Translate this page into:
A rare case of Hansen’s disease masquerading as granuloma annulare

*Corresponding author: Dr. Shikha Thakur, Department of Dermatology and Sexually Transmitted Diseases, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India. shikha.b.thakur@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mousum SA, Thakur S, Dey B. A rare case of Hansen’s disease masquerading as granuloma annulare. CosmoDerma. 2025;5:20. doi: 10.25259/CSDM_201_2024
Abstract
Leprosy, a chronic granulomatous infection caused by Mycobacterium leprae, is prevalent in India and often misdiagnosed due to its variable cutaneous presentations. Granuloma annulare (GA), a benign dermatosis characterized by annular papules and plaques, requires clinicopathological correlation for diagnosis. Rarely, leprosy mimics GA in its presentation. Here, we report a 65-year-old male with a two-year history of multiple circumscribed skin-colored to erythematous annular plaques on the upper arms and back, initially suspected as GA due to the absence of sensation and nerve impairment but was later diagnosed as a case of Hansen’s disease based on histopathological findings.
Keywords
Fite-Faraco stain
Granuloma annulare
Hansen disease
Leprosy
INTRODUCTION
Leprosy, or Hansen’s disease, is a chronic granulomatous infection caused by the acid-fast bacilli (AFB) Mycobacterium leprae. This bacterium is an obligate intracellular pathogen that prefers cooler areas of the body, such as the skin, and commonly infects Schwann cells.[1] Granuloma annulare (GA) is a benign cutaneous disorder that typically presents as annular groups of skin-colored to erythematous papules, usually on the dorsum of hands and feet. Diagnosis relies on clinicopathological correlation.[2] There are few case reports where leprosy has presented with cutaneous lesions similar to GA.[3]
CASE REPORT
A 65-year-old male patient presented with multiple well-circumscribed skin-colored to erythematous annular plaques which were first noticed over both upper arms two years back and which gradually progressed to involve the back for the past six months. There was no history of itching, pain, or loss of sensation. Physical examination revealed multiple non-scaly annular plaques with central clearing and micro papules along the periphery, without loss of sensation or enlarged peripheral nerves [Figure 1].
GA was considered clinically. However, given the high prevalence of leprosy in India and previous instances of leprosy manifesting as GA-like skin lesions, a skin biopsy was performed keeping both GA and Hansen’s disease as differentials.

- A 65-year-old male patient presented with multiple well-circumscribed skin-colored to erythematous annular plaques over the (a) arms and (b) back. The lesions showed central clearing and micropapules along the periphery.
Biopsy revealed epithelioid granuloma in the dermis without any Langhan’s giant cells and lymphocytes [Figure 2] and Fite-Faraco stain demonstrated positive bacilli (bacillary index 1+) [Figure 3]. Lack of palisaded histiocytic granulomas within the reticular dermis and positive Fite-Faraco stain with a bacteriological index of 1+ confirmed the diagnosis as Hansen’s in the tubercular pole. The patient is currently being treated with multibacillary multidrug therapy as per national leprosy eradication program (NLEP) guidelines for multibacillary leprosy.
![(a) Histopathology low power view showing epithelioid granulomas in the dermis [Hematoxylin and Eosin (H&E), ×10]. (b) Histopathology high-power view showing dermal epithelioid granulomas with lymphocytes with occasional Langhan’s giant cell (H&E, ×40).](/content/130/2025/5/1/img/CSDM-5-20-g002.png)
- (a) Histopathology low power view showing epithelioid granulomas in the dermis [Hematoxylin and Eosin (H&E), ×10]. (b) Histopathology high-power view showing dermal epithelioid granulomas with lymphocytes with occasional Langhan’s giant cell (H&E, ×40).
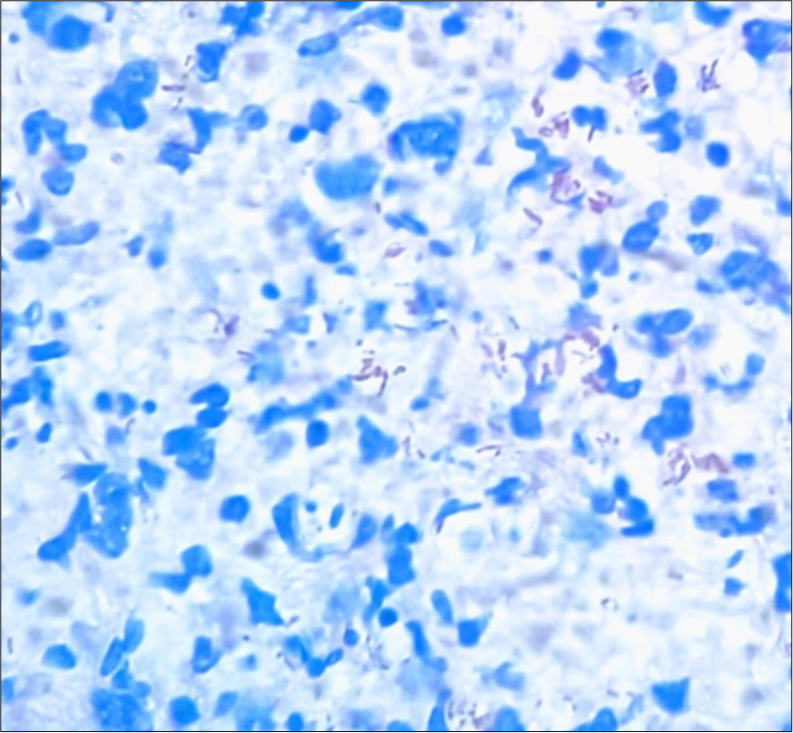
- Fite-Faraco stain demonstrating scattered acid-fast bacilli with bacillary index of 1+ (FiteFaraco stain, ×40).
