Translate this page into:
Precision and efficiency unveiled: Optimizing suction blister formation through syringe edge refinement and height reduction

*Corresponding author: Akshay Arun Vetal, Department of Dermatology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India. akkiii5858@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dhurat RS, Vetal AA, Chamle SM, Ranka A. Precision and efficiency unveiled: Optimizing suction blister formation through syringe edge refinement and height reduction. CosmoDerma. 2024;4:115. doi: 10.25259/CSDM_124_2024
PROBLEM
Suction blister-based epidermal grafting involves the induction of subepidermal suction blisters in the donor area by prolonged application of vacuum, with the subsequent transplantation of its roof to the receptor area for transplanting viable epidermis. The method is advantageous in melanocyte-bearing epidermis transplantation, ensuring both donor and recipient sites heal without scarring. However, the major disadvantages are the time required for blister formation and the limited yield of the graft.
The standard syringe design, often featuring relatively sharp-edged barrel flanges, can cause discomfort and limit skin suction effectiveness. This surgical pearl introduces a modification involving the use of a softened-edge syringe along with a shortened height, which expedites blister formation, increases graft yield, and reduces the risk of hemorrhagic complications.
SOLUTION
The standardized suction blister device was set up as per Gupta et al., containing a 5/10/20 mL disposable syringe connected to a 3-way tap with a latex rubber tube, a 50 mL syringe for air aspiration, and a manometer for measuring negative pressure [Figure 1].[1] The 20-mL syringe was halved using a precise cutting method [Figure 1]. The edges of the halved syringe were softened using sandpaper and a gentle touch of a spirit lamp to further refine and roll the edges [Video 1]. This refined syringe was then integrated into the standard suction blister procedure [Figure 2]. This led to the formation of an intact blister with clear fluid, indicating successful epidermal detachment from the dermoepidermal junction. Reducing the syringe volume by lowering its height while maintaining constant suction pressure was expected to heighten pressure within the syringe in accordance with Boyle’s law (P1V1 = P2V2).[2,3] This adjustment aims to expedite the equilibration between the syringe and the patient’s skin, potentially accelerating blister formation [Figure 3]. The softened edges reduced procedural pain and increased the effective skin suction area by approximately 44%, thereby significantly increasing graft yield [Figure 4]. In contrast to innovations introducing extra equipment, our distinct approach modified the original procedure, marrying simplicity with efficacy through syringe cut edge refinement with height reduction, which increased the graft yield and reduced the time taken for the procedure and complications associated with the procedure. Beyond procedural efficiency, these changes prioritized patient comfort. The potential impact of these modifications called for further empirical validation, presenting promising avenues for advancing suction blister procedures.
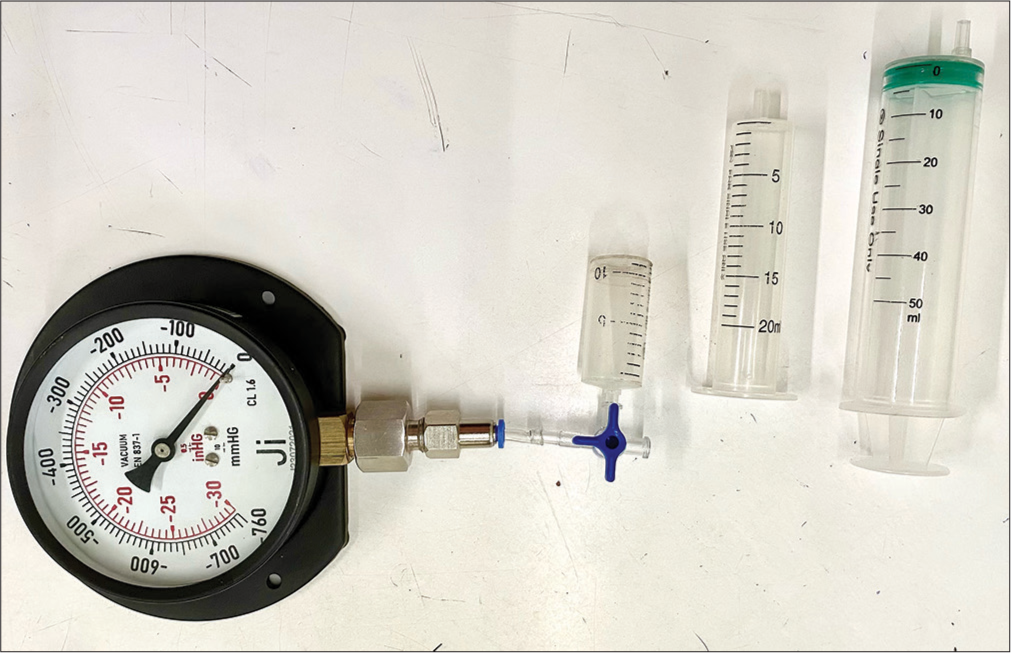
- Standardized suction blister device consisting of a 20 mL disposable syringe, modification of the 20 mL syringe by cutting it into half the size connected to a 3-way tap with a latex rubber tube, a 50 mL syringe for air aspiration, and a manometer for measuring negative pressure.
