Translate this page into:
Role of dermoscopy in differentiating seborrheic dermatitis of scalp and scalp psoriasis

*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, Maulana Azad Medical College, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Bahadur A, Tyagi H. Role of dermoscopy in differentiating seborrheic dermatitis of scalp and scalp psoriasis. CosmoDerma. 2024;4:80. doi: 10.25259/CSDM_101_2024
Dear Sir,
Dermoscopy has emerged as a crucial tool in dermatology, providing a non-invasive technique to enhance diagnostic accuracy. Its utility is particularly pronounced in distinguishing seborrheic dermatitis (SD) (seborrheic capitis), scalp psoriasis, and sebopsoriasis, three prevalent inflammatory scalp disorders that often exhibit overlapping clinical features. By revealing distinct vascular and scaling patterns, dermoscopy helps clinicians in differentiating these disorders.[1] This non-invasive method also allows for the monitoring of disease progression and response to treatment, reducing the need for biopsies.
SD is a chronic, relapsing inflammatory condition that predominantly affects areas rich in sebaceous glands, such as the scalp, face, and upper trunk. Clinically, it manifests as ill-defined plaques with greasy, yellowish scales with or without erythema [Figure 1]. Pruritus is a common symptom, and the condition often flares in response to stress or changes in weather.[2] Conversely, scalp psoriasis is a chronic, immune-mediated disorder characterized by well-demarcated, and erythematous plaques with silvery scales [Figure 2]. It frequently involves the scalp and can extend beyond the hairline, forming what is known as the “corona” or “crown” of psoriasis (corona psoriatica). Psoriasis may also be associated with nail changes and psoriatic arthritis. Sebopsoriasis, a condition that shares features of both SD and psoriasis, presents with well-demarcated erythematous plaques covered with greasy scales, often localized to seborrheic areas. Clinically, it can be challenging to differentiate from the other two conditions due to the overlapping presentation of greasy scales and erythematous plaques.[3]
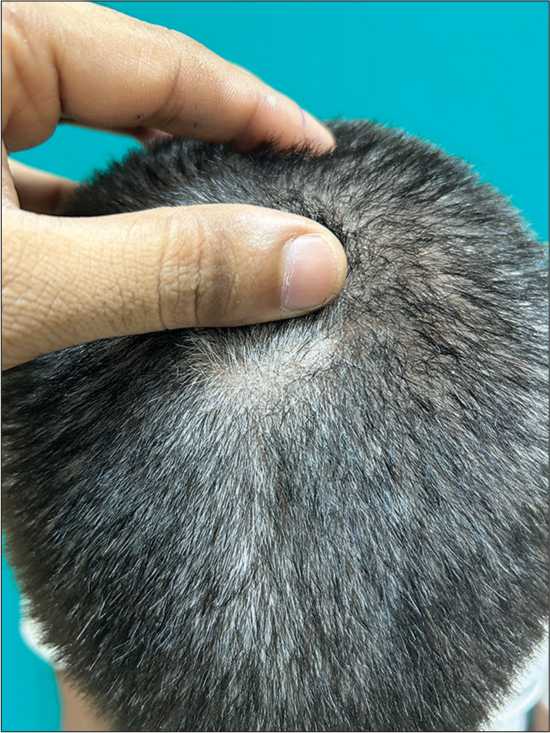
- Ill-defined plaques of seborrheic dermatitis with greasy, yellowish scales over the vertex in a 50-year-old male.

- Well-demarcated, erythematous plaques of psoriasis with silvery scales over the vertex in a 40-year-old male.
Dermoscopy, by enhancing the visualization of surface and subsurface skin structures, reveals specific patterns that are useful in distinguishing SD from scalp psoriasis. In SD, dermoscopy typically shows a yellowish background due to sebaceous activity, with fine greasy, yellow scales [Figure 3]. The vascular pattern often consists of arborizing and dotted vessels on an erythematous background [Figure 4], accompanied by fine, yellowish “ring-like” structures around hair follicles.[4] In contrast, scalp psoriasis under dermoscopy reveals a red background indicative of marked inflammation, with thick, white, or silvery scales [Figure 5]. The vascular pattern is characterized by dotted vessels regularly distributed over the lesion, creating a “red dots” appearance [Figure 6]. In addition, the Auspitz sign, where the removal of scales leads to pinpoint bleeding, is observed under dermoscopy as red dots or globules. Sebopsoriasis shares dermoscopic features with both conditions. It may display a yellowish background with greasy scales similar to SD, but also exhibits the red background and dotted vessels seen in psoriasis. This combination of features can be helpful in diagnosing sebopsoriasis, though it underscores the need for a comprehensive clinical evaluation. Kibar et al., investigated the use of trichoscopy to distinguish between scalp psoriasis and SD. The study involved 31 patients with scalp psoriasis and 112 patients with SD, with trichoscopic findings compared against healthy individuals and other non-scarring alopecias. The results highlighted specific trichoscopic patterns: psoriasis was characterized by atypical red vessels, red dots and globules, signet ring vessels, structureless red areas, and hidden hairs, while SD showed more twisted red loops and comma vessels [Figures 4 and 6]. The study introduced hidden hairs and signet ring vessels as new indicators for psoriasis and identified comma vessels as specific to SD, demonstrating that trichoscopy is a useful tool for differentiating these scalp conditions. The initial dermal histopathological changes in psoriasis are often non-specific, eventually leading to the development of dilated and slightly twisted blood vessels within the dermal papillae. This “signet ring vessel” sign is believed to result from these vascular changes in both psoriasis and SD. The signet ring shape is thought to be created by a slightly twisted glomerular vessel and its elongated, dilated ring-shaped vessel. Both psoriasis and SD result in epidermal and perifollicular inflammation, making the proximal hair shaft appear hidden beneath white-gray epidermal proliferation contributing to the appearance of hidden hair under trichoscopy.[4] In another study, researchers analyzed 12 patients using trichoscopic and direct microscopic examinations, assessing known SD trichoscopic signs and their correlation with Malassezia presence on the scalp. They identified three new signs: The “dandelion” vascular conglomerate, the “cherry blossom” vascular pattern, and intrafollicular oily material. Notably, the “dandelion” vascular conglomerate was the only sign correlating with Malassezia colonization. The study suggests these trichoscopic signs can help indirectly determine fungal colonization in SD.[5]
![Non-polarized dermoscopy [Heine DELTAone] showing fine greasy yellowish-white scales of seborrheic dermatitis (×20).](/content/130/2024/4/1/img/CSDM-4-80-g003.png)
- Non-polarized dermoscopy [Heine DELTAone] showing fine greasy yellowish-white scales of seborrheic dermatitis (×20).
