Translate this page into:
Adverse effects of nail cosmetics and how to prevent them

*Corresponding author: Chander Grover, Department of Dermatology and STD, UCMS and GTB Hospital, Delhi, India. chandergroverkubba76@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bansal S, Grover C. Adverse effects of nail cosmetics and how to prevent them. CosmoDerma. 2024;4:44. doi: 10.25259/CSDM_23_2024
Abstract
Nail cosmetics are being used world over for nail enhancement, and their list is an ever expanding one. However, due to their widespread usage, there are an increasing number of adverse effects also being reported. These have been reported both in the users as well as service providers (nail salon workers/technicians). Adverse effects to nail cosmetics usually present to dermatologists, who need to be equipped to suspect, diagnose, and manage them. A whole range of newer nail cosmetic products are available now, which can lead to a variety of adverse reactions. These may be early and hence easy to temporally correlate with cosmetic usage; or have a delayed onset making it difficult to correlate with the nail cosmetic used. Varying presentations include onycholysis, infections, allergic dermatitis, psoriasiform nail changes, and systemic adverse effects. The range of clinical manifestations, prevention, and management of nail cosmetic-related adverse effects are detailed in this review.
Keywords
Nail cosmetics
Adverse effects
Nail polish
Acrylates
Gel nails
2-Hydroxy-ethyl methacrylate
INTRODUCTION
Nails are considered to be an expression and extension of one’s personality. Hence, nail enhancement with nail cosmetics is being done by millions of users the world over, irrespective of their gender and ethnicity. The impact of nail cosmetics is so much that a study assessing self-cosmetic care during the COVID-19 pandemic concluded that female medical students not doing cosmetic care of nails during the lockdown period, perceived a significant negative social impact.[1] On the flip side, an increment in the incidence of adverse effects related to nail cosmetics is also being seen due to their increased usage. This is especially common among inexperienced or unaware users.
Even though adverse effects are a reality, nail cosmetics are here to stay, because not only do our patients love them, dermatologists can also use them to advantage in a number of otherwise untreatable nail conditions or as good camouflage options.[2] Nail cosmetics have been found useful in patients with nail plate surface abnormalities including onychoschizia, pitting, onychorrhexis, habit tic deformity, onychophagia, and anonychia.[3,4] Starace et al. demonstrated that the daily application of a cosmetic topical treatment product containing Pistacia lentiscus and hyaluronic acid can improve common nail diseases including nail fragility and onychomycosis.[5] The ease of application and cosmetic elegance contributed to a greater acceptance by the patients.
Nail cosmetic usage is witnessing an upward trend. Hence, it is important for dermatologists to familiarize themselves with the various nail cosmetics being used by the public and the range of adverse effects possible. This review aims to discuss these along with the preventive measures that can be taken to minimize them.
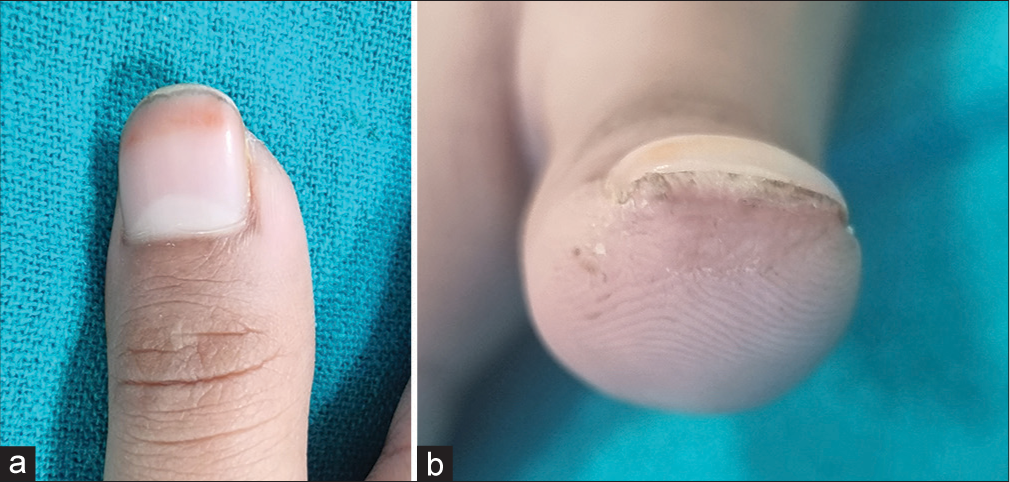
TYPES OF NAIL COSMETICS
Gone are the days of simple nail polish. Now, we have a range of different types of nail cosmetics available and being used [Table 1]. Their purpose is to enhance the esthetic appeal of the nails and give them a healthy and nourished appearance, which is considered indicative of the social status of a person as well [Figure 1a and b]. These are also being used for diseased nails, as camouflage for the distorted appearance, enhancement of cosmetic appeal, ensuring a smooth, shiny appearance, lengthening them by artificial extension, or strengthening them (like gel nails being used for brittle nails). The adverse effects may be due to individual predisposition or incorrect usage. The commonly used nail cosmetics with adverse effects associated with them are discussed below.
| Nail polish |
The constituents of nail polish include
|
| Nail polish variants |
|
| Nail polish removers |
|
| Nail shellacs |
|
| Artificial nails |
|
| Nail adornments |
|
| Nail moisturizers |
|

- (a and b) Appearance of the nail plate, when enhanced with cosmetics. This is perceived to indicate societal status and well-being.