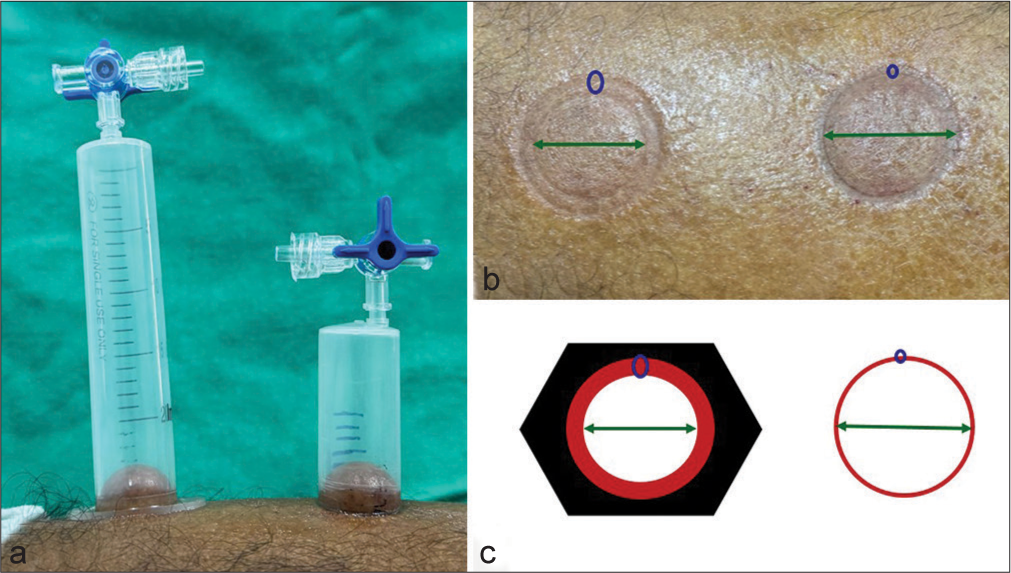
- (a) Induction of suction blister at baseline. A greater effective area for induction of blister in half cut syringe as compared to conventional syringe. (b) Half cut syringe showing 44% increase in effective area for blister induction. (c) Schematic diagram showing 44% increase in effective area for blister induction.
