Translate this page into:
Phacomatosis pigmentovascularis

*Corresponding author: Arun Somasundaram, Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. arunsomasundaram25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Somasundaram A. Phacomatosis pigmentovascularis. CosmoDerma 2023;3:173. doi: 10.25259/CSDM_189_2023
A 5-year-old male child was brought by parents with complaints of skin lesions that present since birth over the face and back. The child was born of a non-consanguineous marriage with uneventful antenatal and natal history. The child was developmentally normal. Cutaneous examination revealed a port-wine stain over the face associated with mild hypertrophy of the upper lip [Figure 1a] and aberrant extensive Mongolian spots (dermal melanocytosis) over the back and leg [Figure 1b]. The child was diagnosed with phakomatosis pigmentovascularis type 2 (association of the nevus flammeus and aberrant Mongolian spots). Our child did not have any neurological or eye and skeletal concerns. Magnetic resonance imaging and magnetic resonance angiography did not reveal any abnormalities. Parents were reassured regarding the condition and were advised to follow-up later if required.
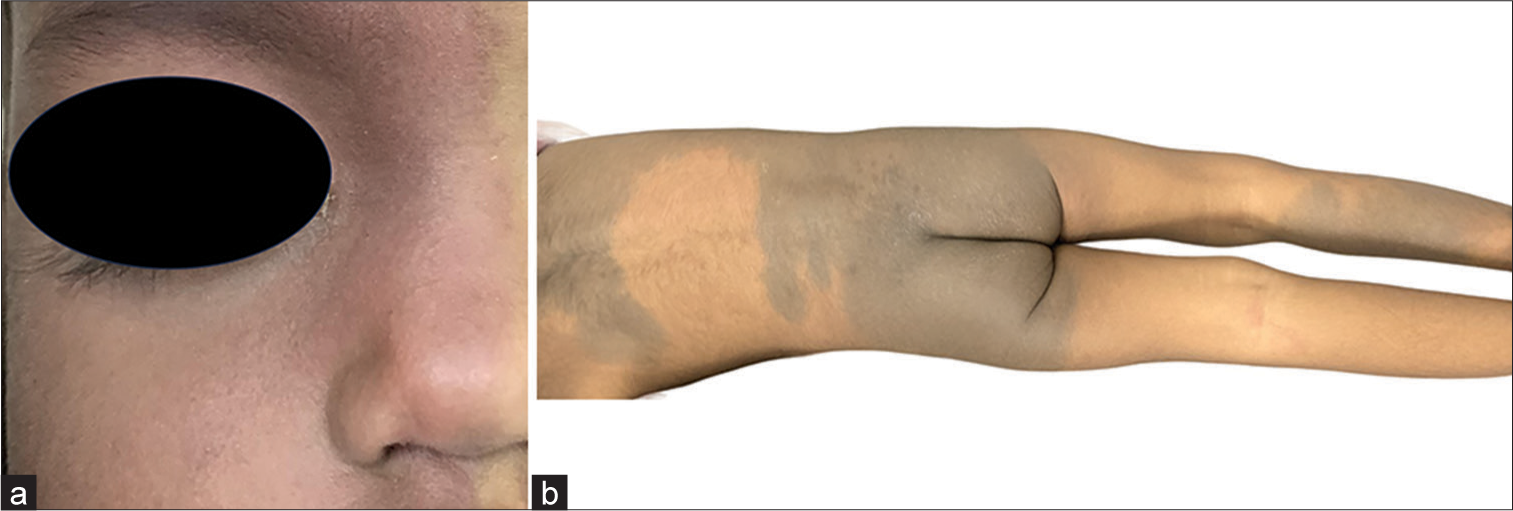
- (a) Port-wine stain over the face associated with mild hypertrophy of the upper lip. (b) Aberrant extensive Mongolian spots (dermal melanocytosis) over the back.
Phacomatosis pigmentovascularis is orchestrated by an association of a vascular nevus with an extensive pigmentary nevus. Hasegawa and Yasuhara classified into five types and each type was further subdivided according to the presence of cutaneous-only manifestations (subtype a) or if associated with systemic manifestations (subtype b), which are ocular, vascular, skeletal, and neurological. Happle classified into four groups – phacomatosis cesioflamea (nevus flammeus and aberrant Mongolian spots or blue nevus), phacomatosis spilorosea (nevus spilus and telangiectatic nevus), phacomatosis cesiomarmorata (aberrant Mongolian spots or blue nevus with cutis marmorata telangiectatica congenita), and phacomatosis pigmentovascularis of non-classifiable type.[1] Magnetic resonance imaging, magnetic resonance angiography and venography of the brain, echocardiogram, detailed eye examination, and skeletal survey are to be done if the organ system is clinically suspected to be affected. This case highlights the importance of screening for associated neurological, ocular, and skeletal abnormalities in a child with phakomatosis pigmentovascularis. Though, our child had extensive skin lesions was found to have no extracutaneous involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Phacomatosis pigmentovascularis: Report of four new cases. Indian J Dermatol Venereol Leprol. 2016;82:298-303.
- [CrossRef] [PubMed] [Google Scholar]