Nail polish
The most common use of nail polish is for the beautification of nails. However, it is also used for strengthening brittle nails and camouflaging discolored and irregular nails. Nail polish is actually a mixture of an assortment of various components as shown in Table 2. Adverse effects related to nail polish can be many. It can lead to nail damage due to its ingredients, the way it has been used, or more importantly, the way it has been removed. Salient nail polish related adverse effects include:
| Basic constituents of nail polish | Components | Role in nail polish |
|---|---|---|
| Film forming agents | Nitrocellulose, methacrylate polymers, and vinyl polymers | |
| Film forming resins | Formaldehyde, TSFR | Lead to adherence and prevention of chipping of nail paint TSFR is a potent cause of contact allergic dermatitis |
| Plasticizers | Diethylpthhalate, dibutyl phthalate, dioctyl- phthalate, tricresyl phosphate and camphor |
Prevention of chipping Maintain pliability of the product |
| Solvents and diluents | Responsible for quick drying of nail paint Leave colored film behind |
|
| Colorants | Various organic and inorganic pigments | |
| Thickening agents | Clay derivatives | Uniform suspension of ingredients |
| Color stabilizers | Benzophenone and Etocrylene Mineral pigments: Zinc oxide, Titanium oxide, Iron oxide Synthetic pigments: D and C red 6/7/19, FDC Yellow |
Prevent UV-induced color fading |
TSFR: Toluene sulfonamide formaldehyde resin, UV: Ultraviolet
Discoloration of the nail plate
On repeated usage, various colorants, especially the red or yellow color of the nail polish, tend to stain the nail plate. It is a consequence of harmless keratin staining. This pattern of staining can be reproduced solely with the pigments D and C red no 7, D and C red no 34, D and C red no 6, and FD and C yellow no 5 lake.[6] The likelihood of residual staining increases with nail polishes in which the pigments are dissolved and not suspended. If the nail polish is left on for longer periods, especially more than seven days, the discoloration starts developing. Upon removal of nail polish, the discoloration tends to self resolve over two weeks. Such discoloration of the nail plate can often be prevented by using a basecoat.[7] However, the base coat may not always provide protection.
Keratin degranulation
It is a type of pseudo-leukonychia, which can result from nail polish binding and subsequently being removed from the nail plate.[8] The nail polish interacts with keratin leading to the appearance of white striae [Figure 2]. Clinical presentation can also be in the form of macules or patches on the nail plate. Onychoscopy shows white areas corresponding to the areas of nail plate exfoliation.[9] The condition can be clinically misdiagnosed as superficial white onychomycosis.[9] Management includes gentle nail care and avoiding frequent contact with irritant and allergenic grooming products including nail polish and remover.[10]

- Pseudoleukonychia or keratin degranulation seen after prolonged nail polish application and removal.
Allergic contact dermatitis
This should be suspected in a patient presenting with itching and/or scaling in the periungual region [Figure 3]. However, manifestations may not be limited to the nail unit, but can also occur in distant regions, wherever the nail tends to touch and transfer the allergen. The secondary film formers in nail polish are usually resins, especially Toluene Sulphonamide Formaldehyde Resin (TSFR) [Table 2]. TSFR has traditionally been recognized as the causative factor responsible for most cases of allergic contact dermatitis, including facial dermatitis in women.[11] The other common allergens include formaldehyde, nitrocellulose,[12] dibutyl phthalate,[13] and D and C yellow 11.[14] Various components of nail polish responsible for contact allergic dermatitis and its manifestations are shown in Table 3.