DISCUSSION
Although India officially declared leprosy eradicated in 2005, having reduced its prevalence rate to 0.72/10,000, the disease has resurfaced with high intensity in several states. India currently has the highest number of leprosy cases worldwide, followed by Brazil and Indonesia.[4]
The Ridley-Jopling classification system categorizes leprosy into five subtypes: Tuberculoid (TT), borderline tuberculoid (BT), borderline, borderline lepromatous, and lepromatous leprosy (LL). These are based on clinical presentation, histopathological findings, and host immunologic status.[5] At one end of the spectrum, TT leprosy is marked by a small number of well-defined, anesthetic, hypopigmented, or erythematous patches, often accompanied by enlargement of peripheral nerves. Biopsies from these lesions reveal well-organized dermal epithelioid granulomas with a surrounding layer of lymphocytes, typically arranged in periadnexal and perineural patterns. Due to a strong cell-mediated immune response, AFB are generally absent on histochemical staining. Conversely, at the other end of the spectrum, LL is characterized by widespread, symmetrical erythematous, and copper-colored plaques and nodules, alongside peripheral neuropathy that follows a stocking-and-glove distribution. Histological examination shows diffuse infiltration of foamy macrophages and plasma cells, with few lymphocytes, no giant cells, and numerous AFB present within the nerves.[6] In between the two polar subtypes, BT leprosy presents similar to TT, with few to many annular erythematous plaques with central hypopigmentation and associated anesthesia.[5] On histopathology, perineural granulomas and Langhans giant cells surrounded by lymphocytes or poorly organized “immature” granulomas may be observed. Histochemical staining typically reveals few organisms within Schwann cells of peripheral nerve fibers in the dermis. In between the two polar subtypes, BT leprosy presents similar to TT, with few to many annular erythematous plaques with central hypopigmentation and associated anesthesia.[6]
GA, on the other hand, is a chronic skin condition characterized by the formation of annular or ring-shaped lesions. These lesions are typically asymptomatic, skin-colored to erythematous, and may appear on various parts of the body, most commonly on the hands and feet. The exact cause of GA is unknown, but it is thought to be related to immune system dysfunction.[7] Histologically, GA is characterized by focal degeneration of collagen with surrounding palisaded granulomas. While GA is generally a self-limiting condition, it can persist for years and may be resistant to treatment, often requiring a biopsy for a definitive diagnosis to differentiate it from other granulomatous diseases.[2]
Our patient’s clinical presentation of annular plaques without sensory loss or peripheral nerve enlargement, combined with biopsy findings of epithelioid granulomas and positive bacilli, led to a diagnosis of BT Hansen’s disease. The imperfect correlation between clinical and histological features in leprosy is well acknowledged, with up to one-third of BT cases showing no alignment with the Ridley-Jopling classification.[6]
Similar cases have reported leprosy presenting with lesions resembling GA, as depicted in Table 1.
| Study | Patient presentation | Histopathological findings | Diagnosis | Key findings |
|---|---|---|---|---|
| Zhu et al.[3] | Multiple non-scaly annular plaques, some with clearing | Palisaded and interstitial granulomatous infiltrate, necrobiotic collagen, Langhans giant cells, lymphocytes, and plasma cells | Borderline Tuberculoid Leprosy | Clinical lesions similar to GA and positive Fite stain revealed AFB |
| Longmire et al.[8] | Elongated granulomas surrounding cutaneous nerves | Perineural granuloma | Granuloma Annulare | Perineural granulomas were observed, raising suspicion of leprosy |
| Current Case | Annular plaques with central clearing, micropapules | Epithelioid granulomas without Langhans giant cells, lymphocytes, and positive bacilli on Fite-Faraco stain | Borderline Tuberculoid Hansen’s | Clinical mimicry of GA confirmed as leprosy with positive Fite-Faraco stain |
GA: Granuloma annulare, AFB: Acid-fast bacilli.
CONCLUSION
This case highlights an unusual presentation of leprosy mimicking GA with histopathology as a cornerstone for accurate diagnosis. The use of Fite-Faraco staining was instrumental in distinguishing Hansen’s disease from GA in this case, highlighting the need for clinicopathological correlation in endemic regions. Dermatologists and dermatopathologists should remain vigilant and use histochemical staining for confirmation as early and accurate diagnosis ensures timely treatment and better patient outcomes.
Ethical approval:
The Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- Tuberculosis and leprosy: Classical granulomatous diseases in the twenty-first century. Dermatol Clin. 2015;33:541-62.
- [CrossRef] [PubMed] [Google Scholar]
- Granuloma annulare: An updated review of epidemiology, pathogenesis, and treatment options. Am J Clin Dermatol. 2022;23:37-50.
- [CrossRef] [PubMed] [Google Scholar]
- Borderline tuberculoid leprosy masquerading as granuloma annulare: A clinical and histological pitfall. Am J Dermatopathol. 2017;39:296-9.
- [CrossRef] [PubMed] [Google Scholar]
- Leprosy in the 21st century. Clin Microbiol Rev. 2015;28:80-94.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of leprosy according to immunity. A five-group system. Int J Lepr Other Mycobact Dis. 1966;34:255-73.
- [Google Scholar]
- Clinico-histopathological correlation in Hansen's disease: A retrospective study. Int J Clin Diagn Pathol. 2020;3:168-72.
- [CrossRef] [Google Scholar]
- Nerve Involvement in granuloma annulare. J Cutan Med Surg. 2012;16:428-32.
- [CrossRef] [PubMed] [Google Scholar]






