Translate this page into:
Zosteriform lichen planus: An uncommon presentation of a common condition

*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, Maulana Azad Medical College, Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Patel V, Yadav D. Zosteriform lichen planus: An uncommon presentation of a common condition. CosmoDerma. 2024;4:68. doi: 10.25259/CSDM_75_2024
Dear Sir,
Zosteriform lichen planus (ZLP) is an uncommon variant of lichen planus (LP), characterized by lesions that follow a dermatomal distribution, mimicking herpes zoster without an association with varicella-zoster virus infection.[1] We report the clinical, dermoscopic, and histologic features of ZLP in an adult male.
A 40-year-old male presented with multiple pruritic, pigmented papules on the right side of his abdomen for five months. He had no history of herpes zoster, and hepatitis B and C screenings were negative. There was no family history of verrucous epidermal nevus or other linear lesions. Cutaneous examination revealed violaceous, polygonal, pruritic papules, and coalescent plaques along with brown atrophic papules in a zosteriform distribution involving the right T12-S1 dermatome, extending from the lower lateral back to the inguinal area [Figure 1a]. Koebner phenomenon was seen without any involvement of oral or genital mucosa, nails, or the scalp. A closer examination revealed multiple Wickham striae [Figure 1b]. Polarized dermoscopy showed Wickham striae along with pigment globules [Figure 2]. Histopathological examination revealed mild hypergranulosis and a dense band-like lymphohistiocytic infiltrate in the papillary dermis, with colloid bodies and marked pigment incontinence [Figure 3]. The patient was treated with betamethasone dipropionate 0.05% cream twice daily application and oral levocetirizine 5 mg tablet before sleep for three weeks resulting in improvement in pruritus and partial resolution of lesions.
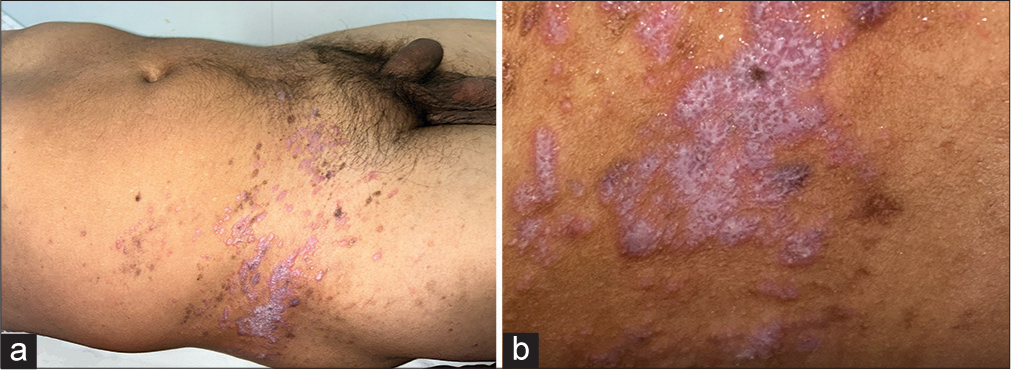
- (a) Violaceous, polygonal, pruritic papules, and coalescent plaques along with brown atrophic papules in a zosteriform distribution involving the right T12-S1 dermatome, extending from the lower lateral back to the inguinal area. (b) A closer examination showing multiple Wickham striae.