- Contact allergic dermatitis involving the periungual area, due to nail polish (ROAT or Repeat Open application Test done). Chronic paronychia with greenish discoloration (chloronychia) can also be seen.
| Adverse effect | Nail cosmetic implicated | Causative allergen/agent |
|---|---|---|
| Contact dermatitis | Nail polish | Nitrocellulose, formaldehyde, TSFR, dibutyl phthalate, butyl stearate, D and C yellow 11, nickel-based solvents |
| Nail adhesives | Methacrylate, ethyl-2-cyanoacrylate | |
| Acrylic nails | Methacrylate, hydroxyethyl methacrylate, benzoyl peroxide | |
| Gel nails | 2-HEMA and 2-HPMA | |
| Nail hardeners | Formaldehyde | |
| Onycholysis | Nail polish | TSFR |
| Acrylic nails | Methyl acrylate or cyanoacrylate nail glue | |
| Gel nails | Photo-onycholysis (If patient is taking tetracyclines or doxycycline) | |
| Nail hardeners | Formaldehyde | |
| Paronychia | Nail polish | Formaldehyde |
| Cuticle remover | Sodium and potassium hydroxide | |
| Gel nails | Cyanoacrylate glue |
TSFR: Toluene sulfonamide formaldehyde resin, 2-HEMA: 2-hydroxyethyl methacrylate, 2-HPMA: 2-hydroxypropyl methacrylate
As the most common allergen in nail polish is TSFR, a variety of “toxin-free nail polishes,” free of it, are available. These are promoted as hypoallergenic and contain cellulose, acetate, butyrate, and polyester resins. However, they may contain plasticizers such as dibutyl phthalate for softness and pliability, dissolved in solvents (N-butyl acetate or ethyl acetate). Nail polishes free of toluene, phthalate, and formaldehyde are also available. These contain natural pigments in a water base. An important ingredient of these nail polishes is argan oil. Nevertheless, there are reports of allergic reactions to these “hypoallergenic nail polishes” as well, since most brands can have at least one component that can trigger allergic reactions in individuals. Hence, it is suggested that before their usage, a patch test with specific allergens based on the exact composition of these products may be considered.[15]
Heavy metal-associated adverse effects
Nail plate fragility and cracks can occur due to chronic and slow exposure to low levels of lead and arsenic in nail polish.[16] As of now lead and arsenic usage in cosmetics is restricted as they can cause long-term systemic disease as well. Nickel in nail polish can cause contact allergy, with nail and skin problems.[17] Kim et al. studied the presence of heavy metals in nail cosmetics and concluded that their content was lower than the permissible limit; hence, nail cosmetics may not pose a lifetime cancer risk.[18] However, with continued usage over a long period, the risk still needs to be kept in mind.
Nail polish removers
The process of nail polish removal involves the dissolution of the resin deposited on the nail plate surface. The remover is applied over the painted nail with the help of a cotton or tissue and removed or a cotton ball with remover is wrapped in an aluminium foil around the digital tip. Nail polish removers are also available in a variety of options. The common ones and their associated adverse effects are described below. To minimize these adverse effects, the products should be used sparingly and infrequently.
Acetone-based nail polish removers
Acetone is one of the commonly used organic solvents in most of the commonly available nail polish removers.[7] It is an irritant even at lower concentrations and leads to dry, lustreless nails.[7] In mild cases, it can also lead to onychoschizia or lamellar splitting of the nail plate [Figure 4]. In more severe cases, irritant dermatitis of the perionychial tissue is possible, especially if kept in contact for a longer period [Figure 5].
- Lamellar splitting of the distal end of the nail plate (onychoschizia) noticed after nail polish removal (Dermlite DL4 Polarized ×10).

- Dry, lustreless, brittle nails due to repeated use of acetone-based nail polish remover.
Acetone free nail polish removers
These contain ethyl acetate, butyl acetate or ethyl lactate. They have less odor and are relatively less drying in comparison to acetone. They are considered safe for human use.
Nail polish remover pads
These contain gamma-butyrolactone, considered safe and convenient to use. Rarely, there have been instances of conversion to gamma-hydroxybutyrate leading to systemic toxicity.[8]
Nail shellac
This product is a hybrid of nail polish and gel.[19,20] It resists chipping and can be worn over a normal nail plate. The shellacs, in comparison to gel nails, are less heavy and thinner. They can be easily removed with acetone. However, fracture of the nail plate can occur while removing nail shellac.
Nail hardeners
Nail hardeners are a set of products promoted as useful for soft, brittle, and thin nails, prone to splitting.[21] They are considered modifications of nail polish with a different solvent and resin concentration. In addition, they also contain keratin, vitamins, calcium fluoride, natural oils, nylon fibers, Teflon, and silk. The base coat of nail hardeners moves through the porous structure of the nail plate to provide it strength and flexibility. Their application also reduces transonychial water loss.
Although the purpose of nail hardeners is to strengthen the nail plate, their prolonged use can paradoxically lead to brittle nails, as the cross-link density within the nail plate increases and its flexibility is reduced. They should be periodically removed with nail polish removers. Other attributable adverse effects include contact allergic dermatitis, onycholysis, and subungual hyperkeratosis.[22]
Artificial nails
Long nails have always been considered a desirable and distinct sign of beauty, throughout human history. This can be achieved with the help of false nails or extensions placed to simulate a true nail. With advancements in this field, various techniques and products have been found useful to produce longer and stronger nails [Table 1]. However, their use is associated with mechanical and chemical adverse effects. Various types of artificial nails and their associated adverse effects are summarized below.
