Translate this page into:
The repurposing of single-use disposable plastic available in dermatology departments for genital dermatoscopy

*Corresponding author: Nikhil Mehta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. nikhilmehtadermatology@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain A, Manandhar K, Mehta N. The repurposing of single-use disposable plastic available in dermatology departments for genital dermatoscopy. CosmoDerma. 2024;4:55. doi: 10.25259/CSDM_46_2024
PROBLEM
In routine outpatient use, a hand-held dermatoscope is rapidly used in successive patients. Often, contact with mucosal, genital, ulcerative, and potentially infective lesions is required, which can make the dermatoscope dirty, obscure the field of vision, and may lead to cross-contamination. Frequent cleaning may damage the lens or the surface of the dermatoscope.
The disposable caps and coverings available with the dermatoscope are few in number and expensive. Solutions involving the usage of glass slides, adhesive tapes, and food-wrapping plastics/cling films have been suggested,[1] but they are impractical, as they lack sterility and user-friendliness and are thin and fragile, leading to wrinkling and tearing. Adhesive tapes stick to the dermatoscope and make it dirty and may need cleaning to be removed completely. They are required to be carried separately with the dermatoscope and have to be purchased separately, incurring cost, and leading to wastage.
SOLUTION
We propose leveraging single-use disposable sterile plastic cover material of materials commonly found in a dermatology clinic, operation theater, and ward, including packets of gauze pieces, punch biopsy instruments, intravenous sets, normal saline bottles, medical drapes, etc. [Figure 1]. They can easily form an interface between the dermatoscope and the skin [Figure 2] and enable clear dermatoscopy [Figure 3]. Compared to cling film wraps, they are packaged sterile, are thick but transparent, and do not wrinkle or tear easily. They are easily obtainable without any waiting in our setting in situations when there is an unexpected need for mucosal dermatoscopic examination, especially when dermoscope caps or cling films are not available at hand. Hence, it can be rapidly deployed using in-house waste material in a pinch by dermatologists, who do not carry caps and cling films with them or have forgotten or exhausted them on a particular day. This repurposing of waste material poses no additional financial burden and does not increase biomedical waste, in contrast to the usage of separate disposable caps, maintaining sustainability in the current era of increasing plastic waste.
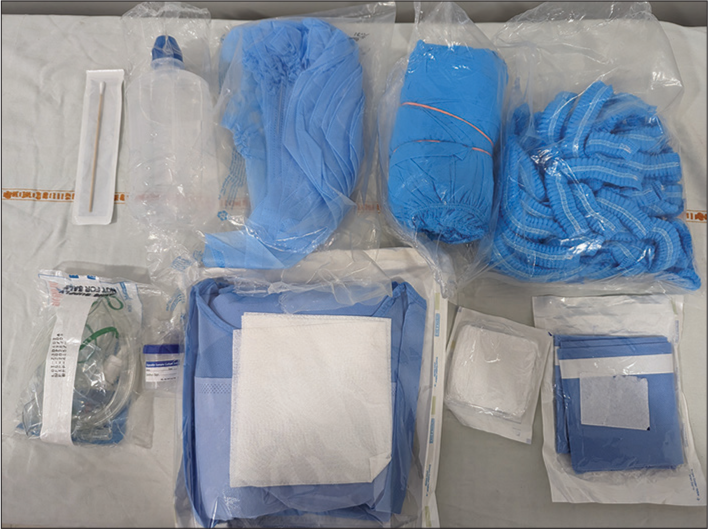
- Various single-use disposable sterile plastic covers of cotton swabs, intravenous sets, normal saline bottles, gauze pieces, and different medical drapes.
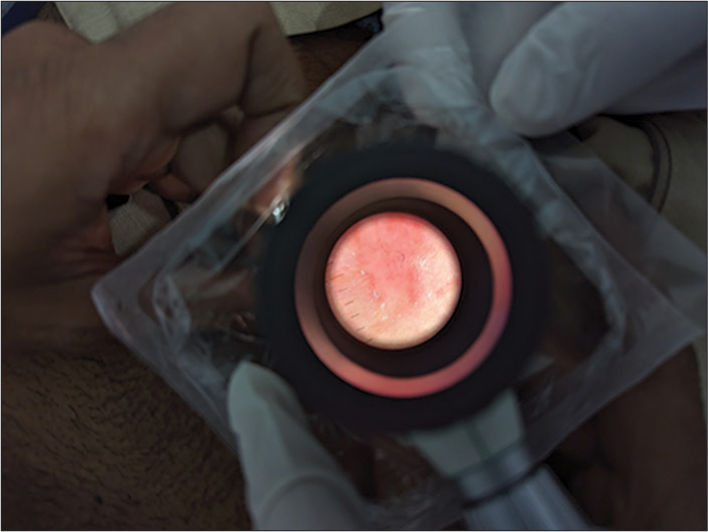
- Dermatoscopy of a genital lesion using single-use disposable plastic cover as a sterile interface.
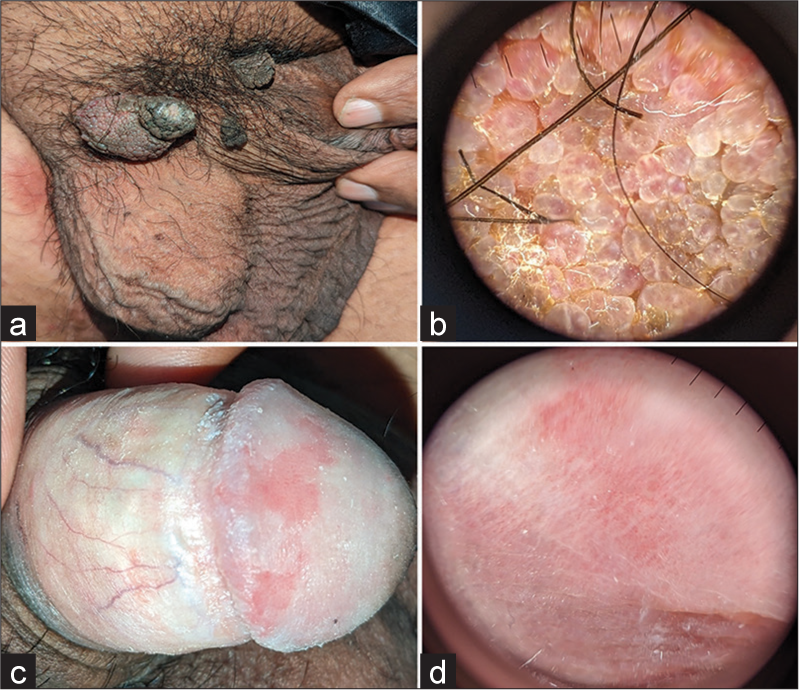
- Some examples of genital dermatoscopy using plastic materials as interface (a) genital warts, (b) corresponding dermatoscopic image showing lobules with red linear and lacunar vessels suggestive of warts, (c) erosive genital lichen sclerosus et atrophicus, and (d) corresponding dermatoscopy showing ill-defined white areas with red dotted and thin linear vessels.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Use of transparent film dressing for dermoscopy of mucosal lesions. Pediatr Dermatol. 2016;33:107-8.
- [CrossRef] [PubMed] [Google Scholar]