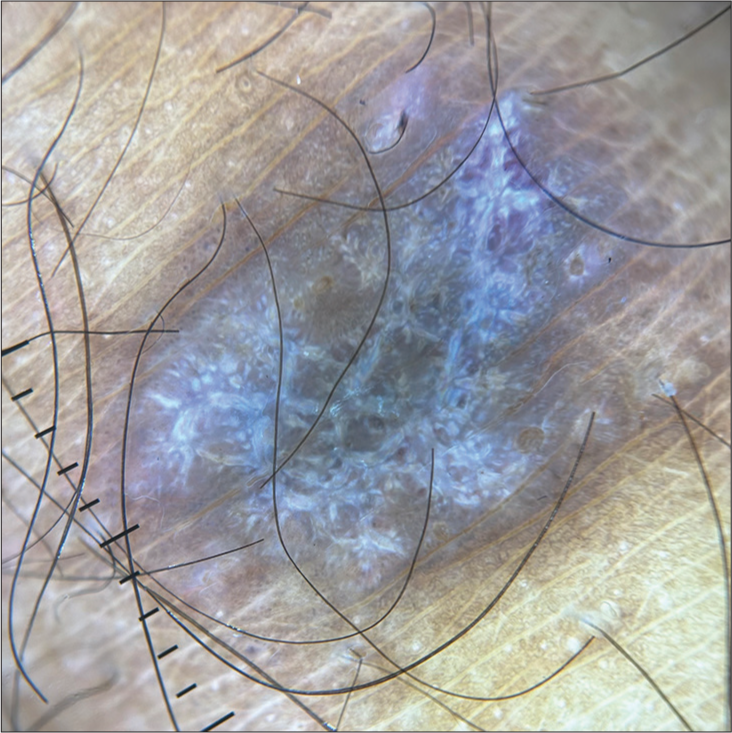
- Polarized dermoscopy showing Wickham striae along with pigment globules (Illuco IDS-1100, ×20).
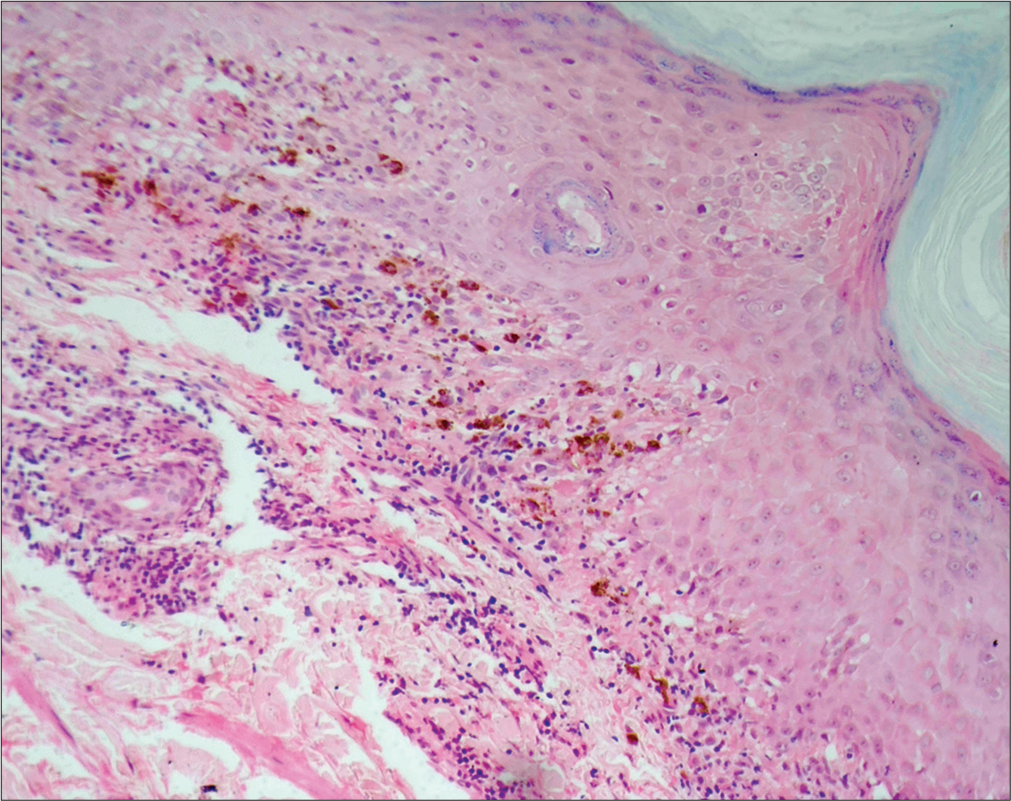
- Mild hypergranulosis and band-like lymphocytic infiltrates in the papillary dermis, with colloid bodies and significant pigment incontinence (H and E; ×10).
