Translate this page into:
Therapeutic efficacy of topical liquid nitrogen cryotherapy in pearly penile papules

*Corresponding author: Mohita Mahajan, Department of Dermatology, Government Medical College, Amritsar, Punjab, India. mohitamahajan96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh R, Mahajan M, Mahajan BB. Therapeutic efficacy of topical liquid nitrogen cryotherapy in pearly penile papules. CosmoDerma. 2024;4:63. doi: 10.25259/CSDM_59_2024
Abstract
Objectives:
Pearly penile papules (PPP) are small dome-shaped to filiform skin-colored papules that are typically located on the coronal sulcus of the glans penis. Present modalities of treatment include ablation using carbon dioxide laser, electrodessication with curettage, and excision. The present study was undertaken to evaluate the efficacy of topical liquid nitrogen cryotherapy with the dipstick method as a therapeutic modality for the treatment of PPP.
Materials and Methods:
Forty patients with the clinical diagnosis of PPP were enrolled for the study. After cleaning the involved area with povidone-iodine solution, the appropriate autoclaved applicators were dipped in liquid nitrogen, applied on the involved area, and repeated to complete two freeze-thaw cycles of 2 s each. All the patients were subjected to three applications at weekly intervals (0, 1, and 2 weeks). Follow-up were done fortnightly for up to 12 weeks.
Results:
The majority of the patients were in the age group 20 – 40 years. A significant number of patients (35%) presumed these lesions to be associated with sexually transmitted infection. Most of the patients 29 (72.5%) had a duration of lesion <1 year, 10 (25%) patients had lesions since 1 – 5 years, while 1 (2.5%) patient had lesions since 30 years. Complete resolution of lesions was seen in 85% of patients.
Conclusion:
Cryotherapy with liquid nitrogen is an effective modality in the treatment of PPP. Advantages are ease of use, low cost, good cosmetic results, high cure rate, no requirement of anesthesia, and rarity of complications, and above all patients of any age can be treated.
Keywords
Cryotherapy
Liquid nitrogen
Pearly penile papules
INTRODUCTION
Pearly penile papules (PPP) are also known as “hirsutoid papillomas,” and Hirsuties coronae glandis,[1] Tyson glands,[2] hirsutoid papillomas,[3] papilla in the corona glandis,[4] hirsuties papillary corona of the penis,[5] corona capillitia,[6] and pink pearly papules[7] by different workers. These are small dome-shaped to filiform skin-colored papules that typically are located on the sulcus or corona of the glans penis. Commonly, PPP are arranged circumferentially in one or several rows and often are assumed wrongly to be transmitted sexually. The incidence of PPP reportedly ranges from 8 to 48%. It is a harmless anatomical variation. They are found significantly more often in uncircumcised men and younger men. They range in size from <1 to 3 mm. These are not transmitted through sexual activity and are not a sexually transmitted infection (STI).[8,9] Present modalities of treatment for PPP are ablation using carbon dioxide laser,[10,11] electrodessication with curettage,[11] and excisional surgery. The present study was undertaken to evaluate the efficacy of topical liquid nitrogen cryotherapy with the dipstick method as a therapeutic modality for the treatment of PPP.
The aim of the study was to evaluate the efficacy of topical liquid nitrogen cryotherapy in PPPs.
MATERIALS AND METHODS
A prospective interventional study enrolling 40 patients of PPP from the STI clinic of a tertiary care hospital was undertaken. The sample size was calculated by convenience sampling.
Information collected in the routine clinical history included the patient’s sex, location and distribution of the disease, age at onset, family history, and disease activity. The diagnosis was based on clinical examination. All the male patients attending the sexually transmitted disease clinic were thoroughly worked up. All the patients were evaluated both by the treating physician himself and confirmed by an observer.
