Translate this page into:
Rosacea awareness among med students: In-depth survey analysis

*Corresponding author: Yusra Fathima, Department of Medicine, Faculty of Medicine, Tbilisi State Medical University, Tbilisi, Georgia. yusrafathima101@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Fathima Y, Karawita JA, Koshy R, Aji A, Korrapati N, Sarvaiya K. Rosacea awareness among med students: In-depth survey analysis. CosmoDerma. 2024;4:77. doi: 10.25259/CSDM_68_2024
Abstract
Objectives:
The main aim of this cross-sectional study is to assess the knowledge of medical students of Tbilisi State Medical University for creating awareness about rosacea among healthcare professionals and the community.
Materials and Methods:
A cross-sectional study in an online survey style was conducted over 2 months among international medical students to assess rosacea awareness. Participants (n = 86) answered questions covering etiology, epidemiology, pathophysiology, clinical expression, treatment modalities, and personal encounters with rosacea patients. Statistical analysis categorized responses by gender, academic year, and awareness levels.
Results:
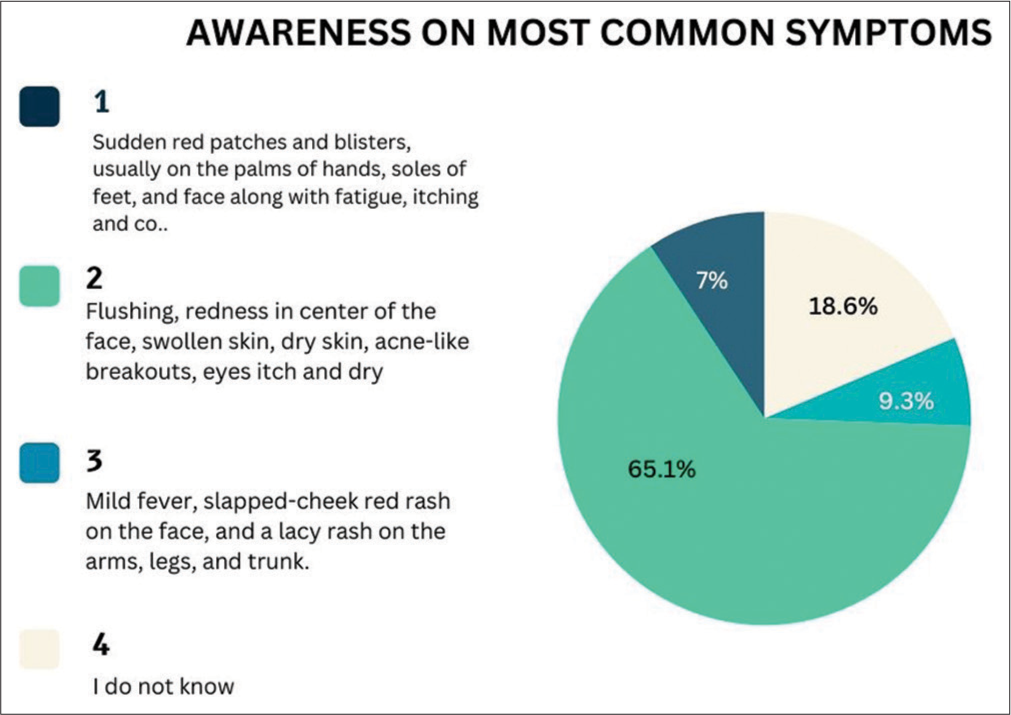
Survey results revealed varying awareness levels among participants. While most recognized rosacea and its symptoms exist, knowledge gaps exist in identifying types, severity signs, genetic links, dietary influences, and treatment modalities. Clinical-year students exhibited superior awareness compared to their preclinical counterparts, indicating the influence of clinical exposure.
Conclusion:
The study highlights inconsistent awareness of rosacea among medical students, emphasizing the need for comprehensive education. Limited exposure to real-world cases underscores the importance of clinical training. Bridging knowledge gaps through updated curricula and practical training can enhance future health-care professionals’ preparedness to diagnose and manage rosacea effectively, thereby improving patient outcomes and quality of life. Further, research and educational interventions are warranted to address these gaps and promote a better understanding of and management of rosacea.
Keywords
Rosacea awareness
Survey analysis
Skin disorder management
Dermatology
INTRODUCTION
Rosacea is a common chronic inflammatory dermatosis with a higher incidence seen in females compared to males.[1] The National Rosacea Society (NRS) estimates that 415 million people have rosacea worldwide and the disease primarily affects adults 45–60 years of age.[2] In 2017, an updated classification was proposed by the Global Rosacea Consensus (ROSCO) panel, suggesting two key features; persistent centrofacial erythema and phymatous changes which were based on an increased understanding of the disease and a combination of diagnostic methodologies.[3] The pathophysiology of rosacea is still under investigation but is associated with risk factors including genetic-environmental reasons, obesity, smoking sun exposure, heat, cold, alcohol, spicy food, and stress.[1,4] There are four main phenotypic subtypes of rosacea according to the NRS, 2002 which include papulopustular, phymatous, ocular, and erythematotelangiectatic forms.[5] Rosacea can cause a serious psychosocial impact on a patient’s life, which can lead to emotional distress, low self-esteem, and depression; hence, prompt diagnosis and early start of treatment is crucial.[5] The treatment of rosacea depends on its severity and involves gentle skin cleansing, sun protection, avoiding triggers, dietary changes, topical treatments such as metronidazole, azelaic acid, brimonidine, and antibiotic therapies. In addition, laser and surgical methods have also proven to be beneficial in certain forms.[1]
A study conducted on Korean rosacea patients stated that they often have relatively little awareness and knowledge of the condition while another stated that low awareness on the part of both patients and doctors could be one of the reasons on low data on ocular rosacea.[6,7] There are very rare studies, which focus on the knowledge imparted on medical students about rosacea, which describes the huge research gap in understanding of this condition. Hence, our study aims at understanding and creating awareness about this condition among future health-care professionals.