Nail tips are preformed tips that can be placed over a preexisting nail and trimmed to the desired shape. Adverse effects associated with their usage include onychoschizia or lamellar splitting of the nail, due to the mechanical tug on the nail plate and traumatic removal [Figure 6]. Due to the fact that nail tips are inflexible, they can lead to onycholysis as well. Cyanoacrylate glues, used as adhesive agents to fix the nail tips to the nail plate surface, can rarely lead to contact allergic dermatitis.
Nail wrap refers to the technique of applying linen, fiberglass or silk over the surface of a natural nail plate. This is done using glue, followed by the application of an acrylic coat. They have been used as a remedy for split nail deformity as well. Not many adverse effects have been reported.
-
Sculptured nails are nail substitutes applied over existing nail plates. These can be custom designed as per the size and shape of the nail on which they are to be worn. They can be either acrylic or gel based. Both these types involve a mixture of powder and a solution applied over the nail. It is important to have an understanding of the various materials used in the preparation/application of these nails, to have an insight into the adverse effects associated with them.
Acrylic nails are less popular currently due to various reasons including their less than natural appearance.[7] The application involves strong chemicals and fumes, which are not advisable in pregnancy. The process of application of acrylic nails involves the preparation of a polymerized acrylic by mixing liquid ethyl or isobutyl methacrylate with powdered polymethyl-methacrylate polymer.[8] A benzoyl peroxide accelerator is used to enhance polymerization. Sometimes, hydroquinone is used to slow down polymerization. The product hardens in 7–9 min and, therefore, needs to be applied quickly onto a chemically roughened nail plate. This application is done to the desired length and shape. A variation of this process involves preformed tips at the distal ends of the nail, making it quicker and less expensive to use. They do not require photocuring.

- Traumatic nail dystrophy due to removal of nail tips.
There are various adverse effects associated. Acrylates have been identified as potent allergens, necessitating the implementation of safety measures for the use of these chemicals in various nail techniques.[23] Over the past few years, there have been an increasing number of reports on allergic contact dermatitis due to acrylates. Among these, 2-Hydroxy-Ethyl Methacrylate (HEMA) is considered to be the main culprit.[24] HEMA was by far the most common ingredient of nail cosmetics, being present in nearly 60% of the products.
Worn-down nails (over-filed nails) are also an adverse effect seen as a direct consequence of procedure-induced trauma. It is seen typically with acrylic nail removal, where mechanical abrasion is required. The overfilled section of the nail is clinically visible as red in color due to nail plate thinning and the visibility of the nail bed underneath. Linear striations due to back-and-forth filing of nails may also be evident clinically, though better visualized onychoscopically. Dilated capillaries and pinpoint hemorrhages are the other onychoscopic features.
Gel nails - These are a commonly used cosmetic procedure, used to improve the appearance even in disease-induced nail disfigurement.[25] They have been used in various indications such as trachyonychia, superficial nail pitting, onychorrhexis, onychoschizia, idiopathic Beau’s lines, and longitudinal ridging with rewarding results.[3]
Gel nails can lead to allergic contact dermatitis due to acrylates present in the preparation. Freeman et al. reported four cases of contact allergy to acrylates with varied reactions, including nail fold, fingertip, and hand dermatitis and face and neck dermatitis.[26] In a case series, all patients were found positive on patch testing for HEMA and experienced resolution of dermatitis after removal of their acrylic nails or upon discontinuing work with acrylic gel nails.[27] Less frequent complications including paronychia, nail dystrophy, and onycholysis have also been reported.[27] Patients with known acrylate allergy should disclose this information to other medical personnel including dentists and orthopedic surgeons, to avoid potential adverse reactions to procedures other than nail procedures.