Inclusion criteria
Those with clinical features of PPP and willing to undergo cryotherapy were included in the study.
Exclusion criteria
Patients with cold intolerance, cold urticaria, Raynaud’s disease, and the presence of active fungal or any other infection were excluded from the study. All the patients were counseled and the benign nature of the disease was explained before enrolling them for study. The study protocol was approved by the ethical committee of the institution where the study was conducted. Written informed consent was taken from each patient before undergoing procedure. A detailed history and general physical examination including local examination and routine investigations was conducted in each case [Figure 1].
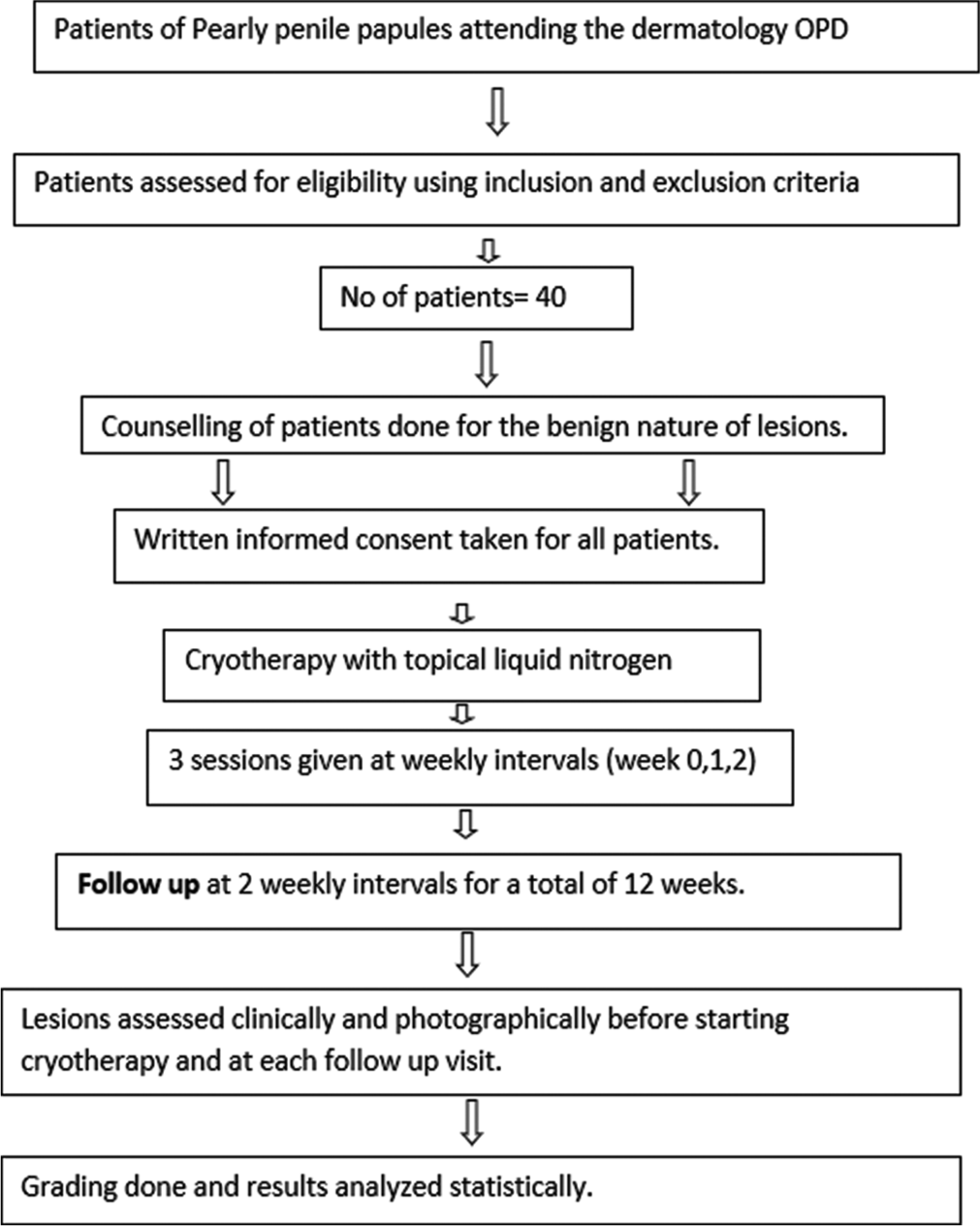
- The protocol of the study conducted.
- OPD: Outpatient department.
At the test site, after cleaning the involved area with povidone-iodine solution, the appropriate autoclaved applicators were dipped in liquid nitrogen, applied on the involved area, and repeated to complete two freeze-thaw cycles of 2 s each. Antibiotic ointment for local application post-cryotherapy was advised.
All the patients were subjected to three applications at weekly intervals (0, 1, and 2 weeks). Follow-up was done every two weeks for up to 12 weeks.
All the patients were assessed clinically as well as photographically at the baseline, at each visit before subjecting to cryotherapy and at each follow-up visit.
Patients’ response to treatment was graded both subjectively by visual analog scale and objectively as follows: GO – <25% of clearing of papules (poor), G1 – 25 – 50% of clearing of papules (fair), G2 – 51 – 75% of clearing of papules (good), G3 – >75% of clearing of papules (very good), and G4 – complete clearance of papules (excellent). Results were analyzed statistically after follow-up of 12 weeks.
Statistical analysis
Categorical variables were presented in number and percentage and continuous variables were presented as mean ± standard deviation. Quantitative variables were compared using an unpaired t-test between two groups. The qualitative variable was correlated using Chi-square test. P < 0.05 was considered statistically significant.
RESULTS
In this study of 40 patients with ages ranging from 15 to 40 years, the majority of the patients were in the age group of 20 – 40 years. Maximum number of patients was students (47.5%). The majority of the patients belonged to cities and towns (67.5%) while 32.5% were rural. Most of the patients presented with the duration of lesions <1 year (72.5%) and only 2.5% had a history of >5 years. A significant number of patients (35%) presumed these lesions to be associated with STI.
First, follow-up was done on the 4th week (28th day) and 34 patients (85%) showed 100% (grade 4) improvement, 3 (7.5%) showed 75% (grade 3), and 3 (7.5%) showed 50% (grade 2) improvement [Figures 2 and 3]. On the second follow-up at 6 weeks (42nd day), 34 patients (85%) showed 100% (grade 4) improvement, 3 (7.5%) showed 75% (grade 3) improvement, and 3 (7.5%) showed 50% (grade 2) improvement [Figures 4 and 5]. In the 3rd follow-up (56th day) at 8 weeks, 34 (85%) showed 100% (grade 4) improvement, 3 (7.5%) showed 75% (grade 3) improvement, and 3 (7.5%) showed 50% (grade 2) improvement. After the 4th follow-up (70th day) at 10 weeks, 34 (85%) showed 100% (grade 4), 5 (12.5%) showed 75% (grade 3), and 1 (2.5%) showed 50% (grade 2) improvement. In the last follow-up done on the 84th day at 12 weeks, 34 (85%) showed 100% (grade 4) improvement, 5 (12.5%) showed 75% (grade 3) improvement, and 1 (2.5%) showed 50% (grade 2) improvement. Thus, finally on the 84th day, 34 patients had full clearance of lesions, five patients showed 75% clearance of lesions, and one patient showed 50% clearance of lesions.