MATERIALS AND METHODS
This cross-sectional study investigates the knowledge of rosacea among International medical students from Tbilisi State Medical University, based in Tbilisi, Georgia, by the use of an electronic form survey-based study over 2 months, receiving 86 responses. The survey consisted of a detailed set of 21 questions, obtaining consent from the participants and covering the etiology, epidemiology, pathophysiology, risk factors, clinical expression, choice of treatments, and their posology, and, if the participants have come across any medically diagnosed rosacea patients. Questions about participants’ gender, age, and year of study were also recorded [Figure 1].
- Detailed list of questions which were part of the survey
The results were disseminated with the help of statistical analysis by the researchers with the use of Google Forms and classed carefully within discrete age groups, genders, and years of study. Students of years 1–3 and 4–6 are termed preclinical and clinical, respectively. Ethical approval is waived for this study.
RESULTS
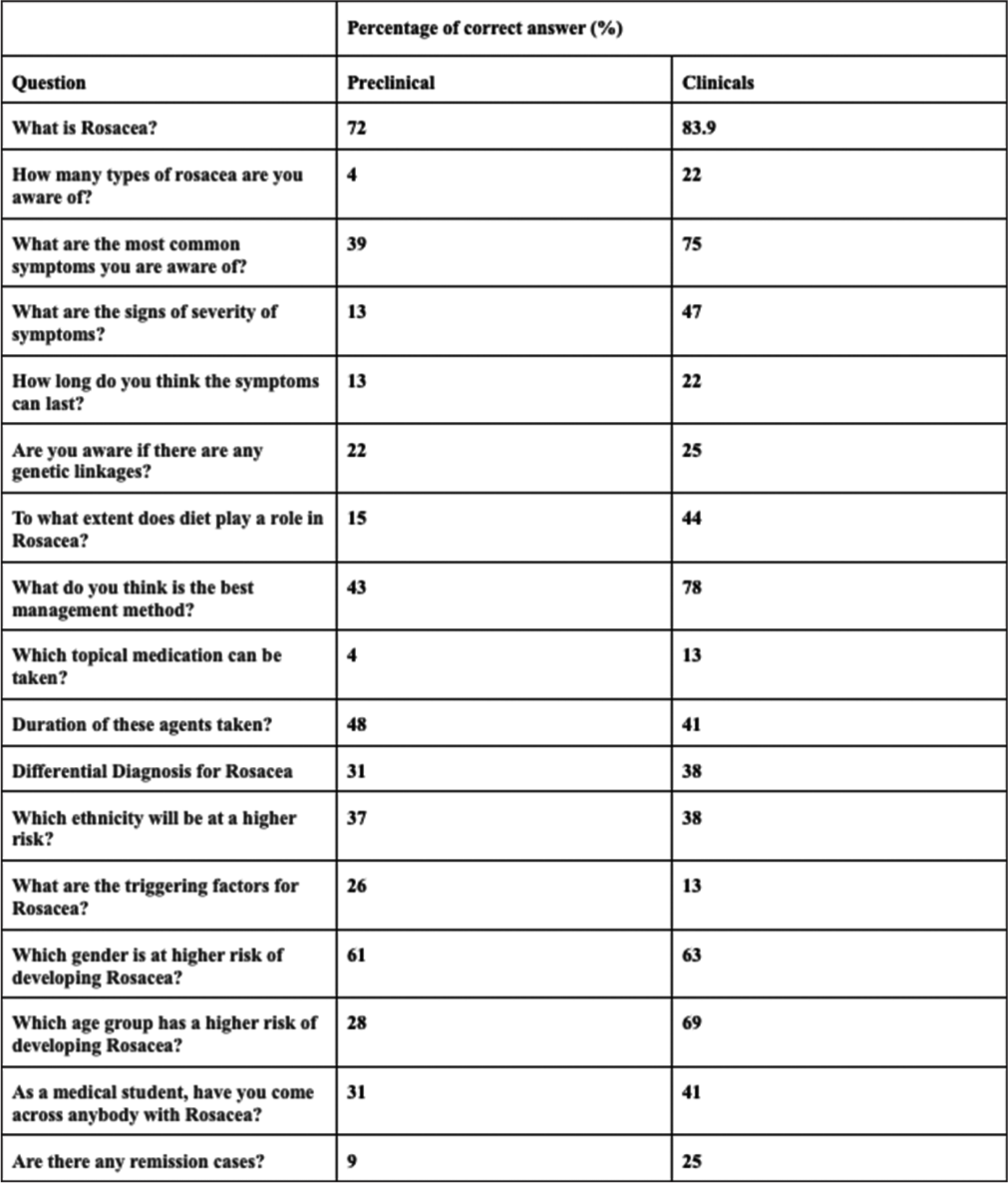
As per the results of the survey that sampled 86 responses, 80.2% of the surveyors were female, and 19.8% were male, coming mostly from 2nd year (32.6%), then 1st years (20.9%), and then 5th years (18.6%), then 4th years as 12.8%, and then the minority being 3rd years, and a 5.8% of 6th years. About 75.6% of the sample knew the definition of rosacea, while the rest 24.4% did not recognize it [Figure 2].
- (A, B, C, D) Responses from the students to the question “What is rosacea?”.