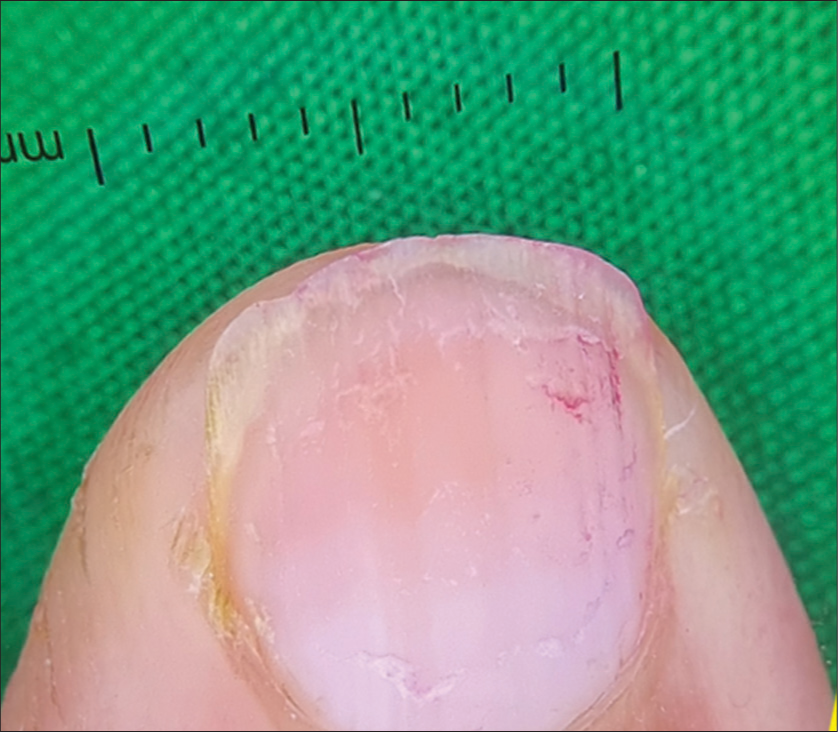
Psoriasiform onychodystrophy has been reported to be induced by photo-bonded nails.[28,29] The patients characteristically present with nail changes suggestive of psoriasis, including onycholysis, splinter hemorrhages, hyperkeratosis, and nail plate thinning [Figure 7]. However, these occur as a consequence of gel manicures. Over a period of time, as nails grow, the gel nails require in-fillings[Figure 8]. Since gel manicures and pedicures are on the rise, these changes are also more commonly reported, necessitating the formulation of recommendations to avoid these complications.
- Pseudo-psoriatic nail as seen on onychoscopy. The patient was not a known case of psoriasis. The onset of nail changes was seen after the usage of artificial nails (Dermlite DL4 Polarized ×10).

- Synthetic nail requiring in-fills at the proximal end.
Peripheral neuropathy is a relatively rare complication reported with the use of gel nails.[30] It may be associated with local neuropathy induced by methyl-methacrylate.[30] The use of ultraviolet light has been linked both with cutaneous malignancy and ocular toxicity. The use of ultraviolet A (UVA) lamps in curing gel nails is the step considered responsible for this. Diffey concluded that although the risk of inducing squamous cell carcinoma from exposure to UVA nail lamps is very low, it should be reduced further by wearing fingerless gloves on lamp exposure.[31] The scatter of light from the UV light unit onto the eyes has also raised concern regarding ocular toxicity. It may be prudent to use UV filter glasses to protect the eyes. Various important points to be kept in mind while performing gel nails to minimize the adverse effects associated with them are shown in Table 4.
|
UV: Ultraviolet
HEMA AND NAIL COSMETICS
HEMA is the most frequently reacting acrylate and is now considered to be an important cause of contact allergic dermatitis.[32] It is present in dental materials, glues, and printing inks and paints, apart from nail cosmetics. Previously, sensitized patients were more prone to the development of contact allergic dermatitis, including dental personnel, printers, and industry workers in contact with the glue.
HEMA has emerged consistently as the most sensitizing monomer, with HEMA allergic reactions affecting health professionals and users both. The majority of cases of contact allergic dermatitis to HEMA are related to cosmetic nail products including acrylic nails, gel nails, and long-lasting nail polish (gel lacquer) [Figure 9]. These are seen both in nail technicians (considered to be an occupational dermatosis) and in clients/women doing self-applications at home. This has necessitated stringent policies regarding the use of these chemicals in aesthetic procedures.[33] Due to a large number of patients reporting contact allergy to HEMA in nail cosmetics, the European Union restricted the use of HEMA in nail cosmetics in 2020, permitting it only for professional use. This meant that warnings like “For professional use only” and “Can cause an allergic reaction” were mandated on the package of nail products containing HEMA.[32]

- Finger-tip dermatitis in a nail salon worker.
NAIL COSMETICS AND HEALTHCARE WORKERS
It is well documented that chipped-off nail enamel and long artificial nails can harbor various organisms including Klebsiella, Pseudomonas, and Candida. These can get transmitted to patients since they are difficult to be washed with soap. Hence, the old chipped-off nail polish should be removed, and nails should be kept short by healthcare workers.[34]
NAIL COSMETICS AND NAIL TECHNICIANS
Nail technicians are exposed to a variety of occupational hazards at the workplace, due to their job profile. Thus, they form an important subset of patients presenting with adverse effects to nail cosmetics. Occupational hazards include those due to bad ergonomics as a large part of their time at work is spent in a bent position. In addition, there are safety hazards related to chemical, physical, and biological factors.
Ergonomics-wise, a nail salon worker or nail technician’s job entails sitting for prolonged periods, while bending and adopting awkward uncomfortable postures. They report more musculoskeletal injuries due to prolonged sitting and bending.[35] Neck, back, and hand/wrist pain are common symptoms in nail technicians.
