Translate this page into:
Dermoscopic colocalization of vitiligo vulgaris and chronic plaque psoriasis

*Corresponding author: Prateek Sharma, Department of Dermatology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. prateeiik@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma P, Bansal S, Chanana C, Sharma S. Dermoscopic colocalization of vitiligo vulgaris and chronic plaque psoriasis. CosmoDerma 2022;2:44.
Dear Sir,
Chronic plaque psoriasis is an inflammatory disorder occurring due to complex interaction of genetic and environmental factors leading to immune-related cytokine dysregulation causing abnormal epidermal proliferation while vitiligo is an autoimmune disorder where destruction of epidermal melanocytes causes macular depigmentation.
Despite being previously documented in the literature, colocalization of vitiligo and psoriasis is still a rare occurrence. Several research has looked into a common underlying etiology, but have mainly attributed their coexistence to coincidence.
We present a patient with colocalized psoriasis and vitiligo with not only clinical and histological overlap but also a dermoscopic overlap, which has never been documented before, to our knowledge.
A 60-year-old female with a long-standing history of stable vitiligo vulgaris presented with multiple, itchy, scaly, and raised red lesions mostly localized to patches of vitiligo on her trunk, elbow, and neck, for the last 4-5 years. She had a family history of vitiligo with no comorbid medical or surgical conditions.
On examination, multiple scaly erythematous indurated plaques of varying sizes were colocalized with patches of vitiligo over her lower back [Figure 1a and 1b], elbow and nape of the neck, and also present separately over her mid to lower back. Examination of mucosa, nails, and joints was normal.
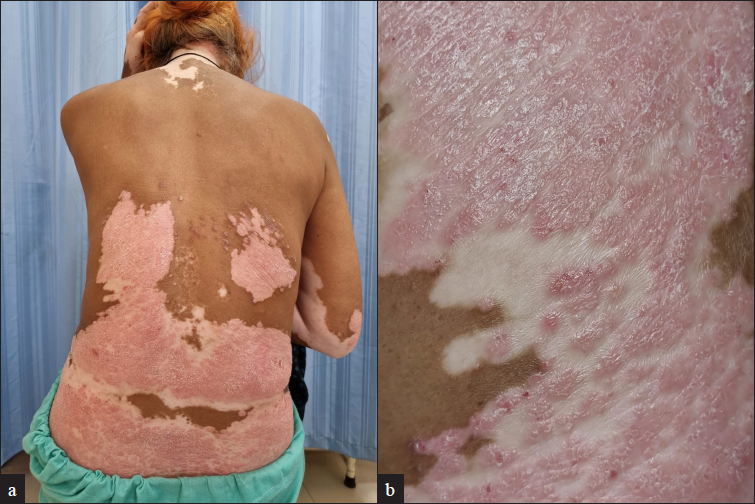
- (a) Multiple scaly erythematous indurated plaques of varying sizes colocalised with patches of vitiligo over lower back, elbow and nape of the neck and also present separately over mid to lower back; (b) Multiple scaly erythematous indurated plaques of colocalised with patches of vitiligo over lower back (close up view)
Dermoscopy revealed the homogenous distribution of red dotted and glomerular vessels against a pink background and white scales along with white structureless areas showing loss of pigment network with trichrome border and amoeboid borders at a few places [Figure 2a and 2b].
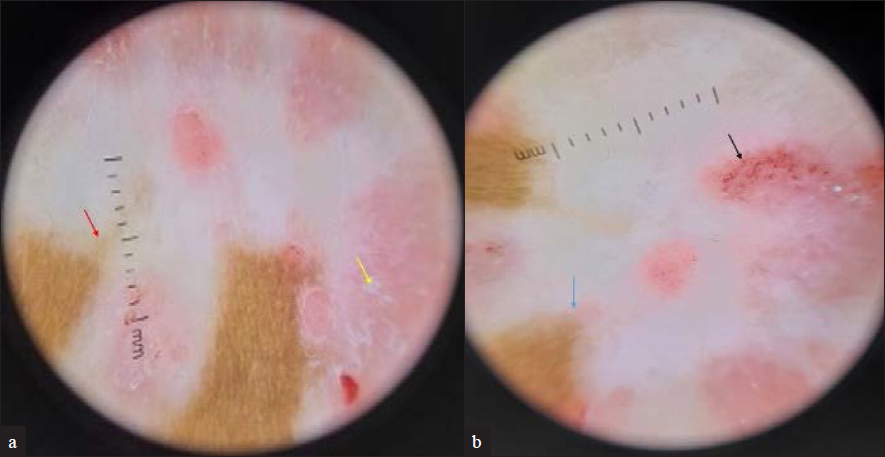
- (a) Dermoscopy shows white structureless areas with loss of pigment network and trichrome border (shown by red arrow) suggestive of vitiligo and white scales (shown by yellow arrow) suggestive of psoriasis (Dermlite DL4 4th generation ×10, polarised, contact mode); (b) Dermoscopy shows amoeboid pattern of border (shown by blue arrow) suggestive of vitiligo. and red dotted and glomerular vessels against a pink background (shown by black arrow) suggestive of psoriasis (Dermlite DL4 4th generation ×10, polarised, contact mode)
A biopsy revealed orthokeratosis, confluent parakeratosis with neutrophilic collections in stratum corneum and spinosum, psoriasiform hyperplasia, dilated blood vessels, suprapapillary thinning, and perivascular lymphohistiocytic infiltrate in upper dermis on H&E staining [Figure 3a], along with loss of melanocytes using special stain; Masson Fontana [Figure 3b].
