Translate this page into:
Aquagenic syringeal acrokeratoderma localized to palmar creases

*Corresponding author: Sudhesan Athira, Department of Dermatology, Government Medical College, Kollam, Kerala, India. athirasudhesan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Athira S, Haridasan Pillai H, Subramoniam L, Simon SA, Ashok P. Aquagenic syringeal acrokeratoderma localized to palmar creases. CosmoDerma 2023;3:155.
Abstract
Aquagenic syringeal acrokeratoderma (ASA) is a rare acquired condition, characterized by translucent papules and plaques mainly involving the palmar surface, which develops after 2–4 min of exposure to water. We present the case of a young female with a history of migraine on flunarizine tablet, who presented with whitish translucent papules and plaques along the palmar creases after exposure to water for 2–3 min. Dermoscopy revealed whitish elevations with dilated sweat duct openings and histopathology showed dilated acrosyringium in the stratum corneum and proliferation of eccrine glands in the dermis. The patient showed partial improvement with topical 20% aluminum chlorohydrate and antihistamines.
Keywords
Aquagenic syringeal acrokeratoderma
Migraine
Flunarizine
INTRODUCTION
Aquagenic syringeal acrokeratoderma (ASA) is a rare acquired condition of uncertain etiology. It is characterized by translucent papules and plaques mainly involving the palmar surface, which develops after 2–4 min of exposure to water. The condition appears to predominantly affect adolescent and young adult women. Several pathogenic mechanisms have been proposed, including structural or functional defects of the stratum corneum during adolescence, primary disease of the sweat ducts, increased sodium concentration in the skin, thereby increasing the water-retention capacity of the horny layer or a reaction to drugs.[1]
We report a case of a woman who used flunarizine tablets for migraine and developed ASA which predominately involved the palmar creases.
CASE REPORT
A 21-year-old female presented to the Dermatology Outpatient Department of Government Medical College Kollam, Kerala, with a 7-month history of asymptomatic raised lesions on the palms after exposure to water. The lesions developed after 2–3 min of contact with water and occurred regardless of water temperature. The condition spontaneously resolved within 5–10 min after exposure to water was ceased without any sequelae. On examination, the physical appearance of her palms before immersion in water was normal, except for the hyperlinearity. The patient was asked to soak her hands in water for 2–3 min at different temperatures. Then, small whitish translucent papules and plaques appeared on both palms predominantly along the creases [Figure 1]. No such lesions were noticed on soles after exposure to water. Dermoscopy revealed whitish elevations with dilated sweat duct openings and preservation of dermatoglyphics [Figure 2]. Histopathological examination showed ortohyperkeratosis of stratum corneum with dilated acrosyringium [Figure 3a]. There was perivascular and peri-adnexal mild lymphoplasmacytic infiltration in the upper dermis and the lower dermis showed proliferation of eccrine glands with capillary proliferation around the glands [Figure 3b]. Focal eccrine glands had a crenulated appearance [Figure 3c].
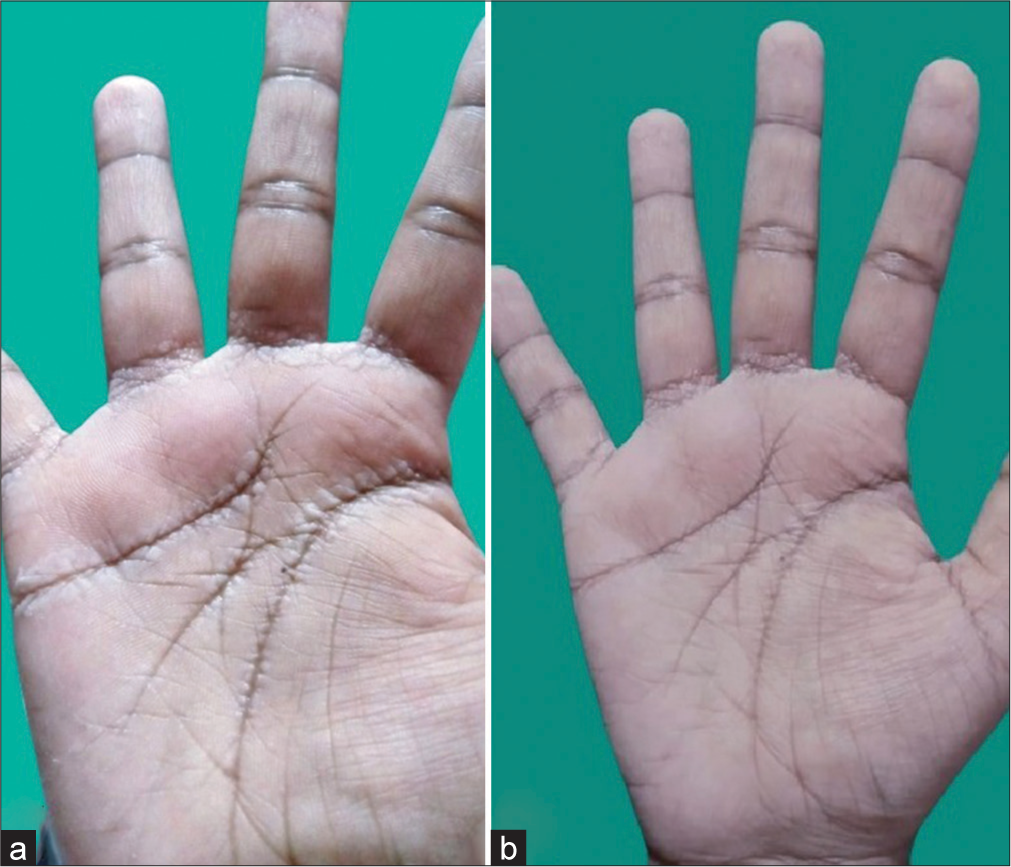
- (a) Clinical image of right hand after soaking in water for 5 min. There are whitish translucent papules and plaques along the palmar creases giving rise to a pebbly appearance. (b) After treatment image taken 2 weeks after starting treatment with topical 20% aluminum chlorohydrate and systemic antihistamine, showing partial response.