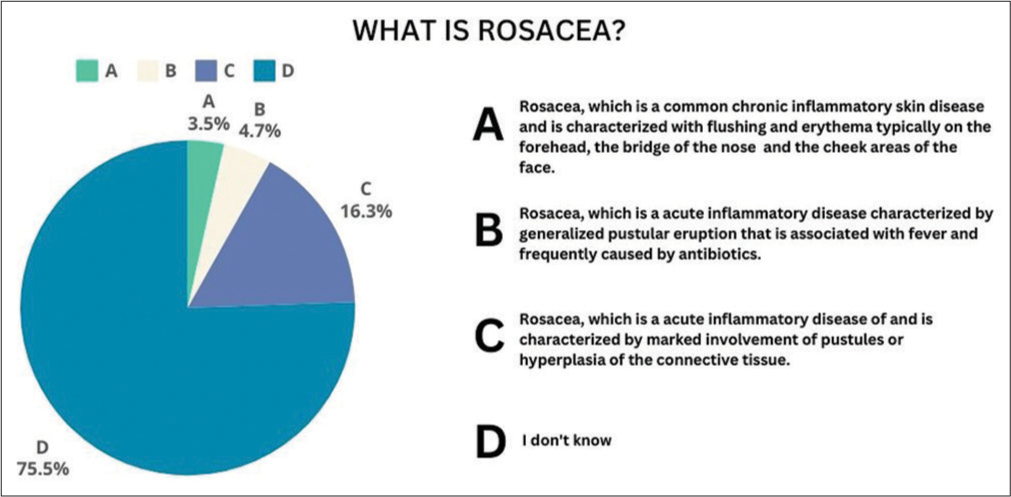
On proposing the types of rosacea present, 53.5% of the sample felt there were no types, while majorly recognizing papulopustular to be more commonly recognized at 38.4% than erythematotelangiectatic at 27.6%, then ocular coming in next with 25.6%, and then phymatous not being recognized as much at 18.6% [Figure 3].
- Responses from the students when asked about the types of rosacea.
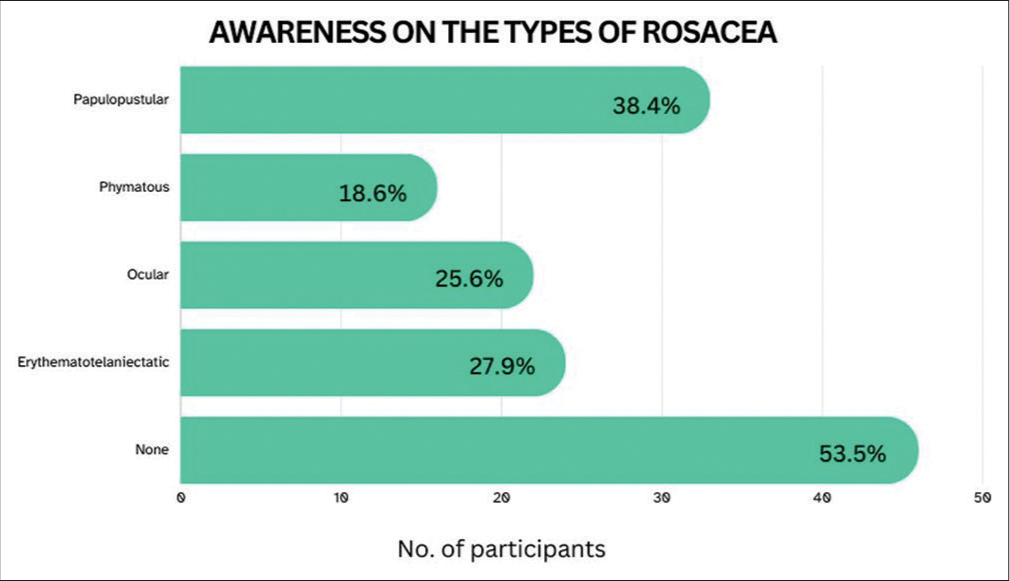
On analysis of the recognition of the symptoms of the most common symptom of rosacea to be redness, 65.1% recognize it to be defined as, “Flushing, redness in the center of the face, swollen skin, dry skin, acne-like breakouts, and eyes itch and dry.” It is notable to mention that 16.3% of the sample could not pinpoint the symptoms, while 18.6% had no idea of the skin manifestations of rosacea [Figure 4].
- (1, 2, 3, 4) Responses of the students on awareness among students on the most common symptoms of rosacea.
On the 86 responses answering the recognition of the signs of severity, the vast majority, 39.5%, did not know. About 26.7% of people identified “Rhinophyma and Papulopustules” as the strongest sign of severity [Figure 5].