The majority of cases of ZLP have been reported in males, particularly between the ages of 30 and 40 years. In most cases, lesions appear on the left side of the body.[1-3] However, there are reports of cases involving females and the right side of the body as well.[3] Clinically, ZLP presents as pruritic, erythematous to hyperpigmented papules that follow a dermatomal distribution. Unlike typical herpes zoster, ZLP may involve multiple non-contiguous dermatomes. Lesions are often grouped in a band-like pattern, resembling herpes zoster but without a history of varicella-zoster virus infection.[1,2] The ZLP can involve the oral mucosa, as noted in the case of a 20-year-old female with hyperpigmented patches in a lacy pattern over the buccal mucosa. Nail, scalp, and genital involvements are typically absent.[3] Few cases report associations with other diseases. One reported case had a history of extracorporeal shock wave lithotripsy for renal colic.[3] There are no strong links to systemic diseases. Dermoscopic examination of ZLP typically reveals features similar to those of LP, including Wickham’s striae and a network of whitish lines over a violaceous background. However, specific dermoscopic findings exclusive to ZLP are not well-documented in the literature.[1-3] Histopathological examination of ZLP lesions reveals features typical of LP, including focal mild acanthosis, hypergranulosis, band-like lymphocytic infiltrate in the upper dermis, disruption of the dermo-epidermal junction, and pigment incontinence. These findings help differentiate ZLP from other dermatoses.[1,2]
Several hypotheses have been proposed for the occurrence of ZLP, including Koebner’s phenomenon, Wolf’s isotopic response, and de novo emergence along Blaschko’s lines. Some authors suggest that ZLP lesions are neural in origin, whereas others believe that ZLP occurs primarily in cases following herpes zoster infections.[2,3] Diagnosis of ZLP is clinical, supported by histopathology. Differential diagnoses include linear LP, lichen striatus/blaschkitis, and linear psoriasis [Table 1].[4-7] A thorough history and examination are crucial to rule out varicella-zoster virus infection and other conditions.[1,3] Treatment options for ZLP are similar to those for LP and include topical corticosteroids, topical salicylic acid, and systemic antihistamines. In refractory cases, systemic or intralesional corticosteroids may be used. The goal is to reduce inflammation and control symptoms rather than to cure the disease, as spontaneous remission is possible.[1,3] The prognosis for ZLP is generally good, with many patients experiencing a resolution of symptoms over time. However, hyperpigmentation and residual skin changes can persist. Regular follow-up is necessary to monitor for potential recurrence or complications.[2,3]
| Feature | Zosteriform Lichen Planus | Blaschkolinear Lichen Planus | Lichen Striatus/Blaschkitis | Linear Psoriasis |
|---|---|---|---|---|
| Presentation | Lichen planus lesions following a dermatomal distribution | Lichen planus characterized by linear lesions following Blaschko’s lines | Linear arrangement of lichenoid papules along Blaschko’s lines; typically unilateral | Psoriasis with lesions arranged in a linear or band-like distribution |
| Age of Onset | More commonly reported in adults, particularly between the ages of 30 and 40 years | Can occur at any age, though more common in adults | Typically presents in children, often before 16 years of age | Usually presents in adults, but can occur at any age |
| Gender Predilection | Slight male predominance was noted in reported cases | No significant gender predilection | No gender predilection reported | Slight male predominance |
| Common Sites | Typically appears on the trunk or extremities following a dermatome | Can appear on any part of the body following Blaschko’s lines | Usually involves the trunk or limbs unilaterally | Commonly involves the extensor surfaces |
| Clinical Presentation | Pruritic, erythematous to violaceous papules and plaques arranged in a zosteriform (dermatomal) pattern | Pruritic, erythematous to violaceous papules and plaques arranged linearly | Linear arrangement of small, flat-topped, flesh-colored, or pink papules | Erythematous plaques with silvery scales, often linear or band-like |