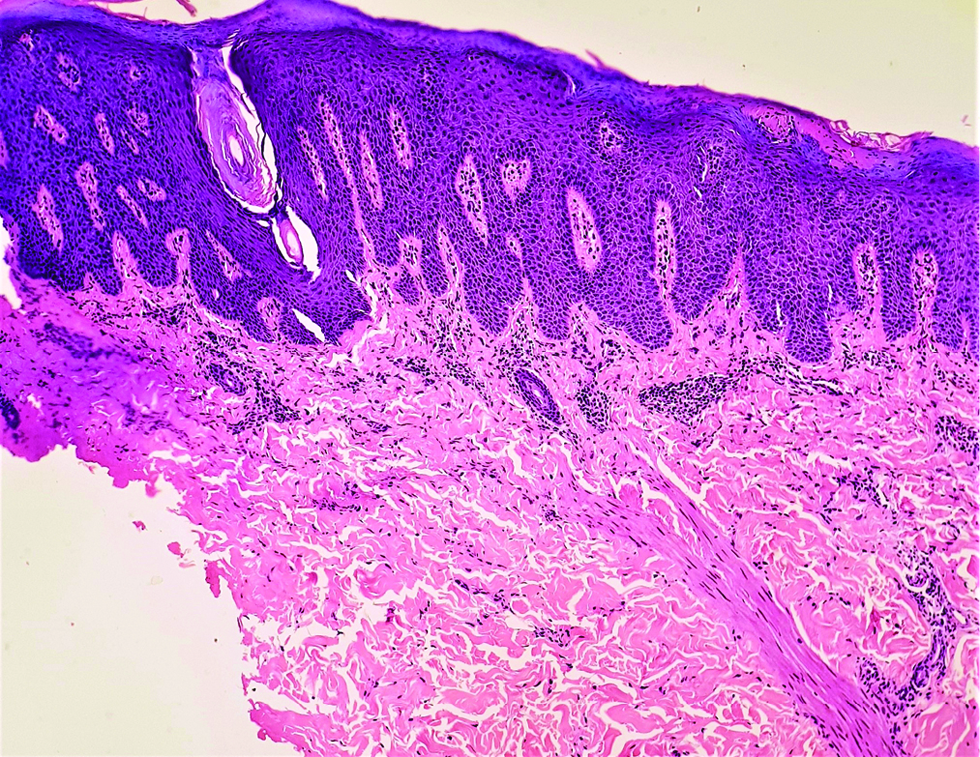
- Histopathology shows orthokeratosis, confluent parakeratosis with neutrophilic collections in stratum corneum and spinosum, psoriasiform hyperplasia, dilated blood vessels, suprapapillary thinning, and perivascular lymphohistiocytic infiltrate in upper dermis (H&E ×100)
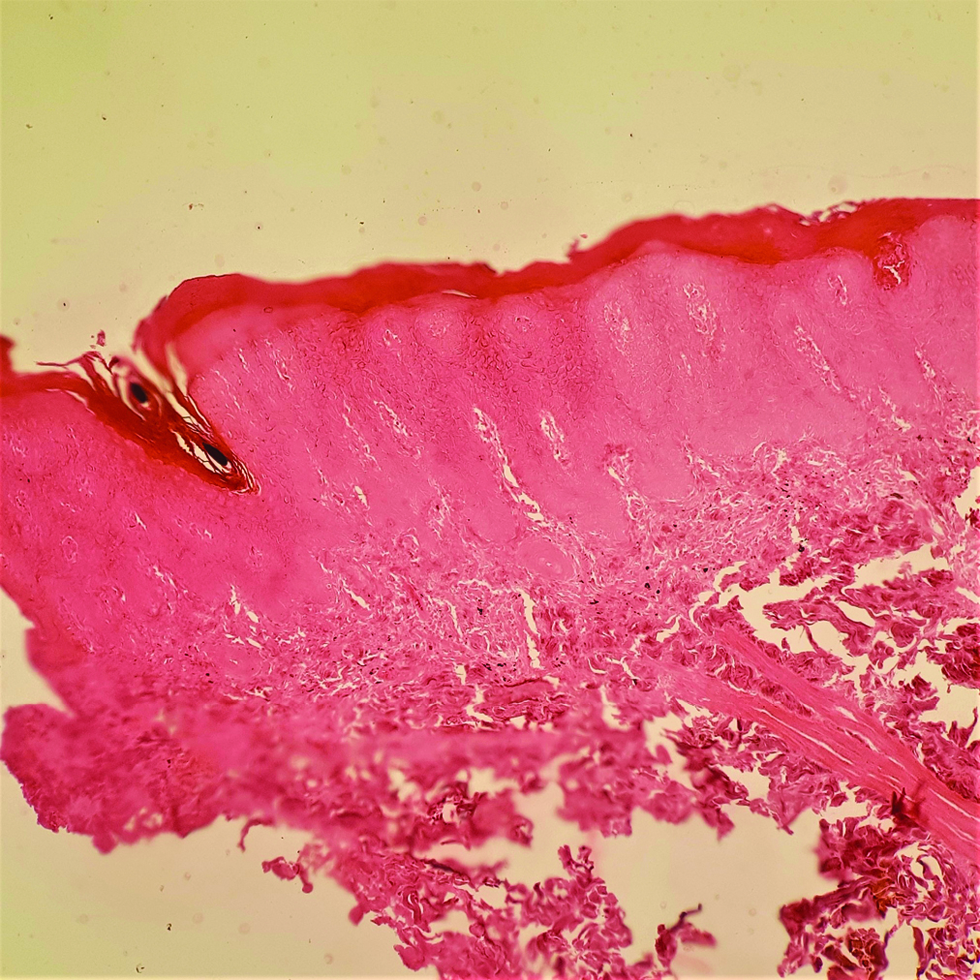
- Histopathology with special stain Masson Fontana shows loss of pigment and melanocytes in epidermis (Masson Fontana ×100)
All screening investigations for metabolic syndrome were within normal limits.
