Translate this page into:
Calcinosis universalis in a case of juvenile dermatomyositis

*Corresponding author: Yamini Sihag, Department of Dermatology, All India Institute of Medical Sciences, Rajkot, Gujarat, India. yaminisihag174@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sihag Y, Tyagi S, Singh A. Calcinosis universalis in a case of juvenile dermatomyositis. CosmoDerma. 2024;4:87. doi: 10.25259/CSDM_102_2024
A 7-year-old female presented with multiple well-defined, non-tender, erythematous, and hyperpigmented noduloplaques with surfaces showing white, gritty hard deposits present over both elbows, axillae, iliac crests, and knees for the past 1.5 years [Figure 1a]. Features of proximal muscle weakness along with heliotrope rash, Gottron’s papules, and malar rash were also present. Investigations revealed anti-NXP-2 antibodies and elevated creatinine phosphokinase (CK-NAC: 270.7 IU/L [Normal < 145 IU/L]; CK-MB: 62.8 IU/L [Normal 0–24 U/L]) and (lactate dehydrogenase: 350 IU/L, Normal 110–295 IU/L) levels with no abnormality in serum calcium and phosphorus levels. X-rays of the limbs showed diffuse soft-tissue calcifications [Figure 1b], while ultrasound of the abdomen revealed multiple calcific foci dispersed throughout the renal cortex and spleen [Figure 1c]. The final diagnosis of juvenile dermatomyositis (JDM) with calcinosis cutis was made based on clinical and laboratory findings. The patient was started on oral nifedipine with good response in cutaneous lesions; however, no improvement was noted in visceral calcification ([Figure 1d and e] at three and six months, respectively).
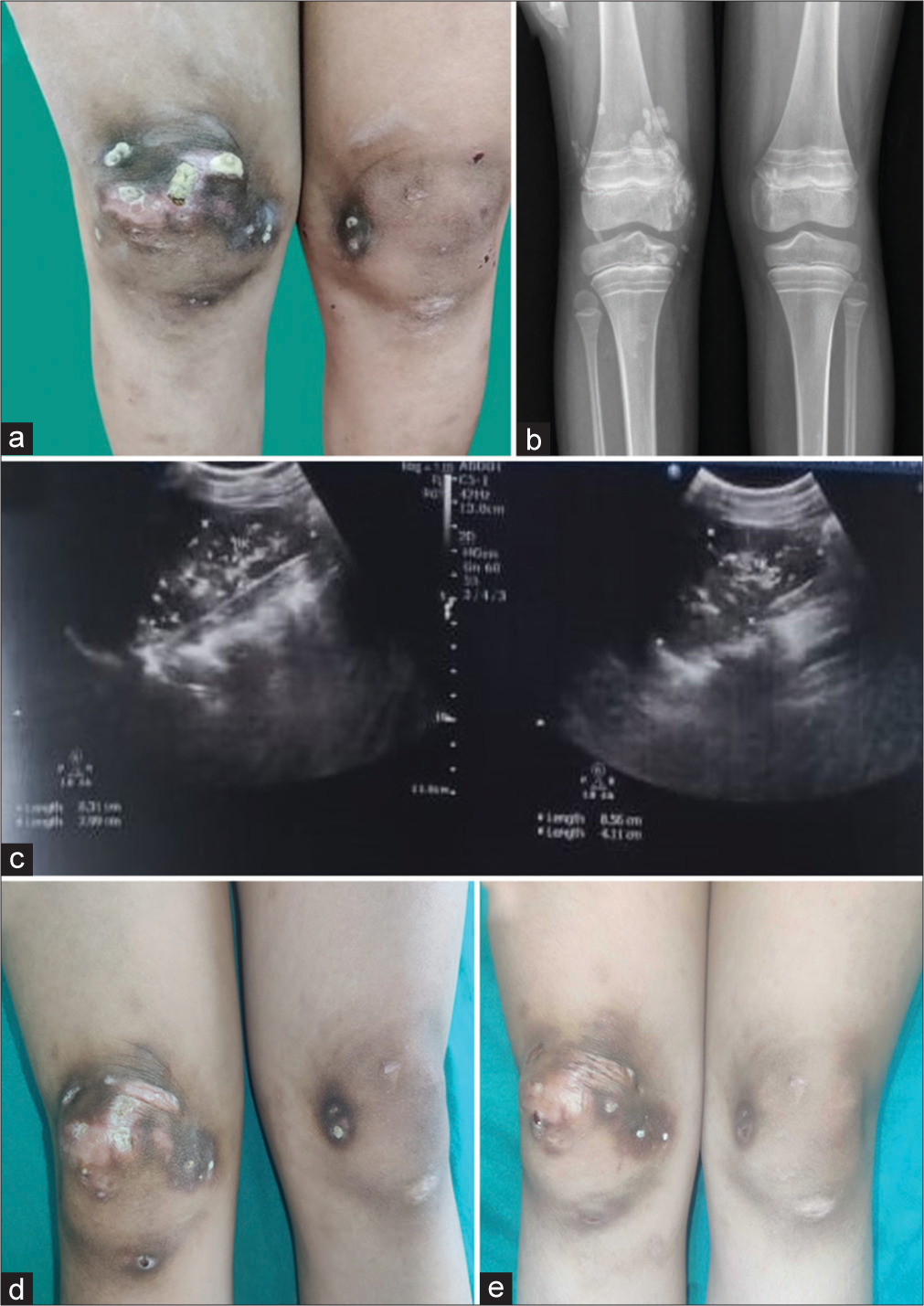
- (a) Well-defined, erythematous to hyperpigmented noduloplaques with surfaces showing white, gritty hard deposits over both knees. (b) X-ray of lower limbs showing diffuse soft tissue calcifications. (c) Ultrasound abdomen showing multiple calcific foci dispersed throughout the renal cortex. (d) Post treatment image showing good response in calcinosis cutis at 3 months. (e) Post treatment image showing good response in calcinosis cutis at 6 months.
Dermatomyositis (DM) is an idiopathic inflammatory myopathy with typical cutaneous manifestations, along with systemic involvement. It shows a bimodal presentation with JDM commonly occurring between 4 and 14 years of age.[1] Calcinosis cutis is noted in up to 40% of cases with JDM which is higher than that noted in adult DM.[1,2] Anti-NXP2 antibodies, detected in 20–25% of cases of JDM, are associated with calcinosis cutis, debilitating myositis requiring aggressive treatment and poor prognosis.[1] While calcification is a common cutaneous manifestation, visceral organ calcification is very rarely reported. We present a case of JDM presenting with cutaneous, as well as renal and splenic calcification.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermatomyositis: Clinical features and pathogenesis. J Am Acad Dermatol. 2020;82:267-81.
- [CrossRef] [PubMed] [Google Scholar]
- Calcinosis in juvenile dermatomyositis: Updates on pathogenesis and treatment. Front Med (Lausanne). 2023;10:1155839.
- [CrossRef] [PubMed] [Google Scholar]