Chemical exposure in nail technicians including exposure to formaldehyde, toluene, phthalates, and acrylates is a significant occupational hazard.[36,37] Respiratory diseases can occur from working in nail salons.[38]
Handling of sharp instruments may also result in pricks and punctures.
Infection is a common complication of nail cosmetics. The workers are also exposed to a variety of pathogens including fungi and bacteria from unsterile instruments and cuts and pricks from sharp instruments used in the performance of cosmetic nail procedures.[39]
Prevention of health hazards among nail salon workers requires efforts to increase knowledge and improve occupational health in nail salons.[35] Dissemination of education regarding workplace hazards and their impact reduction can go a long way in preventing such outcomes. Improved ergonomics can lead to an immediate improvement in their condition, going a long way in minimizing morbidity. It is important to focus on educating nail salon workers regarding the health hazards of chemical exposure, providing them with the right kind of gloves and ensuring good ventilation at the workplace. The nail technicians should also wear proper well-fitting masks and protective eyewear. At the worksite, there is inevitable contact with nail materials daily. It should be ensured that the tools and work surfaces are free from allergens. Extreme precautions should be taken while performing work to ensure that acrylates do not spread on skin or surrounding surface or equipment, as these can subsequently act as a source of exposure. Suuronen et al. performed a simplified penetration test to evaluate the suitability of disposable glove material to be used in nail salons for protection against methacrylates.[40] They concluded that neoprene was the best material for protection against gel nail products. Other materials were not found suitable for protection against acrylates which could penetrate through or even degrade the glove material very quickly. Disposable gloves should not be used for handling of acrylic nail liquids. Some uncommon adverse effects of nail cosmetics are shown in Table 5.
| Adverse effect | Responsible nail cosmetic | Responsible component |
|---|---|---|
| Desquamative gingivitis | Nail polish | Tosylamide/formaldehyde resin |
| Decreased sperm mobility and viability |
Nail polish | Dibutyl Phthalate |
| Withdrawal symptoms and acute renal failure when used as an addiction drug |
Nail polish remover | Gamma butyrolactone |
| Acute toxicity in infants | Nail polish remover | Gamma butyrolactone |
| Paresthesia | Sculptured acrylic nail | Acrylates |
| Respiratory complaints (Occupational)[41] |
Acrylic nail development | Acrylic resins |
| Effect on pulse oximeter readings[41] | Nail polish | Fingernails painted with black or brown nail paint showed a 2% decrease in the measurement of oxygen saturation |
| Neurological symptoms - Mild cognitive and neurosensory symptoms (Occupational) |
Nail cosmetic development | Solvents and methacrylates |
| Transmission of infections (Occupational) | Artificial nails and adornments | Artificial nails harbor bacteria that are difficult to remove by cleansing with antimicrobial soaps or alcohol-based gels. This can be hazardous In hospital settings. |
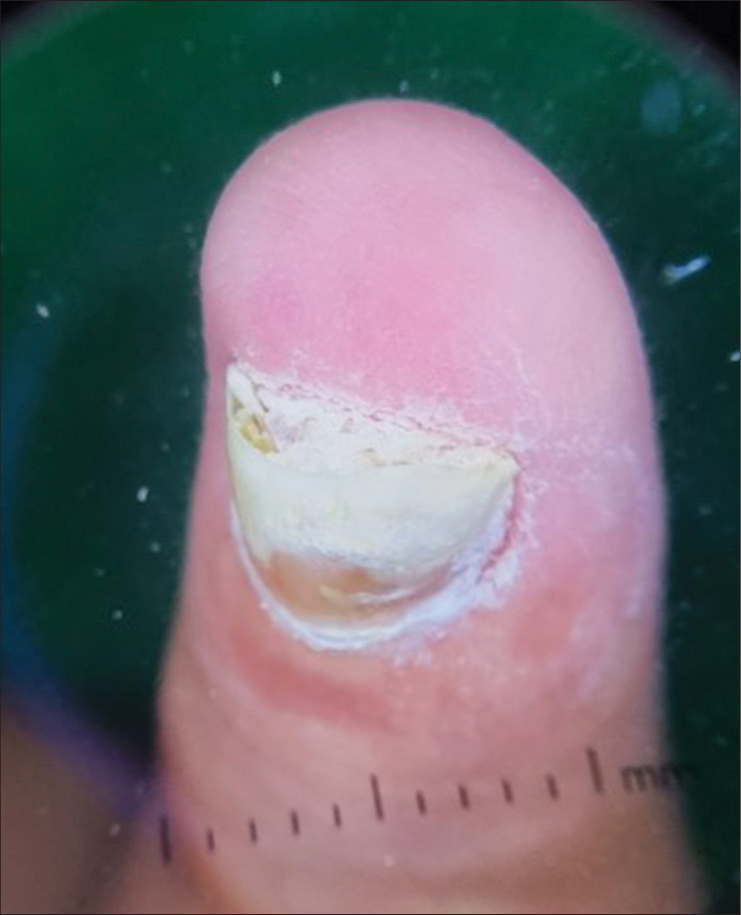
| Pterygium inversum unguis[42] [Figure 10a and b] | Gel nails | Nail fortifiers containing formaldehyde and acrylic nails and UV/LED gel polishes can be causative agents. |
UV: Ultraviolet, LED: Light-emitting diode
MANAGEMENT
Adverse events may occur during the nail grooming procedure or as an adverse reaction to individual components of nail cosmetics. It is important to have an understanding of the adverse effects and their management. These include acute toxicity, paresthesiae and neurological complaints, respiratory complaints, and pterygium inversum [Figure 10]. [41,42] The management approach is shown in Table 6.
