Translate this page into:
Trichilemmal cyst with xeroderma pigmentosum in pediatric patient – A case report with review of the literature

*Corresponding author: Janjala Narahari, Department of Pediatric surgery, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India. drnarahari@aiimsmangalagiri.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Narahari J, Vepakomma D. Trichilemmal cyst with xeroderma pigmentosum in pediatric patient – A case report with review of the literature. CosmoDerma. 2024;4:119. doi: 10.25259/CSDM_133_2024
Abstract
Pediatric trichilemmal cysts associated with xeroderma pigmentosum (XP) are rare. We report the case of an 11-year-old child with XP who presented with an ulcerative lesion on the right temporal region. A wedge biopsy of the lesion was performed under local anesthesia, and histopathological examination confirmed a benign, encapsulated trichilemmal cyst. The ulcerative lesion was treated conservatively, with no recurrence or complications reported in the 24 months following treatment. We recommend considering trichilemmal cysts as a differential diagnosis in cases of XP, alongside basal cell and squamous cell malignancies. To the best of our knowledge, this is the first reported case of a trichilemmal cyst in a child with XP.
Keywords
Trichilemmal cyst
Xeroderma pigmentosum
Pediatric patient
Ulcerative lesions
Skin malignancies
INTRODUCTION
A trichilemmal cyst, commonly known as a pilar cyst or “wen,” is a frequently occurring cyst that originates from the hair follicle.[1,2] These cysts account for approximately 10% of the population, with a higher prevalence in middle-aged females compared to males. Pilar cysts may have a hereditary component, often associated with autosomal dominant inheritance.[3] Clinically, these cysts are typically asymptomatic or mildly painful, presenting as firm, mobile masses filled with cytokeratin.[4] Trichilemmal cysts can occasionally become tender, inflamed, or rupture, and should be carefully differentiated from skin malignancies, such as nodular or nodulocystic basal cell carcinomas. This report discusses a case of a proliferating trichilemmal cyst in a child with xeroderma pigmentosum (XP), presenting as an ulcerative lesion on the scalp that closely mimicked a skin malignancy.
CASE REPORT
An 11-year-old boy presented with a history of photophobia, vertigo, and widespread brown pigmentation. He also had a 6-month history of a 4 × 3 cm ulceration on the right temporal region [Figure 1a]. The ulceration was non-bleeding and had no discharge. Based on these features, a provisional clinical diagnosis of XP associated with an ulcer was made. Given the increased risk of skin malignancies in XP patients, a wedge biopsy of the ulcer was performed for histopathological examination.

- (a) Child with xeroderma pigmentosum with ulcer and (b) follow-up pic of the child after successful treatment.
Histopathological analysis revealed a trichilemmal cyst, characterized by keratinized stratified squamous epithelium with keratinous luminal content and an absence of the granular cell layer [Figures 2 and 3]. We have done regular dressing with povidone iodine ointment and, the ulcer was healed within 10 days of starting treatment, and the child is on regular follow-up [Figure 1b].
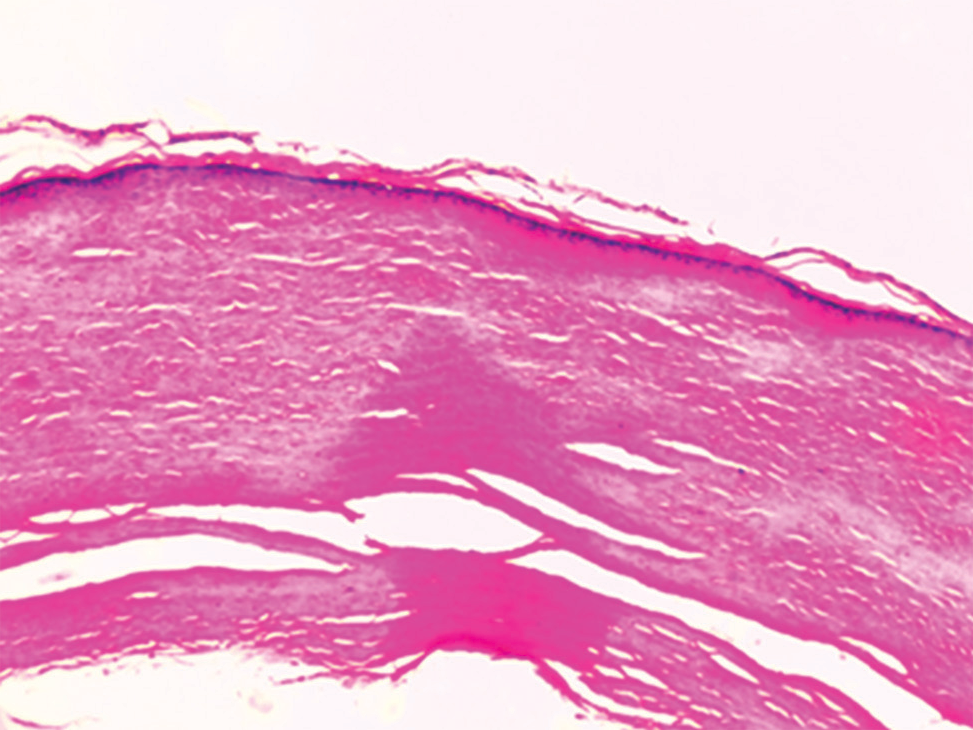
- Scanner view of the trichilemmal cyst lined by keratinized stratified squamous epithelium with keratinous luminal content (H&E, ×40).