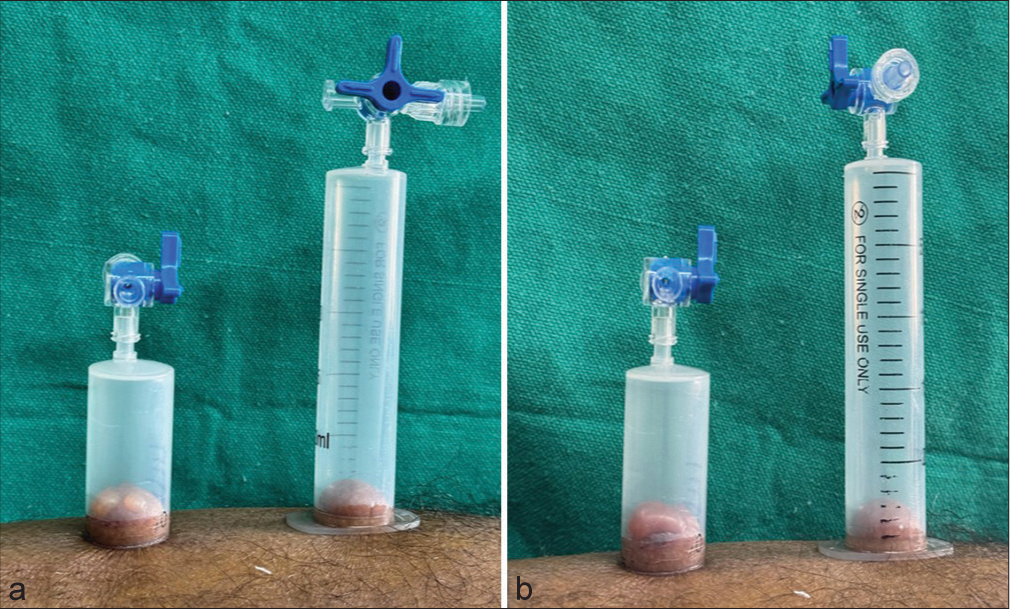
- (a) Induction of suction blister at 45 min induction of two small blisters in the half-cut syringe and absence of blister formation in conventional syringe. (b) After 1 h induction of single large blister in half cut syringe and no blister formation in conventional syringe.
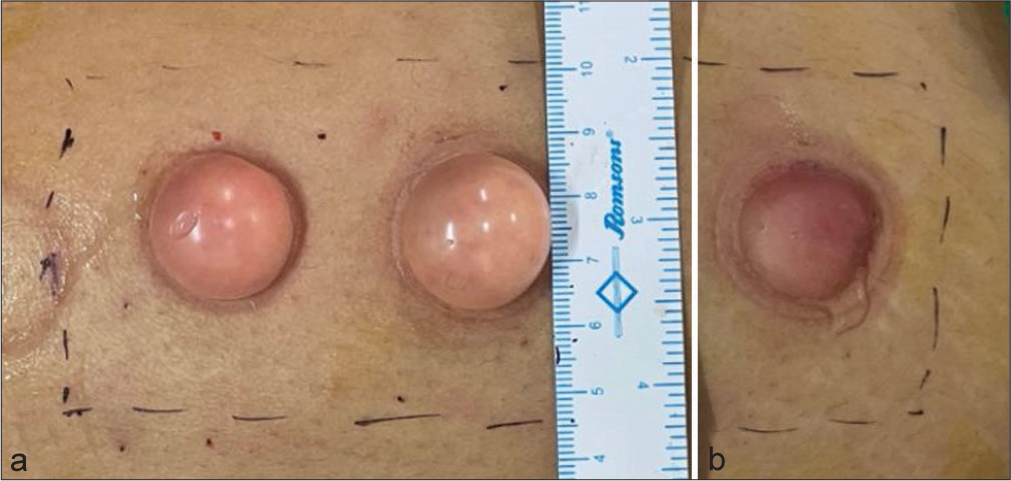
- The image depicts. (a) A well-formed intact blister with clear fluid indicating successful epidermal detachment from dermoepidermal junction free from blood tinge with enhanced graft size using smooth edged syringe. (b) A well-formed but ruptured blister with comparatively lesser graft size using standard syringe.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Video available on:
Financial support and sponsorship
Nil.
References
- Surgical pearl: Standardized suction syringe for epidermal grafting. J Am Acad Dermatol. 2005;52:348-50.
- [CrossRef] [Google Scholar]
- Surgical pearl: Suction syringe for epidermal grafting. J Am Acad Dermatol. 1997;37:638-9.
- [CrossRef] [Google Scholar]