- (a and b) Pterygium inversum unguis due to gel nails. The patient had no other skin lesions, tightening of skin, or any other predisposing factors.
| Adverse effect | Cause | Management |
|---|---|---|
| Onychoschizia | Repeated and/or prolonged nail polish application | Do not leave nail polish for more than two weeks |
| Keratin staining/Keratin granulation/ Pseudo-leukonychia |
||
| Paronychia, infections (bacterial, fungal, viral) |
Non-sterile instruments | Use sterile instruments and if possible, disposable ones. |
| Nail staining | Nail pigment is dissolved rather than suspended |
Avoid repeated use of nail polish, avoid deep colors, especially red |
| Nail plate fracture | Occurs with shellac nail gel during removal |
There are reduction in chances of nail plate damage |
| Onycholysis | Seen with gel nails, due to a strong bond formed between etched nail plate and acrylic |
Avoid deep etching of nail plate, both physical and chemical |
| Discolored yellow thin nail | Seen after nail sculpturing with shellac gel nail he natural nail plate gets damaged after 2–4 months of wear |
Avoid wearing sculptured nails for more than three months Ensure a gap of one month in between application of subsequent gel nails |
| Allergic contact dermatitis | Various allergens as discussed in text | Use of hypoallergenic products Avoidance in cases with known hypersensitivity |
| Burns | Methacrylate’s if spilled | Careful handling Adequate training of staff |
| Nail matrix damage | Improper technique of artificial nail application with liquid acrylic entering underneath the proximal nail fold |
|
| UV light related concerns | UV exposure in curing lamps | Wearing of nitrile gloves, sunscreens |
UV: Ultraviolet
CONCLUSION
The field of nail aesthetics is fast expanding and improvising to meet the increasing demand of consumers worldwide. Nail cosmetics are considered to be relatively safe; however, they can lead to significant contact allergic or irritant dermatitis, infections, and nail damage. Therefore, awareness regarding their clinical presentations, techniques and materials used in the nail cosmetic industry, and viable management options, is absolutely essential for dermatologists to educate and promote safe nail cosmetics in patients and manage complications.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Self-cosmetic care during the COVID-19 pandemic and its psychological impacts: Facts behind the closed doors. J Cosmet Dermatol. 2021;20:3093-7.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of gel nails in improving the appearance of cosmetically disfigured nails: Experience with 25 cases. J Cutan Aesthet Surg. 2014;7:26-31.
- [CrossRef] [PubMed] [Google Scholar]
- Nail cosmetics: What a dermatologist should know! Indian J Dermatol Venereol Leprol. 2023;29:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Review of the literature on the efficacy and safety of a new cosmetic topical treatment containing Pistacia lentiscus and hyaluronic acid for the treatment of nail plate damages. J Cosmet Dermatol. 2022;21:5514-8.
- [CrossRef] [PubMed] [Google Scholar]
- Side effects of gel nail polish: A systematic review. Clin Dermatol. 2022;40:706-15.
- [CrossRef] [PubMed] [Google Scholar]
- Cosmetically Induced disorders of the nail with update on contemporary nail manicures. J Clin Aesthet Dermatol. 2016;9:39-44.
- [Google Scholar]
- Nail cosmetics. Indian J Dermatol Venereol Leprol. 2012;78:309-17.
- [CrossRef] [PubMed] [Google Scholar]
- Onychoscopy In: Grover C, Relhan V, Nanda S, Bansal S, eds. NSI textbook of onychology (1st ed). Delhi: Evangel Publishing; 2021. p. :73-93.
- [Google Scholar]
- Leukonychia: What can white nails tell us? Am J Clin Dermatol. 2022;23:177-93.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency and main sites of allergic contact dermatitis caused by nail varnish. Dermatitis. 2008;19:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Nail cosmetics In: Rich P, Scher R, eds. An atlas of diseases of the nail (1st ed). New York, NY: Parthenon Publishing; 2003. p. :97-100.
