Translate this page into:
Coexistence of neurofibromatosis 1 and vitiligo

*Corresponding author: Logamoorthy Ramamoorthy, Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. logamoorthy.r@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramamoorthy L, Rout N. Coexistence of neurofibromatosis 1 and vitiligo. CosmoDerma 2023;3:126.
Dear Sir,
Von Recklinghausen’s disease is an autosomal dominant condition characterized by multiple soft-tissue tumors arising from Schwann cells and fibroblasts.[1] It is rarely associated with autoimmune diseases, of which association with vitiligo is reported in a few cases.[1,2] Herein, we report a case of neurofibromatosis 1 (NF1) coexistence with vitiligo.
A 47-year-old male case of NF1 presented with hypopigmented to depigmented patches all over the body for the past 2 years. There is no family history suggestive of NF and hypopigmented lesions. On clinical examination, axillary freckling, palmar freckling, and multiple well-defined light brown macules consistent with café-au-lait macules were present. Multiple soft, sessile, and pedunculated, dome-shaped, papulonodular lesions ranging from 1 mm to 15 mm in size distributed all over the body suggestive of neurofibromas. Ophthalmological examination revealed Lisch nodules. Multiple, well-defined, depigmented macules of size ranging from 0.1 cm to 10 cm over the right forearm, abdomen, and bilateral legs were present [Figure 1a-c]. Dermatoscopy of the depigmented macules showed a white glow with a starburst pattern, perifollicular pigmentation, trichome sign, and tapioca sago appearance [Figure 2a and b]. A diagnosis of NF1 with the coexistence of vitiligo was made. The patient was treated with topical clobetasol ointment and soaked PUVASOL for vitiligo vulgaris.
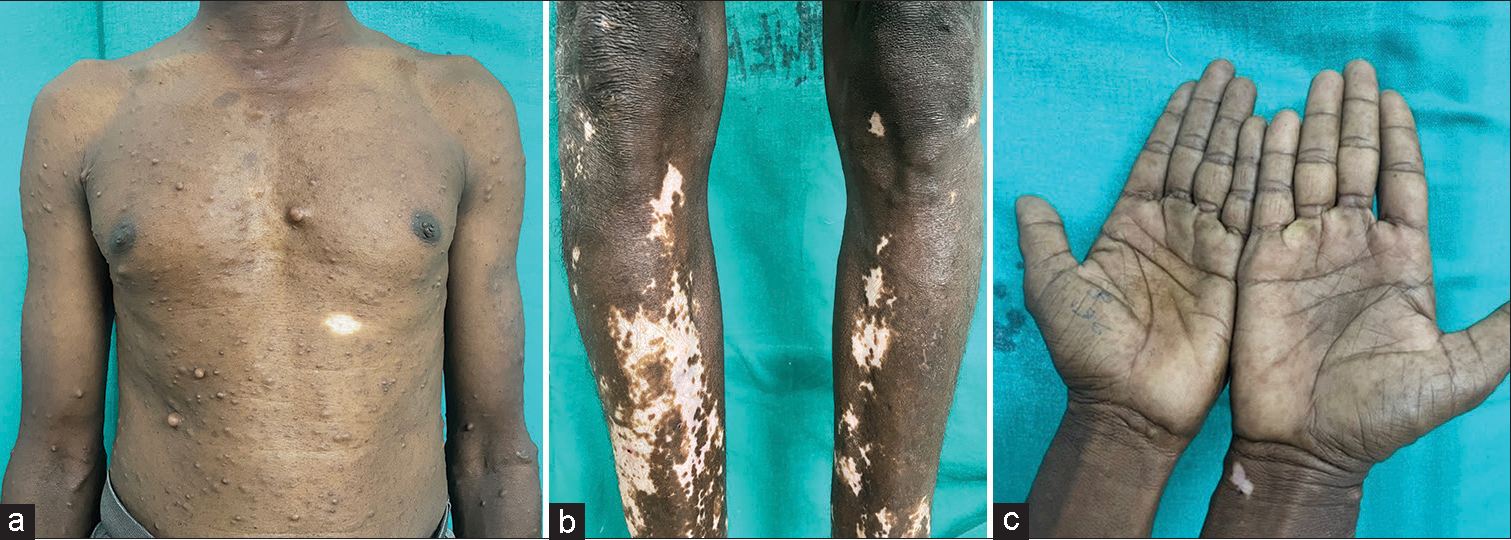
- (a) 47-year-old male case of neurofibromatosis 1 showing multiple neurofibromas over the trunk and a single depigmented macule over the upper abdomen. (b) Multiple depigmented macules over the bilateral legs. (c) Palmar freckling with single depigmented macule over the right wrist.