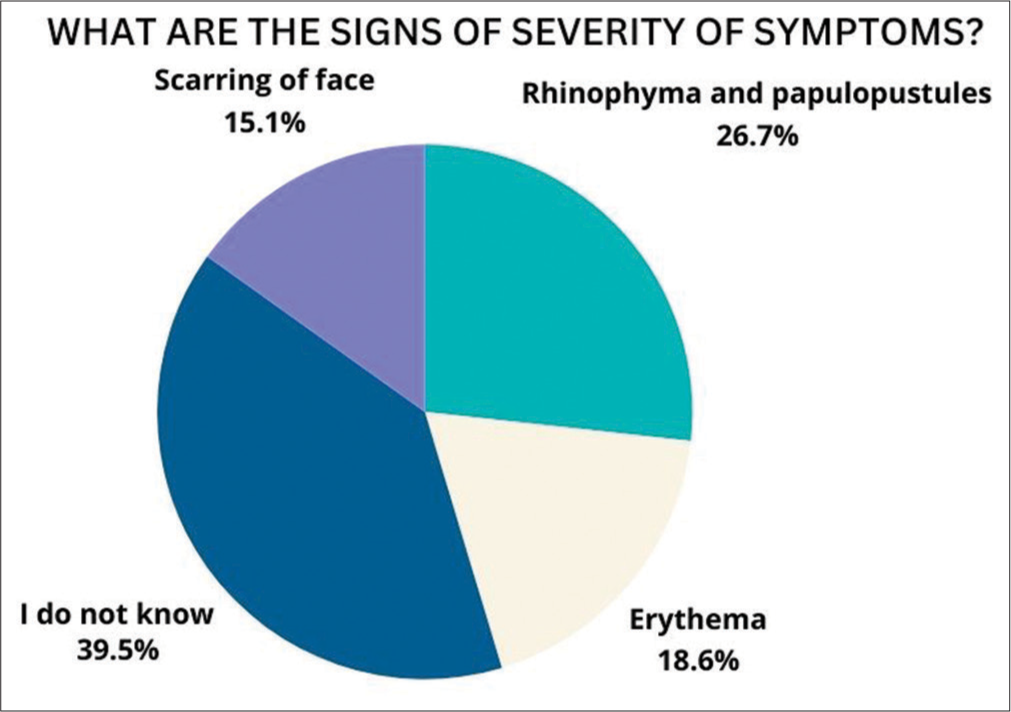
- Responses of the students on the signs of severity of symptoms
With the duration of symptoms, 27.9% said they did not know, while 18.6% recognized the symptoms to last a few days to a few weeks. About 20.9% of the sample felt the duration of symptoms a few months to years. Furthermore, 16.3% felt that lifelong treatment was necessary, and another 16.3% felt the symptoms to last for a few weeks to a few months
Minutely, 23.3% recognized that there is a genetic linkage, while 30.2% rejected it. About 34.9% did not know about the association between diet and rosacea, while 34.9% there is a situational link, while 25.6% strongly felt there is.
According to the awareness of the management method, topical agents were the most preferred management method, with a percentage of 58.1%. With a display of “I don’t know” secondly at 18.6%, most others thought the medications (10.5%), hormonal therapy (8.1%), and home remedies (3.5%) were the best management methods [Figure 6].
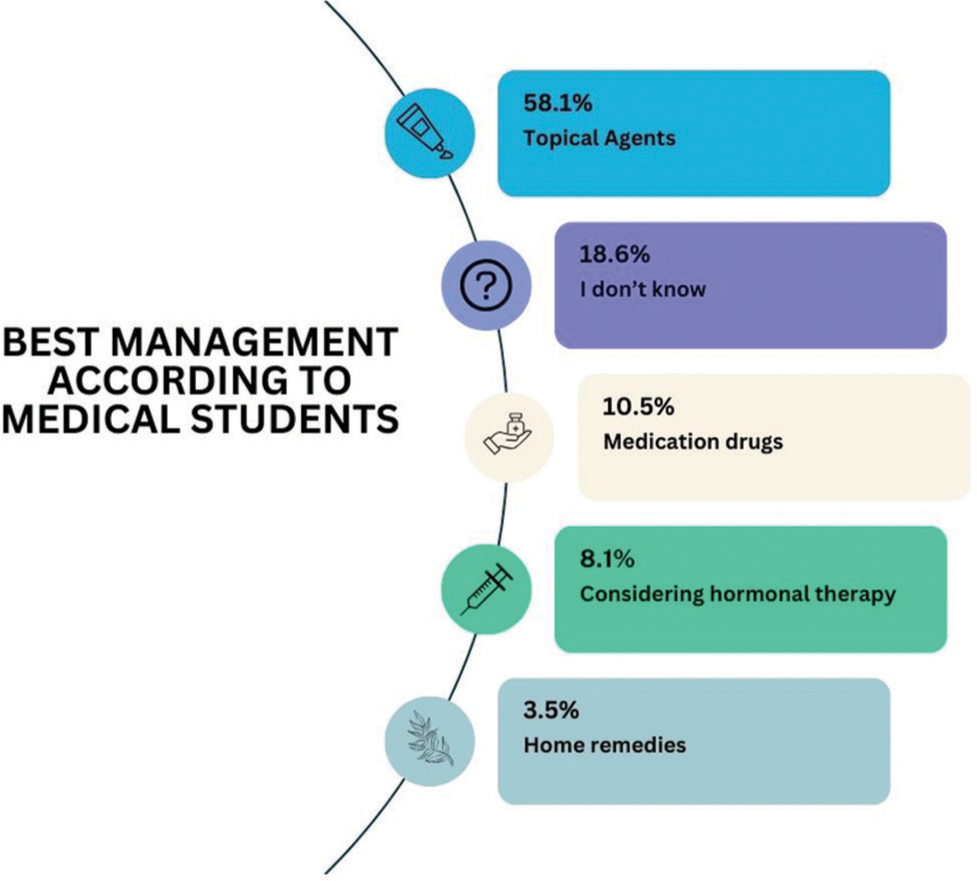
- Responses from the students on best management methods of rosacea
Most of the sample had limited knowledge about which topical medication to use, while only 24.4% correctly identified azelaic acid as the appropriate medication. The selection of metronidazole, ivermectin, and brimonidine was very limited [Figure 7]. About 38.4% did not know the duration of these agents.