| Hypothesized Pathogenesis | Hypotheses include Koebner’s phenomenon, Wolf’s isotopic response, neural mechanisms, or post-herpetic inflammatory response | Thought to arise from genetic mosaicism or inflammatory processes along Blaschko’s lines | Possibly due to a genetic or acquired mosaic disorder affecting keratinization | Thought to involve genetic predisposition and environmental triggers |
| Dermoscopy | Similar findings to linear/blaschkoid LP, but specific dermoscopic features for ZLP not well documented | Wickham’s striae, a network of whitish lines over a violaceous background | Gray granular pigmentations and a white scar-like line with mild scales on the flesh-colored background | Regular arrangement of red dots, glomerular vessels, and white scales |
| Histopathology | Similar to classic lichen planus, with hypergranulosis, acanthosis, basal cell degeneration, and a band-like lymphocytic infiltrate | Similar to classic lichen planus along with deeper infiltrates along appendages | Lichenoid inflammation along with deeper infiltrates along appendages | Hyperkeratosis, alternating parakeratosis, regular acanthosis, elongated rete ridges, and dilated blood vessels in dermal papillae |
| Extracutaneous Involvement | Rarely involves mucous membranes; primarily cutaneous with few reports of oral involvement | Can involve mucous membranes, nails, and scalp in some cases | Primarily cutaneous; mucous membrane involvement rare | Typically limited to the skin, but psoriatic arthritis may occur in some cases |
| Associated Diseases | Few associations were reported; one case linked to extracorporeal shock wave lithotripsy | May be associated with other variants of lichen planus or autoimmune conditions | Usually an isolated condition, but associations with atopic dermatitis and autoimmune disorders reported | May be associated with psoriatic arthritis and other autoimmune conditions |
| Treatment | Topical and systemic corticosteroids, antihistamines; intralesional corticosteroids for refractory cases | Topical and systemic corticosteroids, topical calcineurin inhibitors, phototherapy | Usually self-limiting; topical corticosteroids may be used for symptomatic relief | Topical corticosteroids, Vitamin D analogs, phototherapy, systemic medications for refractory cases |
| Prognosis | Generally good, with potential for spontaneous remission; hyperpigmentation may persist | Generally good, but chronic and relapsing course is possible | Usually resolves spontaneously within months to years; recurrence rare | Variable; some cases may resolve with treatment whereas others may be chronic and recurrent |
In conclusion, ZLP is a rare variant of LP, distinguished by its dermatomal distribution and lack of association with varicella-zoster virus infection. Diagnosis relies on clinical and histopathological findings. Treatment focuses on managing symptoms, and the prognosis is generally favorable. Further research is needed to elucidate the exact pathogenesis and optimal management strategies for this unique condition.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Zosteriform lichen planus on the trunk: A case report of a rare clinical entity. Cureus. 2022;14:e22867.
- [CrossRef] [Google Scholar]
- Zosteriform lichen planus after herpes zoster: Report of a new case of Wolf 's isotopic phenomenon and literature review. Dermatol Online J. 2014;20:13030/qt5vf99178.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral zosteriform lichen planus involving multiple noncontiguous dermatomes with oral involvement. Indian Dermatol Online J. 2016;7:539-41.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral linear lichen planus along the lines of Blaschko. Indian J Dermatol. 2003;48:170-1.
- [Google Scholar]
- Blaschko-linear lichen planus of the face: A retrospective study of 6 cases and a literature review. Ann Dermatol Venereol. 2022;149:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lichen striatus: An updated review. Curr Pediatr Rev 2024 doi: 10.2174/0115733963273945240101042423
- [CrossRef] [Google Scholar]
- Clinical characteristics and therapeutic aspects of Blaschko linear psoriasis. Dermatol Ther (Heidelb). 2024;14:1039-48.
- [CrossRef] [Google Scholar]