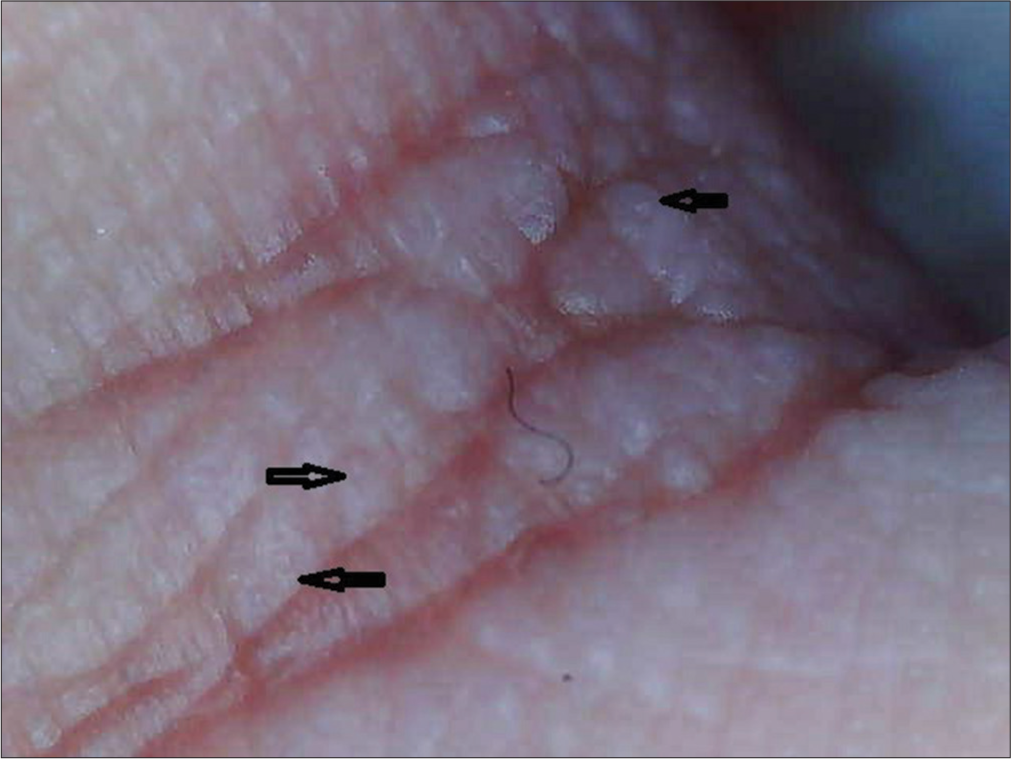
- Dermoscopy (Dino-Lite AM2111) showing dilated sweat duct openings (×40), black arrows.

- Histopathological examination (hematoxylin and eosin) showing (a) ortohyperkeratosis of stratum corneum with dilated acrosyringium (H& E ×400, black arrow). (b) Proliferation of eccrine glands in the lower dermis (H&E ×100, black arrow). (c) Focal eccrine glands showing crenulated appearance (H&E ×400, black arrow).
From her medical history, we learned that she had chronic headache for the past 2 years, which diagnosed as migraine, and was on flunarizine tablet for the past 1 year. Palmar lesions on exposure to water developed 5 months after starting flunarizine. She denied any associated hyperhidrosis. Neither the patient nor any of the close family members had similar lesions. There were no clinical features suggestive of cystic fibrosis. We could not do the sweat chloride test as she was not willing for any further investigations.