- (Patient 1): Lesion on day 0.

- (Patient 1): Complete resolution on day 28.

- (Patient 2): Lesions on day 0.

- (Patient 2): Complete resolution on day 42.
The side effects associated with cryotherapy were minimal like a burning sensation felt immediately after application of liquid nitrogen. Only three patients showed erythema which persisted for a few days after application and faded on its own. Two patients felt pain after application which decreased after 4 – 6 h. One patient had blister formation after the first application, which healed after one week with topical antibiotics. Majority of the patients, that is, 34(85%) had no side effects associated with the therapy [Table 1].
| Side effect | N | Percentage |
|---|---|---|
| No side effect | 34 | 85 |
| Blister | 1 | 2.5 |
| Erythema | 3 | 7.5 |
| Pain | 2 | 5 |
| Total | 40 | 100 |
N: Number of patients.
DISCUSSION
The PPP are benign and harmless anatomical variations present on the penis. They are found significantly more often in uncircumcised men and younger men. They are almost always asymptomatic and therefore detected incidentally in most cases. The PPP are histologically similar to acral angiofibromas. They usually do not require any treatment except reassurance, although many therapies have been tried in patients with PPP, who may request therapy to alleviate psychological anxiety.
Various studies have reported cases ranging from an 11-year-old boy[12] to a 52-year-old man,[13] but it commonly occurs in pubertal boys and young adults. Urban patients outnumbered rural patients in the present study. This might be attributed to the fact that urban patients seek treatment even for asymptomatic but cosmetically disturbing skin conditions. Most of the patients had a duration of lesion <1 year, indicating that PPP lesions cause psychological distress to the patients, and thus, they seek treatment early. Therapies used for the treatment of PPP such as electrodessication and curettage or surgery may lead to various side effects such as post-operative infection and scarring. Lasers such as CO2 laser ablation, ablative 2940 Er: YAG laser,[11] fractional resurfacing with 1550 nm erbium laser, and pulsed dye laser have been used.[14] Carbon dioxide laser appears to be an effective treatment but costly affair.[10] Therefore, cryotherapy should be the preferred treatment, as it is cost effective and without significant side effects and can be used in any age group.
Limitations
Larger, multicentric randomized controlled studies are needed to substantiate the results of our study.
CONCLUSION
The PPP are asymptomatic lesions that despite their benign nature can cause significant distress in male patients due to the fear of STIs and can affect the quality of life. Cryotherapy with liquid nitrogen is an effective modality in the treatment of PPP. Advantages are ease of use, low cost, good cosmetic results, high cure rate, no requirement of anesthesia, and rarity of complications, and above all patients of any age can be treated.
Ethical approval
The research/study approved by the Institutional Review Board at Guru Gobind Singh Medical College, Faridkot, number It was approved in 2012, dated 2012.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hirsutoid papillomas of coronal margin of glans penis. J Urol. 1955;74:375.
- [CrossRef] [PubMed] [Google Scholar]
- Pearly penile papules: A statistical study of incidence. Arch Dermatol. 1966;93:56.
- [CrossRef] [Google Scholar]
- Pink pearly papules: an epidemiologic study. J Pediatr. 1984;105:594-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pearly penile papules: A review. Int J Dermatol. 2004;43:199-201.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of pearly penile papules with fractionated CO2 laser. J Clin Aesthet Dermatol. 2015;8:50-2.
- [Google Scholar]
- Management of pearly penile papules: A review of the literature. J Cutan Med Surg. 2020;24:79-85.
- [CrossRef] [PubMed] [Google Scholar]
- Ectopic pearly penile papules: A pediatric case. Genitourin Med. 1997;73:136.
- [CrossRef] [PubMed] [Google Scholar]
- Pearly penile papules-A common cause of concern. Int J STD AIDS. 1999;10:726-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of pearly penile papules. Am J Mens Health. 2018;12:624-7.
- [CrossRef] [PubMed] [Google Scholar]