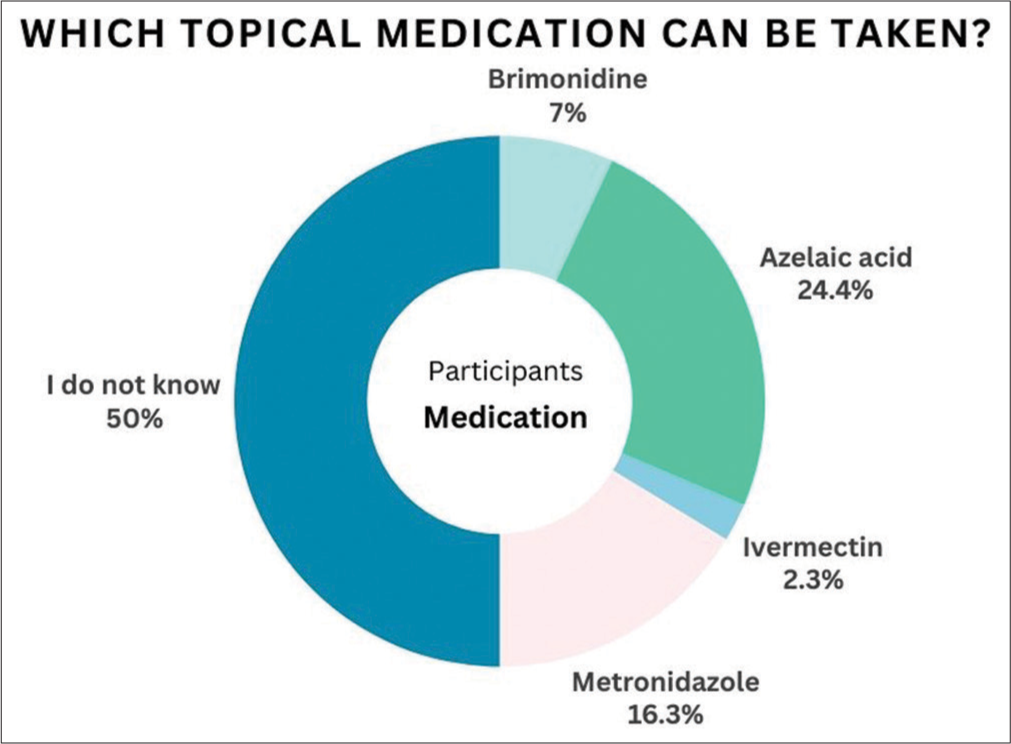
- Responses of the students when asked about topical medication for rosacea.
Regarding differential diagnosis, 33.7% felt acne vulgaris, dermatitis, lupus, and folliculitis to be potential answers. Singularity, 19.8% felt dermatitis to be the sole answer with acne vulgaris coming in as 10.5%. It is notable to mention that 29.1% did not know [Figure 8].
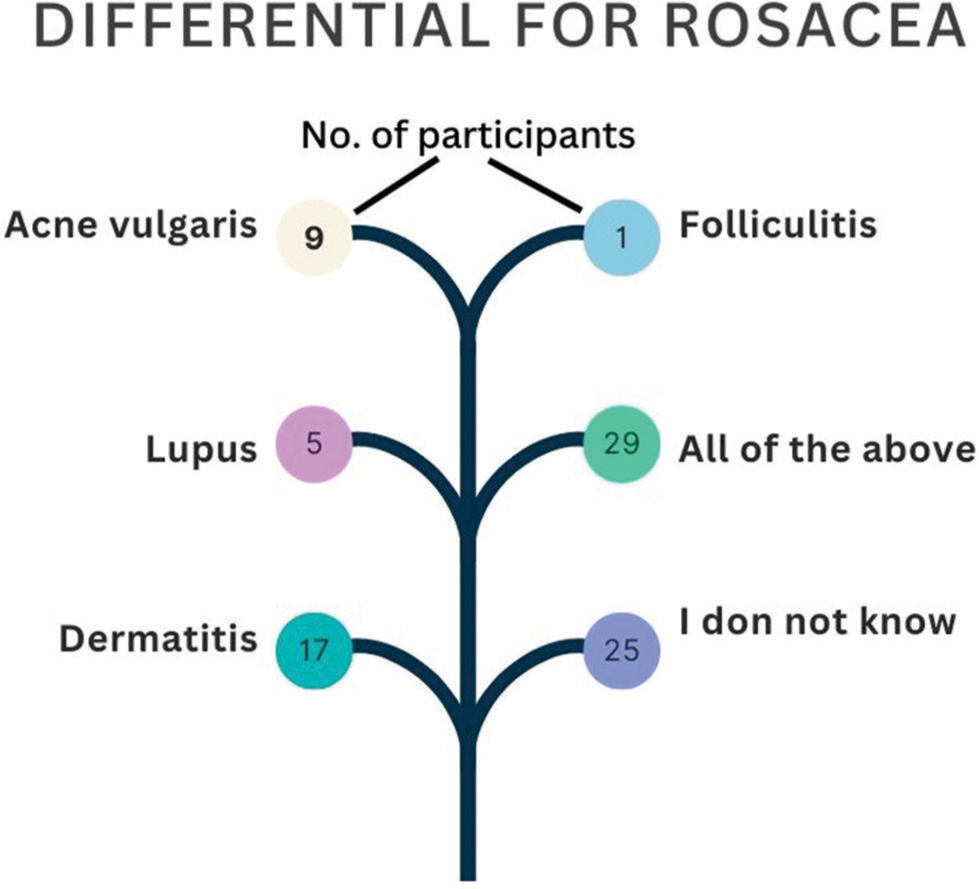
- Responses of the students on differential for rosacea
On analysis of awareness of high-risk individuals according to ethnicities, 50% did not know. About 37.5% felt Northern and Western European descent to be affected more than the other ethnicities. Second, 8.1% chose Southeast Asia to be affected [Figure 9].