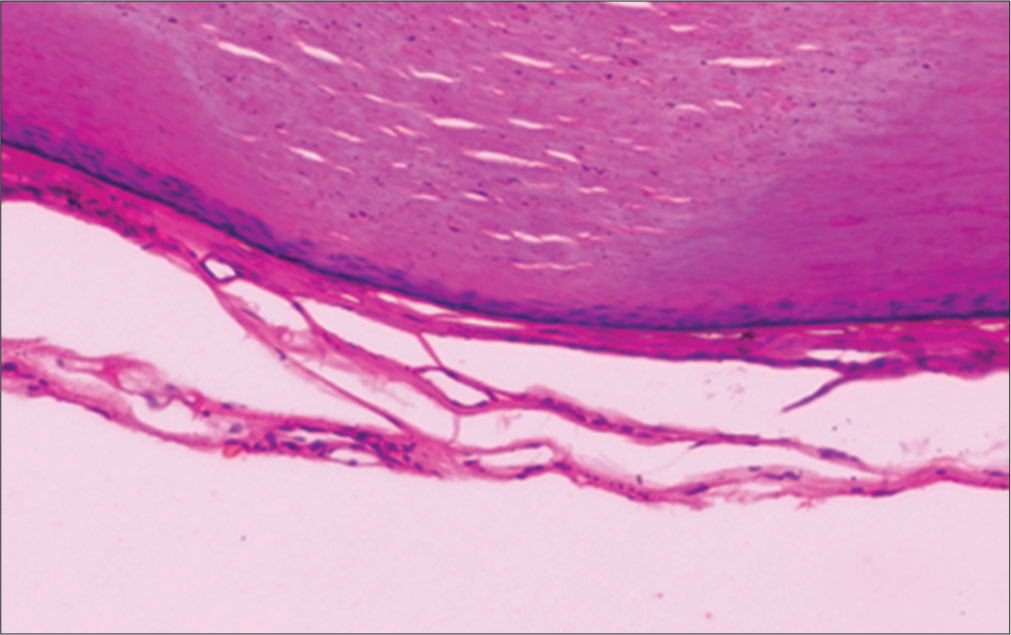
- Trichilemmal cyst lined by keratinized stratified squamous epithelium with absence of granular cell layer (H&E, ×400).
DISCUSSION
The diagnosis of pilar cysts is primarily clinical, based on presenting signs and symptoms. Radiological investigations are rarely necessary, except when differentiating between midline head and neck lesions or assessing the extent of lesion involvement with the central nervous system. The mainstay of treatment is surgical excision, which involves making a small incision in the skin to remove the cyst sac.[5]
In our case, due to the patient’s history of XP and the increased risk of skin malignancies, a wedge biopsy was first performed under local anesthesia to rule out skin cancer. Histological examination revealed abundant squamous proliferation, consistent with a trichilemmal cyst, as observed in our case. This squamous proliferation can rarely lead to the formation of a proliferating trichilemmal cyst, which may rupture and ulcerate. We speculate that this might have been the cause of ulceration in our patient.
Malignant proliferation in trichilemmal tumors is extremely rare and typically occurs in the sixth or seventh decade of life, with females being the most commonly affected gender.[6] Proliferative trichilemmal tumors often exhibit infiltrative growth, significant cytological atypia, and high mitotic activity including atypical forms and may involve lymph node metastases.[7] In our case, there were no clinical signs indicative of malignant proliferating trichilemmal tumor, no palpable lymphadenopathy, and histopathological examination, which showed no features consistent with malignancy, as seen in proliferating trichilemmal tumors.
There is a potential for misdiagnosis as squamous cell carcinoma due to the presence of dyskeratotic cells, mitotic figures, and nuclear atypia.[8] In our case, basal cell carcinoma was initially suspected, given its prevalence in XP patients, followed by squamous cell carcinoma. Fortunately, the lesion was confirmed to be a trichilemmal cyst.
CONCLUSION
In cases of XP with ulcerative lesions, the diagnosis of a trichilemmal cyst should also be considered alongside basal cell carcinoma and squamous cell carcinoma.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Proliferating trichilemmal cyst with focal calcifications. Dermatology Online J. 2008;14:25.
- [CrossRef] [Google Scholar]
- Cutaneous cysts In: Pathology of the skin with clinical correlations (3rd ed). China: Mosby; 2005. p. :1670.
- [Google Scholar]
- Hereditary trichilemmal cysts. A proposal for the assessment of diagnostic clinical criteria. Clin Genet. 2013;84:65-9.
- [CrossRef] [Google Scholar]
- Cytodiagnosis of simple and proliferating trichilemmal cysts. Acta Cytol. 2001;45:582-8.
- [CrossRef] [Google Scholar]
- IgG/IgE bullous pemphigoid with CD45 lymphocytic reactivity to dermal blood vessels, nerves and eccrine sweat glands. N Am J Med Sci. 2010;2:540-3.
- [CrossRef] [Google Scholar]
- Malignant proliferating trichilemmal tumour. Indian J Dermatol. 2012;57:50-2.
- [CrossRef] [Google Scholar]
- Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cysts. Dermatologica. 1983;166:203-8.
- [CrossRef] [Google Scholar]
- Malignant proliferating trichilemmal cyst. J Am Acad Dermatol. 1995;32:870-3.
- [CrossRef] [Google Scholar]