![Polarized dermoscopy [Heine DELTAone] showing arborizing (yellow arrows), comma (navy blue arrows) and dotted vessels (green circle) on an erythematous background in seborrheic dermatitis (×20).](/content/130/2024/4/1/img/CSDM-4-80-g004.png)
- Polarized dermoscopy [Heine DELTAone] showing arborizing (yellow arrows), comma (navy blue arrows) and dotted vessels (green circle) on an erythematous background in seborrheic dermatitis (×20).
![Non-polarized dermoscopy [Heine DELTAone] showing thick, white-silvery scales of psoriasis (×20).](/content/130/2024/4/1/img/CSDM-4-80-g005.png)
- Non-polarized dermoscopy [Heine DELTAone] showing thick, white-silvery scales of psoriasis (×20).
![Polarized dermoscopy [Heine DELTAone] showing atypical red vessels (purple arrows), red dots (black arrows) and globules (navy blue circles), signet ring vessels (navy blue arrows), glomeruloid vessels (sky blue arrows), twisted red loop (yellow arrow), and hidden hairs (green arrows) in psoriasis (×20).](/content/130/2024/4/1/img/CSDM-4-80-g006.png)
- Polarized dermoscopy [Heine DELTAone] showing atypical red vessels (purple arrows), red dots (black arrows) and globules (navy blue circles), signet ring vessels (navy blue arrows), glomeruloid vessels (sky blue arrows), twisted red loop (yellow arrow), and hidden hairs (green arrows) in psoriasis (×20).
Histopathologically, SD shows mild acanthosis, parakeratosis, and spongiosis in the epidermis. The dermis features perivascular and perifollicular inflammatory infiltrate, predominantly lymphocytes, and histiocytes, with the presence of Malassezia species in the stratum corneum. Scalp psoriasis, on the other hand, is characterized by marked acanthosis, parakeratosis, and the absence of the granular cell layer in the epidermis. The dermis shows dilated blood vessels in the papillary dermis, with an influx of neutrophils forming Munro microabscesses and regular elongation of rete ridges. Sebopsoriasis histopathology can reveal overlapping features of both SD and psoriasis, including mild acanthosis and parakeratosis, with a mixed inflammatory infiltrate that may include neutrophils, akin to Munro microabscesses.[6]
The dermoscopic examination provides a bridge between clinical assessment and histopathological analysis, enabling immediate differentiation. Furthermore, dermoscopy serves as an educational tool for both clinicians and patients, improving understanding and compliance with treatment regimens.
In conclusion, dermoscopy plays an essential role in the differential diagnosis of SD, scalp psoriasis, and sebopsoriasis. By providing a clear view of underlying vascular and scaling patterns, dermoscopy enhances diagnostic precision, guiding appropriate treatment strategies, long-term management, and monitoring of these common scalp disorders, thus improving patient outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopy can be useful in differentiating scalp psoriasis from seborrhoeic dermatitis. Br J Dermatol. 2011;164:652-6.
- [CrossRef] [PubMed] [Google Scholar]
- Scalp seborrheic dermatitis: What we know so far. Skin Appendage Disord. 2023;9:160-4.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and trichoscopic features in various forms of scalp psoriasis. J Eur Acad Dermatol Venereol. 2021;35:1830-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic findings in scalp psoriasis and seborrheic dermatitis; two new signs; signet ring vessel and hidden hair. Indian J Dermatol. 2015;60:41-5.
- [CrossRef] [PubMed] [Google Scholar]
- Seborrheic dermatitis: Three novel trichoscopic signs and its correlation to Malassezia sp. colonization. Skin Appendage Disord. 2019;5:288-2.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological differential diagnosis of psoriasis and seborrheic dermatitis of the scalp. Ann Dermatol. 2016;28:427-32.
- [CrossRef] [PubMed] [Google Scholar]