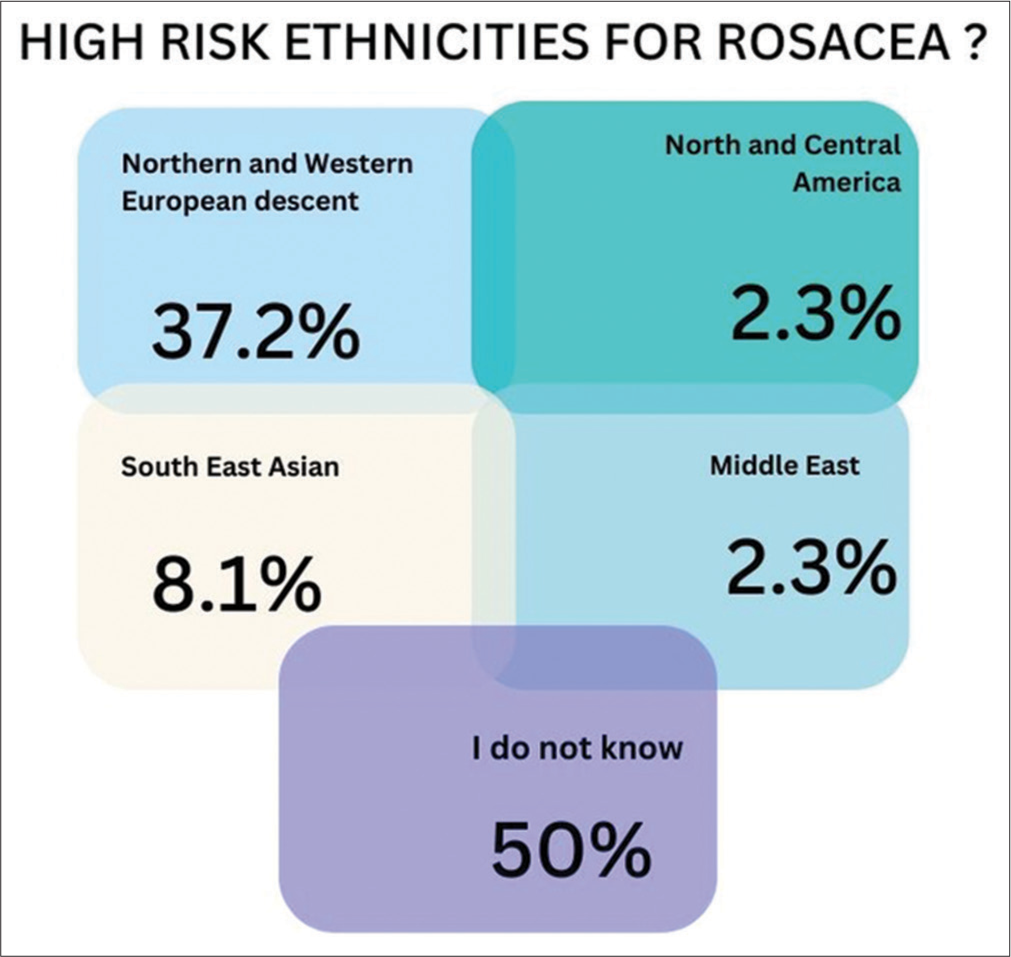
- Responses of the students on the ethnicity with the highest risk for rosacea
About 26.7% correctly recognized all the risk factors for rosacea. About 40.7% found exposure to harsh sunlight to be a stronger risk factor, with spicy food coming in second at 27.9%, being of female gender at 25.6%, age 30–60 being at 14%, and having multiple systemic illnesses. About 30.2% did not know [Figure 10].
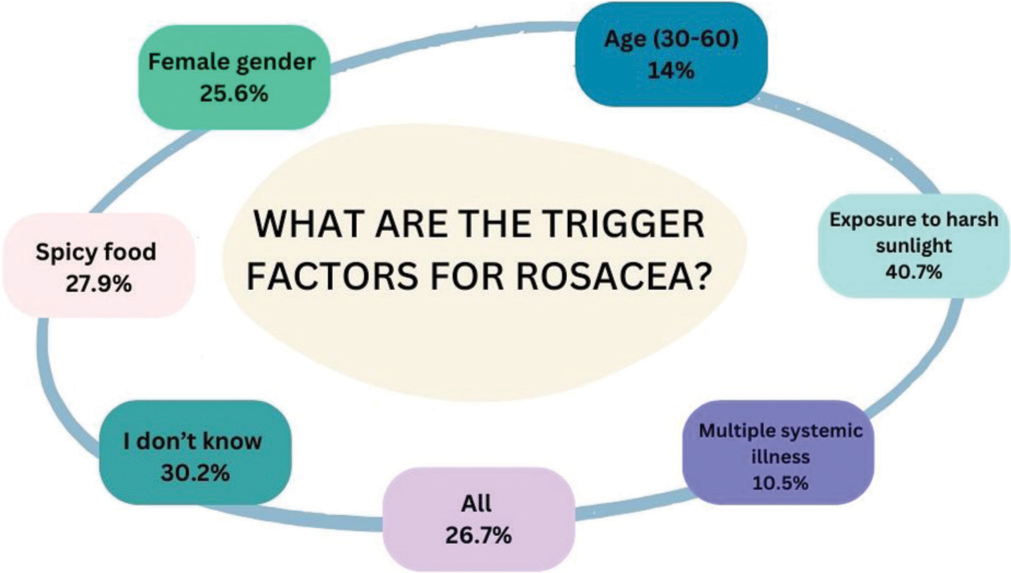
- Responses of the students on the trigger factors for rosacea.
About 61.6% of the sample recognized females to be the gender with the highest gender at risk, while 30.2% did not know. A small minority of 3.5% found males to be more affected, and 4.7% felt none of the above to be affected, while 0% chose the “others” option.
It is correct that rosacea affects individuals from the ages of 30–65. 24.4% of the sample felt adults aged 25–40 to be more at a higher risk, while 18.6% felt middle ages of 40–65 years to be affected more. About 37.2% found young adults to be affected.
On inspection to see how often our sample is, it is notable that 65.1% have never discovered a rosacea patient, while 27.9% have discovered less than three cases. Regarding remission cases, a vast majority of 80.2% did not know, and only 15.1% were aware of the remission cases.
