Translate this page into:
Bullous dermatophytosis

*Corresponding author: P. Vishnu, Department of Dermatovenereology, Velammal Medical College and Research Institute, Madurai, Tamil Nadu, India. vishnusgm02@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sriram CK, Vishnu P. Bullous dermatophytosis. CosmoDerma 2023;3:136.
A 12-year-old boy who is studying 7th standard was evaluated for fluid-filled pruritic lesions over the groin and lower abdomen for the past 1 month. There was no history of any topical applications. He was staying in a hostel and his roommates were getting treatment for dermatophytosis. On examination, there were multiple flaccid bulla and vesicles of varying sizes seen distributed over the lower abdomen and there was a single annular scaly plaque with central clearing [Figure 1]. Clinically, the differential diagnosis of impetigo and bullous scabies was considered. There were no mites and mite products seen in the skin scarping. The Tzanck smear was negative for acantholytic cells. The fluid from the vesicle was subjected to 10% potassium hydroxide (KOH) mount and it revealed thin, slender, refractile, branching, and septate hyphae suggestive of cutaneous dermatophytes [Figure 2]. Hence, a diagnosis of bullous dermatophytosis was made and he was started on oral capsule itraconazole 100 mg BD and topical luliconazole for 6 weeks twice daily application.

- Multiple flaccid fluid-filled vesicles and bulla in the lower abdomen and groin (Black arrows). A single scaly annular plaque with central clearing (white arrow).
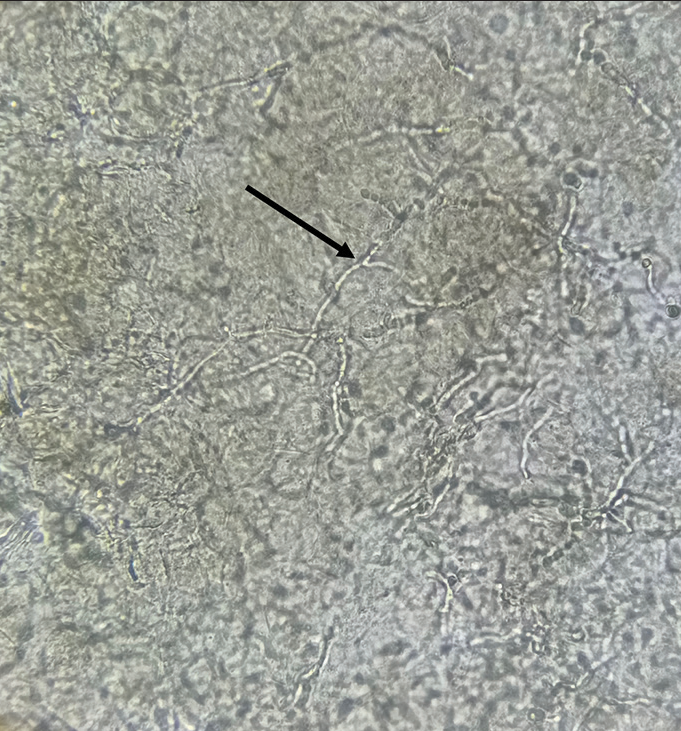
- 10% potassium hydroxide mount under ×40 magnification showing long, thin, slender, branched, and septate hyphae.
Various clinical presentations of cutaneous dermatophytosis are verrucous, plaque, eczematous, crusted, herpetic, and subcutaneous nodular (Majocchi’s granuloma) type. Bullous dermatophytosis is an uncommon clinical presentation that is most often caused by Trichophyton rubrum or Trichophyton mentagrophytes.[1] “Tinea corporis bullosa” was the term used for such rare presentation. They were commonly reported at hands and foot, and sometimes, they may be confined to the borders, called as “tinea corporis bullosa annularis.” Bulla occurs as a result of inflammatory response secondary to a delayed hypersensitivity which is provoked by the dermatophyte antigens. Often, it is mistaken for contact dermatitis, herpetic infection, and impetigo and dyshidrotic eczema. KOH examination and family history of tinea infection will help to rule out others.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Clinical and immunological studies in chronic dermatophytosis caused by Trichophyton rubrum. Acta Derm Venereol. 1984;64:493-500.
- [CrossRef] [PubMed] [Google Scholar]