- [CrossRef] [Google Scholar]
- A series of four cases of allergic contact dermatitis to phthalic anhydride/trimellitic anhydride/glycols copolymer in nail varnish. Contact Dermatitis. 2005;53:63-4.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic contact cheilitis from D and C Yellow 11. Contact Dermatitis. 2009;60:294-5.
- [CrossRef] [PubMed] [Google Scholar]
- Allergy to hypoallergenic nail polish: Does this exist? An Bras Dermatol. 2017;92:421-2.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis due to artificial nails. J Eur Acad Dermatol Venereol. 2008;22:998-1000.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of heavy metals and risk assessment in nail cosmetics sold in Seoul, Korea. Cut Ocular Tox. 2023;42:131-6.
- [CrossRef] [PubMed] [Google Scholar]
- Colored nail cosmetics and hardeners In: Draelos ZD, ed. Cosmetic dermatology products and procedures. Hoboken, NJ: Wiley-Blackwell; 2010. p. :206-13.
- [CrossRef] [Google Scholar]
- Cosmetic prostheses as artificial nail enhancements In: Draelos ZD, ed. Cosmetic dermatology products and procedures. Hoboken, NJ: Wiley-Blackwell; 2010. p. :215-21.
- [CrossRef] [Google Scholar]
- Nail cosmetics in nail disorders. J Cosmetic Dermatol. 2007;6:53-8.
- [CrossRef] [PubMed] [Google Scholar]
- Contact allergy caused by acrylates in nail cosmetics: A pilot study from Greece. Contact Dermatitis. 2024;90:273-9.
- [CrossRef] [PubMed] [Google Scholar]
- Presence of 2-hydroxyethyl methacrylate (HEMA) and other (meth) acrylates in nail cosmetics, and compliance with EU legislation: An online market survey. Contact Dermatitis. 2024;90:60-5.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of gel nails in improving the appearance of cosmetically disfigured nails: Experience with 25 cases. J Cutan Aesthet Surg. 2014;7:240-1.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse contact reactions to sculptured acrylic nails: 4 case reports and a literature review. Contact Dermatitis. 1995;33:381-5.
- [CrossRef] [PubMed] [Google Scholar]
- Sensitization to acrylates is a common adverse reaction to artificial fingernails. J Eur Acad Dermatol Venereol. 2007;21:169-74.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasiform onychodystrophy induced by photobonded acrylic nails. J Clin Aesthet Dermatol. 2020;13:18-20.
- [Google Scholar]
- Severe onychodystrophy due to allergic contact dermatitis from acrylic nails. Skin Appendage Disord. 2015;1:91-4.
- [CrossRef] [PubMed] [Google Scholar]
- Local neurotoxicity of methylmethacrylate monomer. Toxicol Lett. 1983;18:111-4.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of squamous cell carcinoma in women from exposure to UVA lamps used in cosmetic nail treatment. Br J Dermatol. 2012;167:1175-8.
- [CrossRef] [PubMed] [Google Scholar]
- 2-hydroxyethyl methacrylate (HEMA): A clinical review of contact allergy and allergic contact dermatitis-Part 1. Introduction, epidemiology, case series and case reports. Contact Dermatitis. 2023;89:401-33.
- [CrossRef] [PubMed] [Google Scholar]
- Acrylates as a significant cause of allergic contact dermatitis: New sources of exposure. Postepy Dermatol Alergol. 2021;38:555-60.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial carriage on the fingernails of OR nurses. AORN J. 1994;60:796, 799-805
- [CrossRef] [PubMed] [Google Scholar]
- Health and safety in nail salons: A cross-sectional survey. Ann Work Expo Health. 2021;65:225-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acrylate contact allergy: Patient characteristics and evaluation of screening allergens. Dermatitis. 2011;22:98-101.
- [CrossRef] [Google Scholar]
- Perceived work exposures and expressed intervention needs among Michigan nail salon workers. Int Arch Occup Environ Health. 2021;94:2001-13.
- [CrossRef] [PubMed] [Google Scholar]
- Screening survey of ocular, nasal, respiratory and skin symptoms in manicurists in Poland. Int J Occup Med Environ Health. 2017;30:887-96.
- [CrossRef] [PubMed] [Google Scholar]
- Nail cosmetics: A dermatological perspective. Clin Exp Dermatol. 2019;44:599-605.
- [CrossRef] [PubMed] [Google Scholar]
- Acrylates in artificial nails-Results of product analyses and glove penetration studies. Contact Dermatitis. 2023;90:266-72.
- [CrossRef] [PubMed] [Google Scholar]
- Nail cosmetics: Potential hazards. J Am Acad Dermatol. 2007;57:1069-70.
- [CrossRef] [PubMed] [Google Scholar]
- Pterygium inversum unguis secondary to gel polish. J Eur Acad Dermatol Venereol. 2018;32:160-3.
- [CrossRef] [PubMed] [Google Scholar]