DISCUSSION
Rosacea, a common chronic dermatological condition of the face with remission and relapse, has already proved its prevalence across different populations and geographic regions.[8] According to recent studies, it affects up to 22% of the population and is often linked to multifactorial etiologies contributing to significant psycho-social impact.[5] There is an urge for healthcare professionals, to identify and diagnose rosacea due to its higher prevalence in the general population and negative psychosocial impact.[9]
Early identification also allows prompt intervention and management, which can prevent the progression of the condition and minimize potential complications, thus improving the patient’s quality of life.[1] By understanding different aspects of rosacea, medical students can accurately provide information to patients and help manage their symptoms effectively.[7] Since rosacea often requires multidisciplinary and symptom-based management, medical students should be aware of different lifestyles and treatment options.[8]
It is crucial to understand that the sample predominantly comprises international medical students from Tbilisi State Medical University. The education structure entails module-based preclinical years (1–3) and clinical rotations in years 4–6. While the faculty has some focus on dermatology concepts, there are significant systemic obstacles limiting quality patient interactions in hospitals.
On a sample of 86 responses, with a majority of females, there is a general understanding of the nuances of rosacea, especially what it is, and its symptoms. For the nuances of the types, the treatment, diet, and genetics, the results varied immensely, especially when the sample was divided into preclinical and clinical the difference was significant throughout the academic years. This study recognizes the importance of the wide array of clinical manifestations of rosacea, which emphasizes the significance of early diagnosis and treatment for physicians-to be. It was recognized that rosacea is under-reported and undiagnosed in patients of color. Another study showed a staggering report of only 2% of patients who were black, 2.3% were Asian, and 3.9% were reported to have diagnosed rosacea when a survey on the racial/ethnic distribution of patients was done by the US National Ambulatory Medical Care Survey from 1993 to 2010.[9] It is noteworthy to state that rosacea is reported to have a prevalence rate of up to 10% and 40 million cases worldwide, even when it is prevalently reported in fair-skinned people from Celtic and North European Heritage, leading to the perception that people of color do not experience it.[3,10-12]
This study is on a volunteer basis, with questions asked on an online survey through Google Forms. Overall, clinical students, who made up 37% of the sample, displayed the highest correct answers in the survey. Preclinical, made up of 62.7% of the sample, had an evident decrease in the overall understanding and awareness of rosacea.
Out of all the questions in the survey, most of the sample understood the correct definition of rosacea, while a notable amount of 16.3% simply did not know, and a small minority had a misunderstanding as to what it was. Lack of awareness of the differentiation of other skin manifestations such as acne and dermatitis is a reason; however, this is minutely seen as there is a generalized understanding of rosacea noted. For the types of rosacea noted, 53.5% noted there was none, while an increased awareness was noted for papulopustular, and a decreased manifestation was ocular and phymatous.
On analysis, 65.1% correctly recognized the symptoms to be the flushing and redness in the center of the face, swollen skin, dry skin, and acne-like breakouts with itchy eyes. About 16.3% could not recognize, and 18.6% were not aware of the symptoms. There is a lack of awareness for identifying the signs of severity, with only 26.7% recognizing “Rhinophyma and Papulopustules” to be the correct answer, and a shocking 39.5% not knowing how to differentiate.
When it came to understanding the risk factors such as diet and genetics, 46.5% did not know of a genetic link, while 23.3% correctly recognized there to be a link. The identification of a striking familial inheritance pattern for rosacea validates the presence of a genetic component in the etiopathogenesis of the condition.[13]
We do need to recognize the impact of non-genetic factors such as the environment and diet to contribute to the occurrence of rosacea. Ultraviolet radiation from the sun is known to damage skin cells. Studies also contribute to the fact that an overgrowth of Demodex folliculorum may cause the development of rosacea as it stimulates an abnormal immune response, disrupting the normal skin barriers. Many dietary trigger factors for rosacea have been stated, including hot beverages, spicy foods, caffeine, and so on, as a result in the case of heat, there is direct vasodilation, which activates the transient receptor potential vanilloid member 1 cation channels that are linked to flushing, stinging sensation, and sensitive skin.[14] From our study, 34.9% are not aware of any association of dietary risk, while 25.6% did correctly recognize it.
Overall, a general understanding and awareness is that topical treatments are the most preferred management method, as the sample displayed 58.1% for it, while a minority of 18.6% did not know. About 10.5% did opt for medications rather than topical treatments. With which type of topical medications, the majority of the sample, a staggering 50% did not know, while 7% correctly answered brimonidine to be the right treatment with over 40.7% being incorrectly guided. On a positive note, 45.3% did correctly recognize that treatment is given until the symptoms disappear, while disappointingly, 38.4% did not know.
With regard to differential diagnosis, rosacea can be mistaken for acne vulgaris, dermatitis, lupus, and folliculitis, as noted by 33.7% of our sample. While a minority of 19.8% preferred dermatitis to be more concerning rosacea than just acne vulgaris, and just folliculitis and lupus. The majority of 29.1% did not know. Recognizing the psychosocial implications of rosacea and increased chances of misdiagnosis is pivotal. An NRS survey done in 2012 of 801 patients noted a negative social impact.[15]
For similarities, most of the sample could define rosacea, but for the types, the clinical group was 5.5 times more correct. The clinical group displayed 1.9 more times to recognize the common symptoms than preclinical, with awareness of the signs of severity 3.6 times than preclinical. There are similarities between the awareness of genetic linkages between both parties; however, the clinical sample could recognize that there is a dietary link, 2.9 more times than the preclinical group. For the management of rosacea, clinicians could correctly recognize the best management 1.8 more times and topical medication 3.25 more times than the preclinical group. However, for the duration of the treatment plans, the preclinical group could correctly recognize 17% more than the clinical, and the same was noted in recognizing the triggering factors, with the preclinical group recognizing 50% more. For understanding differential diagnostics, both the preclinical and clinical groups could recognize correctly, with clinical recognizing 18.4% times more; the same applies to recognizing high-risk groups, and gender affected as well. Clinicians could recognize the age group more affected 2.5 times more and have found more patients with rosacea, minutely with 10% more than preclinical. The clinical group noted the recognition of more remission cases than the preclinical group, 2.7 more times.