The patient was diagnosed with a case of colocalized vitiligo and psoriasis based on clinical, dermoscopic, and histopathological evaluation.
The diagnosis of both vitiligo and psoriasis is primarily clinical, with dermoscopy used as an auxiliary tool. Common dermoscopic features of psoriasis are red dots/globules, in a regular distribution along with diffuse white scales against a pinkish background. For vitiligo, dermoscopic features include loss of pigment and altered pigment network. Specific morphological patterns like starburst, comet tail, trichrome, and salt and pepper patterns have also been described.
Our case showed overlapping clinical as well as dermoscopic features, also confirmed by histopathology.
Currently, there are few studies investigating a common etiological link between psoriasis and vitiligo which could simply be a coincidence, but it has been hypothesized that people with one immune-mediated inflammatory condition are more likely than controls to have another.[1]
A recent meta-analyses by Yen et al. found that when compared with controls, psoriasis patients were 2.29-fold more likely to have vitiligo, while vitiligo patients were 3.43-fold more likely to be diagnosed with psoriasis.[1]
T-helper1 and T-helper17 pathways have been proposed as a source of hyperactive cellular response in both to explain a similar cell-mediated immune pathology.
Bassiouny et al. indicated that IL-17A levels in serum and lesional skin were higher in vitiligo patients, correlating with disease severity and duration.[2] Also, greater numbers of IL-17A-producing cells were discovered in colocalized psoriasis-vitiligo lesions in a recent study.[3]
In addition, increased levels of Tumor Necrosis Factor-alpha have been observed in perilesional skin of vitiligo patients, as well as in psoriatic lesions.[4]
A case-control study of 463 vitiligo patients by Arunachalam et al. found that 27 patients had concomitant psoriasis (two had colocalized disease). Inflammatory-type vitiligo and a positive family history of cardiovascular disease were the greatest predictors of concurrent psoriasis, implying shared inflammatory pathways and genetic susceptibility between psoriasis, vitiligo, and cardiovascular morbidity.[5]
Last but not the least, a treatment overlap supports the hypothesis of a close relationship between the two, as evidenced by promising preliminary results for tofacitinib’s effectiveness in both. In psoriasis it acts by inhibiting activation of JAK/STAT-dependent cytokines, blocking Th17 activation and IL-17 production, and in vitiligo by reducing IFNγ and JAK-STAT mediated destruction of melanocytes by T cells.[1]
To conclude, this is a rare case with vitiligo and psoriasis colocalizing, and the first to emphasize the dermoscopic overlap, prompting us to investigate a relationship that could have substantial treatment implications and their association with systemic autoimmune diseases which will also aid in screening, including markers of cardiovascular risk. Several theories have been proposed to explain their coexistence, but more research is needed to determine the common pathways that cause these disorders to coexist and colocalize.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Association between psoriasis and vitiligo: A systematic review and meta-analysis. Am J Clin Dermatol. 2019;20:31-40.
- [CrossRef] [PubMed] [Google Scholar]
- Role of interleukin-17 in the pathogenesis of vitiligo. Clin Exp Dermatol. 2011;36:292-7.
- [CrossRef] [PubMed] [Google Scholar]
- Coexistent skin lesions of vitiligo and psoriasis vulgaris. Immunohistochemical analyses for IL-17A-producing cells and regulatory T cells. Acta Dermato Venereologica. 2014;94:329-30.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrence of vitiligo and psoriasis: A simple coincidence? Clin Exp Dermatol. 2009;34:90-1.
- [CrossRef] [PubMed] [Google Scholar]
- Non-segmental vitiligo and psoriasis comorbidity - A case-control study in Italian patients. J Eur Acad Dermatol Venereol. 2014;28:433-7.
- [CrossRef] [PubMed] [Google Scholar]