The patient was diagnosed with ASA. Considering the temporal association between flunarizine intake and the development of skin lesions, the patient was asked to stop flunarizine. She was given 20% aluminum chlorohydrate and antihistamines and showed partial improvement with this treatment (shown in the after treatment image). She was reassured that the condition is transient and benign. Reintroduction of flunarizine was not done in our patient as the drug was already substituted in her. Based on the World Health Organization-Uppasala Monitoring Centre causality assessment, flunazirine was considered the possible cause of ASA in this case.[2]
DISCUSSION
ASA was first described in 1996 by English and McCollough as transient reactive papulotranslucent acrokeratoderma.[3] Subsequently, it has been described under various names in the literature as aquagenic palmoplantar keratoderma, aquagenic keratoderma, and aquagenic wrinkling of the palms. The term ASA refers to the dramatic initiation of the lesions after exposure to water, keratoderma in acral sites, and dilated sweat ducts. Although there is no consensus regarding the nomenclature of this condition, we feel that the term ASA seems to be the apt term considering the morphology and histopathological appearance of this rare entity. The hand-inthe-bucket sign (papules appear due to the immersion of both hands into warm or cold water for 3–5 min) is considered pathognomonic sign.[4] Aquagenic syringeal acrokeratoderma has been reported mainly in young females, but a case series of 10 patients from Turkey showed a male predominance.[5] The condition is postulated to have a genetic basis, with both autosomal dominant and recessive patterns of inheritance,[6] but most reported cases are sporadic. It is reported to be associated with palmar/plantar hyperhidrosis, atopy, cystic fibrosis, malignant melanoma,[5-7] certain drugs including tobramycin,[8] cyclooxygenase-2 (COX-2) inhibitors, such as rofecoxib,[9] celecoxib,[10] aspirin,[11] and aldosterone antagonist and potassium-sparing diuretic, spironolactone.[1] Its association with cystic fibrosis and COX-2 inhibitors suggests increased salt content in the stratum corneum leading to these changes. The association with spironolactone is thought to be associated with upregulation of COX-2 expression.[1]
Various treatments have been tried in this condition including topical 10% urea in combination with 10% salicylic acid, 20% aluminum hydroxychloride, antihistamines, and botulinum toxin injection with variable response.[5]
Similar to the previously reported cases, this patient with ASA was a young female. However, unlike other cases, our patient developed lesions along the palmar creases. Furthermore, the association of ASA with migraine or flunarizine has not been reported previously. Flunarizine is a non-selective calcium antagonist, which has also been shown to block voltage-gated sodium channels.[12] It may affect ASA by blocking the cell surface channels and receptors, which may influence cell-volume regulation. The mechanism of its localization to palmar creases is not clear. Further research is needed to understand the pathomechanisms of this rare condition.
CONCLUSION
Aquagenic syringeal acrokeratodema is an uncommon disorder of uncertain etiology. Drugs may play a role in its development. Dermatologists should be aware about this rare condition in order to make prompt diagnosis. 20% aluminium chlorohydrate is a promising option when treatment is necessary.
Declaration of patient consent
The patient’s consent was not required as the patient’s identity was not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Aquagenic syringeal acrokeratoderma. Indian J Dermatol. 2014;59:632.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse drug reaction and causality assessment scales. Lung India. 2011;28:152-3.
- [CrossRef] [PubMed] [Google Scholar]
- Transient reactive papulotranslucent acrokeratoderma. J Am Acad Dermatol. 1996;34:686-7.
- [CrossRef] [PubMed] [Google Scholar]
- Familial aquagenic acrokeratoderma: Case reports and review of the literature. Int J Dermatol. 2005;44:906-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired aquagenic syringeal acrokeratoderma: A case series of 10 patients. Australas J Dermatol. 2015;56:e43-5.
- [CrossRef] [PubMed] [Google Scholar]
- Aquagenic syringeal acrokeratoderma. Indian Dermatol Online J. 2016;7:327-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of aquagenic syringeal acrokeratoderma. Int J Dermatol. 2016;55:e407-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tobramycin-induced aquagenic wrinkling of the palms in a patient with cystic fibrosis. Clin Exp Dermatol. 2009;34:e75-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rofecoxib-induced instant aquagenic wrinkling of the palms. Pediatr Dermatol. 2002;19:353-5.
- [CrossRef] [PubMed] [Google Scholar]
- Celecoxib-induced aquagenic keratoderma. Actas Dermosifiliogr. 2005;96:537-9.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral aquagenic wrinkling of the palms associated with aspirin intake. Arch Dermatol. 2006;142:1661-2.
- [CrossRef] [PubMed] [Google Scholar]
- Current prophylactic medications for migraine and their potential mechanisms of action. Neurotherapeutics. 2018;15:313-23.
- [CrossRef] [PubMed] [Google Scholar]