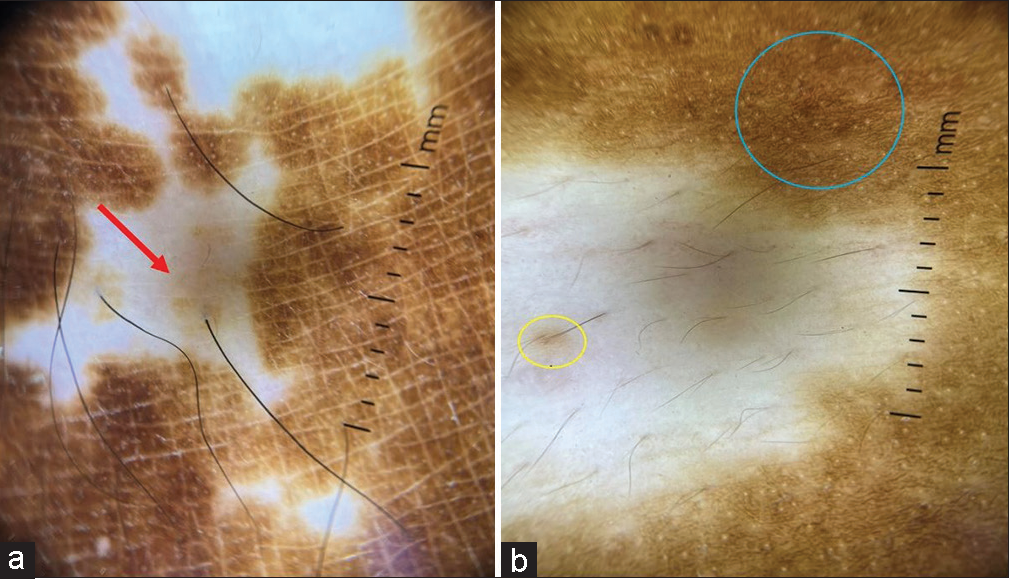
- (a and b) Dermatoscopy (Non-polarised Dermlite 4 ×10) of depigmented macule shows white glow, starburst pattern (red arrow), perifollicular pigmentation (yellow circle), trichome sign, and tapioca sago sign (blue circle).
NF 1, also called von Recklinghausen’s disease caused by a mutation in the neurofibromin one gene located on chromosome 17q11.2.1 NF, is associated with autoimmune disorders like systemic lupus erythematosus, multiple sclerosis, mixed connective tissue disease, immunoglobulin A nephropathy, bullous pemphigoid, Grave’s disease, and autoimmune hemolytic anemia.[1-3] Vitiligo is a disorder affecting melanocytes characterized by macular depigmentation of varying sizes or shapes. The coexistence of vitiligo and NF1 may be a coincidence finding in our patient. There is a hypothesis that abnormal neurofibromin production can cause decreased T-cell apoptosis which may be an underlying factor for developing vitiligo.[4] Another theory is neurofibromin which is present in the melanocyte membrane. It forms a complex with amyloid precursor protein. Hence, the mutation in the NF1 gene leads to abnormal transport of melanosomes leading to pigment-related manifestations such as hypopigmented macules, vitiligo, and café-au-lait macules.[5] Miraglia et al. reviewed all 1102 charts of NF1 patients from 1983 to February 2020 at the “Sapienza” University of Rome, Italy, to see the actual prevalence of cutaneous manifestations of NF1. Vitiligo was present in 25 cases (2.3%), of which seven patients had generalized vitiligo and 18 patients had localized vitiligo.[6] Based on previous reports and our case, association between NF1 and vitiligo is not a coincidence but a potential association.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neurofibromatosis Type 1 in the setting of systemic lupus erythematosus. Cutis. 2019;103:E9-12.
- [Google Scholar]
- Autoimmune diseases associated with neurofibromatosis Type 1. Pediatr Dermatol. 2008;25:392-3.
- [CrossRef] [PubMed] [Google Scholar]
- Bullous pemphigoid and neurofibromatosis-a chance association requiring special vigilance. Clin Exp Dermatol. 2000;25:658-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neurofibromatosis and vitiligo: A simple coincidence or coexistence? Int J Rheum Dis. 2022;25:506-7.
- [CrossRef] [PubMed] [Google Scholar]
- Neurofibromatosis Type 1 protein and amyloid precursor protein interact in normal human melanocytes and colocalize with melanosomes. J Invest Dermatol. 2006;126:653-9.
- [CrossRef] [PubMed] [Google Scholar]





