait spot, and nevus spilus (speckled lentiginous nevus) [Table 1].
| Feature | Becker’s nevus | Congenital melanocytic nevus | Café-au-lait spot | Nevus spilus (speckled lentiginous nevus) |
|---|---|---|---|---|
| Onset | Adolescence | Birth or early childhood | Birth or early childhood | Birth or early childhood |
| Appearance | Hyperpigmented patch with increased hair | Hyperpigmented patch or nodule, often hairy | Light brown, uniform pigmentation | Light brown macule with darker macules/papules |
| Hair Growth | Commonly present | Often present | Absent | Absent |
| Pigmentation | Brown to black | Brown to black | Light brown | Light brown background with darker spots |
| Borders | Irregular but well-defined | Well-defined, can be irregular | Well-defined | Well-defined |
| Size | Variable, can enlarge over time | Variable, can be large | Usually small to medium | Variable |
| Texture | Smooth | Can be smooth or nodular | Smooth | Smooth with speckled appearance |
| Dermoscopic Features | Reticular or globular pattern, homogeneous pigmentation | Globular or cobblestone pattern, homogeneous pigmentation | Featureless light brown, no specific structures | Uniform light brown with globular/reticular pattern in darker areas |
| Associated Conditions | None | Rarely can be associated with neurocutaneous melanosis if large | Can be associated with neurofibromatosis if multiple | None |
| Growth Pattern | Enlarges and darkens with age | Proportional growth with the child | Stable, does not grow | Stable, does not grow |
| Histology | Hyperkeratosis, acanthosis, basal layer hyperpigmentation, increased dermal melanocytes | Increased number of melanocytes in epidermis and dermis, nests of nevus cells | Increased melanin in basal layer, normal number of melanocytes | Increased number of melanocytes in basal layer, lentiginous proliferation of melanocytes |
After their initial appearance, BN lesions typically darken and expand over a period of about two years, resulting in a light tan to dark brown color that can be cosmetically troubling for patients. Various treatments have been explored, but none have proven consistently effective in treating BN hyperpigmentation. Treatment options include laser therapy to reduce pigmentation and hair growth. Laser treatments and topical therapies offer only temporary reduction in pigmentation without complete removal. Surgical excision is usually not recommended due to the large size of lesions and the risk of scarring. Camouflage makeup is often used when conventional treatments fail. Studies on laser treatments indicate that BN hyperpigmentation is highly resistant and prone to recurrence, presenting significant challenges for both patients and physicians. Earlier studies often suffer from small sample sizes and lack data on the safety of laser treatments for patients with darker skin. The fractional Erbium: Yttrium aluminum garnet (YAG) (2940 nm) laser has shown superior results in treating BN hyperpigmentation compared to the Q-switched neodymium-doped: YAG (1064 nm) laser, with the former being safer and having no reported side effects.[9]
Dermoscopy and histology are invaluable tools in the diagnosis of BN, providing detailed visualization and correlation of clinical features. Understanding the variants, potential syndromic associations, and the underlying etiopathogenesis aids in the comprehensive management of BN. While treatment is primarily cosmetic, the prognosis remains excellent, with BN posing no significant health risks.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Becker's melanosis: Associated abnormalities. J Am Acad Dermatol. 1983;9:509-14.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of congenital melanocytic nevus and Becker nevus in an adult male population: An analysis with a 10-fold magnification. Dermatology. 2006;212:354-60.
- [CrossRef] [PubMed] [Google Scholar]
- Becker's melanosis: A report of 12 cases with atypical presentation. Int J Dermatol. 2005;44:20-4.
- [CrossRef] [PubMed] [Google Scholar]
- Follicular Becker's nevi: A case series and review of literature. Pediatr Dermatol 2024
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrichosis is not so prevalent in Becker's nevus: Analysis of 47 cases. ISRN Dermatol. 2014;2014:953747.
- [CrossRef] [PubMed] [Google Scholar]
- Postzygotic mutations in beta-actin are associated with Becker's nevus and Becker's nevus syndrome. J Invest Dermatol. 2017;137:1795-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicohistopathological and dermoscopic features of Becker nevus: An analytical observational study from southwestern India. Pigment Int. 2023;10:24-9.
- [CrossRef] [Google Scholar]
- Clinicopathologic discordance: Congenital smooth muscle hamartoma clinically mimics reticulated vascular lesion. JAAD Case Rep. 2022;26:9-12.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating the roles of different types of laser therapy in Becker's nevus treatment. J Clin Med. 2022;11:4230.
- [CrossRef] [PubMed] [Google Scholar]