Overall, most of the sample has not seen a rosacea patient with 65.1% stating, while 27.9% have seen <3 patients. Factors such as a lack of rheumatology, or dermatology clerkships, or rotations can play a part. The exploration of where a patient was seen was not identified. The lack of patient encounters and exposure to rosacea contributes to the lack of awareness and the increased chances of misdiagnosis. For remission cases, a shocking 80.2% simply did not know, while 15.1% correctly did note the awareness of remission cases. After a patient achieves therapeutic success, according to Schaller et al., clinicians should take proactive steps to maintain remission and stave off relapse for as long as they can. Research indicates that administering treatment for up to 52 weeks can decrease the relapse rate and raise the percentage of patients who achieve near-complete or near-complete clearance.[16]
The sample size recorded from the online survey was only 86 responses, which is one of the major limitations to comprehending this study on a broader population. Since the study was limited to only international medical students, this could potentially lead to selection bias and gender-based bias, as most of the participants were females. Some participants needed to gain knowledge or were uncertain about certain questions, which could introduce the potential for response bias and affect the accuracy of the information collected.
Understanding basic concepts and treatment methods of rosacea can positively contribute to medical students’ approach to patient care by knowing precise clinical presentations, enhancing diagnostic skills, and applying effective evidence-based medical interventions.
It is also important to stay updated and bridge gaps in knowledge through the latest research studies and treatment options. By gathering information about risk factors, medical students can contribute to prompt diagnosis, prevention and psychosocial impact, and improving patients’ quality of life.
Firstly, by incorporating dermatology modules into the curriculum, medical students can gather theoretical knowledge effectively. Integrations of practical training, especially during clinical rotations in respective departments, can improve clinical skills and ensure apt exposure to patients affected by rosacea.
In summary, the study highlights varied awareness levels of rosacea among international medical students. Disparities between preclinical and clinical students suggest the influence of clinical exposure on knowledge levels. Despite valuable insights, study limitations, such as small sample size and potential biases, should be noted. Addressing these gaps in medical education is crucial for enhancing the preparedness of future health-care professionals to manage rosacea effectively.
CONCLUSION
This cross-sectional study assessed the level of awareness of rosacea amongst medical students at Tbilisi State Medical University, Georgia. No prior study was found, similar to this study, where this study was conducted. The findings of this study showed that medical students were not well aware of certain information on rosacea, particularly for treatment options and remission cases. However, based on comparisons between medical students in their clinical and preclinical years, it was seen that clinical-year students had a more comprehensive awareness of rosacea than those in their pre-clinical years, which highlights how crucial it is to expose students to patients to modify their perception of what is understood. The gap in knowledge can be overcome by incorporating case-based seminars and workshops to integrate preclinical knowledge with different stages of the disease and its management options. The understanding and prognosis of this condition would be greatly improved by increasing public awareness of the different varieties of rosacea, risk factors, and particularly treatment choices and lifestyle changes.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- An update on the treatment of rosacea. Aust Prescr. 2018;41:20-4.
- [CrossRef] [PubMed] [Google Scholar]
- Microbiota in rosacea. Am J Clin Dermatol. 2020;21(Suppl 1):25-35.
- [CrossRef] [PubMed] [Google Scholar]
- Applying the phenotype approach for rosacea to practice and research. Br J Dermatol. 2018;179:741-6.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence-based update on rosacea comorbidities and their common physiologic pathways. J Am Acad Dermatol. 2018;78:156-66.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial aspects of rosacea with a focus on anxiety and depression. Clin Cosmet Invest Dermatol. 2018;11:103-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea understanding among Korean patients: A multi-center questionnaire study. Dermatol Sin. 2023;41:214.
- [CrossRef] [Google Scholar]
- Clinical clues to identify patients with ocular rosacea-a Germany-wide epidemiologic analysis. Int J Dermatol. 2022;61:880-5.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances in understanding and managing rosacea. F1000Research. 2018;7:1885.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences of rosacea and its treatment: An interpretative phenomenological analysis. Br J Dermatol. 2018;178:154-60.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea in skin of color: Not a rare diagnosis. Dermatol Online J. 2014;20:13030/qt1mv9r0ss.
- [CrossRef] [Google Scholar]
- Rosacea: New features for better care. Ann Dermatol Venereol. 2017;144:508-17.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of rosacea in the general population of Germany and Russia-The RISE study. J Eur Acad Dermatol Venereol. 2016;30:428-34.
- [CrossRef] [PubMed] [Google Scholar]
- Ethnicity versus climate: The impacts of genetics and environment on rosacea epidemiology and pathogenesis. Clin Exp Dermatol. 2020;2:109.
- [Google Scholar]
- Rosacea pathogenesis, common triggers, and dietary role: The cause, the trigger, and the positive effects of different foods. Clin Dermatol. 2021;40:122-7.
- [CrossRef] [PubMed] [Google Scholar]
- Topical metronidazole maintains remissions of rosacea. Arch Dermatol. 1998;134:679-83.
- [CrossRef] [PubMed] [Google Scholar]
- How to optimize rosacea treatment for better patient outcomes: An opinion piece. J Clin Aesthet Dermatol. 2022;15:E60-2.
- [Google Scholar]







